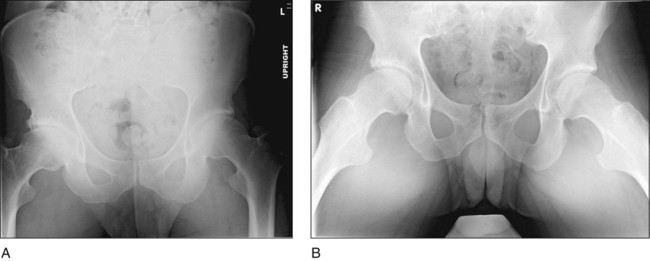
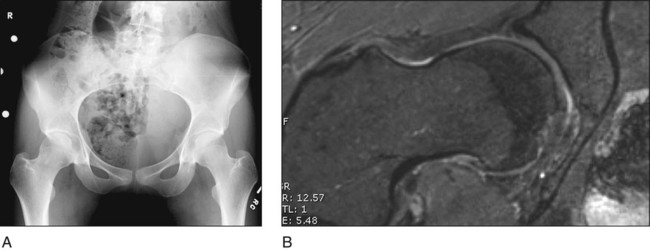
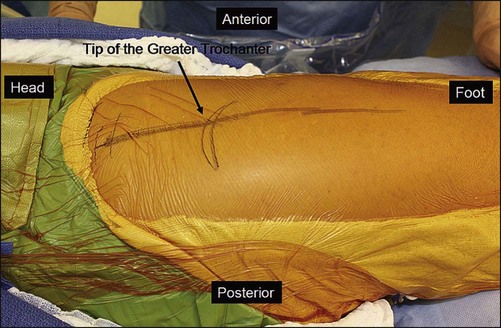
• Anteroposterior (AP) views of both hips should be obtained on a single film with the beam centered over the femoral heads. Care should be taken to ensure appropriate pelvic tilt and avoid pelvic rotation. Lateral center-edge angles can be measured to assess lateral acetabular coverage. • On false profile views of both hips, anterior coverage can be evaluated by measuring an anterior center-edge angle. • Frog-leg lateral, cross-table lateral, or modified Dunn lateral views have all been used to assess femoral head-neck offset, but many cam lesions can still be missed. • Figure 1 shows AP (Fig. 1A) and frog-leg lateral (Fig. 1B) views of the pelvis in a 28-year-old male with cam- and pincer-type femoroacetabular impingement. Note the decrease in femoral head-neck offset, the large cam deformity, and the right rim fracture caused by impingement. • diGEMRIC MRI is the best imaging study to evaluate the soft tissues of the hip, including the labrum, ligamentum teres, and extracapsular musculature. • diGEMRIC sequences are especially useful for evaluating the health of the articular cartilage and identifying chondral flaps. • Radial cuts taken circumferentially around the femoral head and neck allow better identification of subtle cam lesions. In a 20-year-old female with right hip pain, a plain AP radiograph is somewhat suggestive of a cam deformity, but the findings are subtle (Fig. 2A). Radial sequence MRI of the same hip, however, clearly shows the cam morphology (Fig. 2B). • The proximal extent of the incision is just distal to the iliac crest, and the distal end of the incision is 6–8 cm past the vastus ridge. The average incision length is 20–25 cm. • The Gibson approach starts with a straight incision centered over the anterior third of the greater trochanter (Fig. 5). • Alternatively, the cephalad limb of the incision can be curved posteriorly for the Kocher-Langenback approach.
Surgical Dislocation of the Hip
Indications
 Femoroacetabular impingement caused by (CAM) and/or pincer-type mechanisms (may be idiopathic or due to Perthes’ disease, slipped capital femoral epiphysis, etc.)
Femoroacetabular impingement caused by (CAM) and/or pincer-type mechanisms (may be idiopathic or due to Perthes’ disease, slipped capital femoral epiphysis, etc.)
 Subcapital realignment of unstable slipped epiphyses
Subcapital realignment of unstable slipped epiphyses
 Intra-articular lesions such as pigmented villonodular synovitis or synovial chondromatosis
Intra-articular lesions such as pigmented villonodular synovitis or synovial chondromatosis
 Femoral head and neck fractures
Femoral head and neck fractures
 Any other procedure requiring full exposure of the femoral head, femoral neck, or acetabulum
Any other procedure requiring full exposure of the femoral head, femoral neck, or acetabulum
Examination/Imaging
 Specific physical examination findings and imaging modalities may vary depending on the specific hip condition being treated by the surgical dislocation approach.
Specific physical examination findings and imaging modalities may vary depending on the specific hip condition being treated by the surgical dislocation approach.
 In general, examination should include a careful assessment of hip range of motion, including flexion, extension, abduction, adduction, and internal and external rotation. The latter should be tested both in extension and 90° of hip flexion.
In general, examination should include a careful assessment of hip range of motion, including flexion, extension, abduction, adduction, and internal and external rotation. The latter should be tested both in extension and 90° of hip flexion.
 Magnetic resonance imaging (MRI): diGEMRIC with radial sequences
Magnetic resonance imaging (MRI): diGEMRIC with radial sequences
Surgical Anatomy
 The main blood supply to the femoral head arises from branches of the medial femoral circumflex artery (MFCA), and preservation of this blood supply is critical to achieving safe surgical dislocation of the hip (Fig. 3).
The main blood supply to the femoral head arises from branches of the medial femoral circumflex artery (MFCA), and preservation of this blood supply is critical to achieving safe surgical dislocation of the hip (Fig. 3).
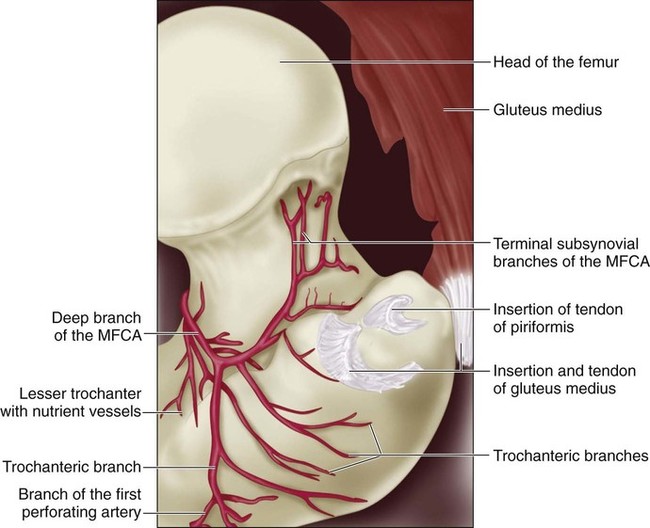
 The trochanteric branch of the MFCA does not contribute appreciably to the perfusion of the femoral head but is a constant landmark that will guide the surgeon to the level of the obturator externus.
The trochanteric branch of the MFCA does not contribute appreciably to the perfusion of the femoral head but is a constant landmark that will guide the surgeon to the level of the obturator externus.
 The deep branch of the MFCA is the largest contributor to femoral head perfusion. It crosses posterior to the obturator externus and anterior to the tendons of the superior gemellus, obturator internus, and inferior gemellus. It perforates the capsule of the hip just proximal to the insertion of the tendon of the superior gemellus and distal to the tendon of the piriformis.
The deep branch of the MFCA is the largest contributor to femoral head perfusion. It crosses posterior to the obturator externus and anterior to the tendons of the superior gemellus, obturator internus, and inferior gemellus. It perforates the capsule of the hip just proximal to the insertion of the tendon of the superior gemellus and distal to the tendon of the piriformis.
 During dislocation of the hip, this vessel is protected by the intact obturator externus muscle.
During dislocation of the hip, this vessel is protected by the intact obturator externus muscle.
Positioning
 The patient is placed in a lateral decubitus position on a radiolucent table (Jackson, Steris, etc.) using a pegboard.
The patient is placed in a lateral decubitus position on a radiolucent table (Jackson, Steris, etc.) using a pegboard.
 The ipsilateral arm is placed in a safe position using a cardiac armholder.
The ipsilateral arm is placed in a safe position using a cardiac armholder.
 A special pillow placed over the down leg to protect it also provides a good working surface on which to lay and position the operative leg (Fig. 4). Alternatively, standard pillows can be used over the down leg.
A special pillow placed over the down leg to protect it also provides a good working surface on which to lay and position the operative leg (Fig. 4). Alternatively, standard pillows can be used over the down leg.

 A plastic hip drape is used that will allow placement of the leg into a sterile bag during the anterior dislocation maneuver.
A plastic hip drape is used that will allow placement of the leg into a sterile bag during the anterior dislocation maneuver.
Portals/Exposures
 A longitudinal incision is made over the lateral aspect of the femur, centered over the anterior third of the greater trochanter.
A longitudinal incision is made over the lateral aspect of the femur, centered over the anterior third of the greater trochanter.
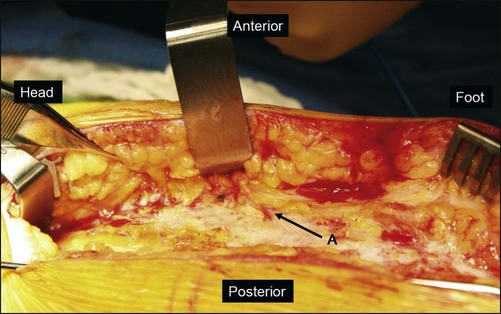
 The subcutaneous tissues are divided sharply down to the level of the iliotibial band and the fascia over the gluteus maximus muscle. The gluteus maximus should be released at its anterior edge. The anterior border of the gluteus maximus can be located by identifying the perforating branches of the inferior gluteal artery (Fig. 6, A). These blood vessels are constant and mark the anterior edge of the muscle.
The subcutaneous tissues are divided sharply down to the level of the iliotibial band and the fascia over the gluteus maximus muscle. The gluteus maximus should be released at its anterior edge. The anterior border of the gluteus maximus can be located by identifying the perforating branches of the inferior gluteal artery (Fig. 6, A). These blood vessels are constant and mark the anterior edge of the muscle.
 The fascia overlying the gluteus maximus should be preserved and the muscle can be released along its anterior edge. Distally, the fascia lata can be split in line with the femur.
The fascia overlying the gluteus maximus should be preserved and the muscle can be released along its anterior edge. Distally, the fascia lata can be split in line with the femur.![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


17: Surgical Dislocation of the Hip




