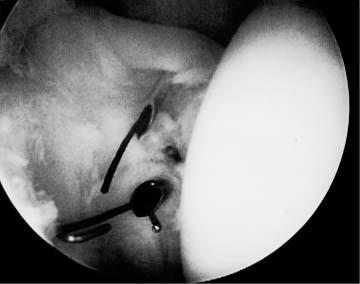
Case 16 A 23-year-old, right-hand-dominant woman who is a recreational softball player presents with a 6-month history of persistent right shoulder pain and “slipping,” occurring most often during overhead activities. She denies any frank dislocations. This patient has a full range of shoulder motion and has no tenderness about the shoulder. She has normal strength of the rotator cuff and is neurovascularly intact. However, examination demonstrates a 2+ sulcus sign on the affected side. Translation testing demonstrates symmetrically increased anterior and posterior translation of the shoulder. She also demonstrates a positive apprehension sign for pain, but not for instability. There is a positive relocation test for resolution of the pain as well. 1. Rotator cuff tendinitis 2. Anterior shoulder instability 3. Multidirectional instability 4. Rotator interval capsular lesion with symptomatic inferior instability A three-view shoulder radiographic series including an anteroposterior (AP), axillary, and scapular Y view fail to reveal any obvious abnormalities. Rotator Interval Capsular Lesion. This patient presents with a rather insidious onset of primarily inferiorly directed instability symptoms associated with overhead activities. No pathognomonic finding in the history or physical examination distinctly points toward a rotator interval capsule lesion, although the symptoms of instability, combined with the increased inferior translation on the affected side, lend support to such a possible pathologic disruption. The patient did not demonstrate any classic symptoms of anterior shoulder instability, such as a positive apprehension sign for subluxation, but clearly does have a component of multidirectional instability. These patients may demonstrate arthroscopic findings such as the classic Bankart lesion, midsubstance or humeral sided glenohumeral ligament disruptions, evidence of rotator interval capsular tearing, and/or superior and middle glenohumeral ligament disruptions. They may also demonstrate no apparent pathology at all. The only known means for confirming the diagnosis of an isolated rotator interval capsular lesion is by surgical identification during arthroscopy or at the time of arthrotomy. The role of the rotator interval capsule in shoulder instability has only recently been defined. Harryman and colleagues (1992), in a cadaveric study, have demonstrated the importance of the anterosuperior quadrant of the shoulder capsule as it relates to limiting inferior translation of the glenohumeral joint. Clinical studies by Nobuhara and Ikeda (1987), as well as a recently published study by one of the authors (L.D.F.), have demonstrated the value of rotator interval capsule plication in patients with inferior or multidirectional instability. Most patients with multidirectional instability and clinical evidence of increased inferior translations respond to an organized exercise program. However, if clinical instability persists despite such a program, operative intervention is indicated. The arthroscope has proven to be a very valuable tool not only in diagnosing but also in treating many patients with increased inferior translations. The authors perform arthroscopy on every patient undergoing shoulder instability surgery because of its value in accurately assessing intraarticular pathologic disruptions. Typically, patients with inferior instability secondary to disruption of the rotator interval capsule do not have any other identifiable intraarticular pathology. No Bankart lesions or humeral avulsions of the glenohumeral ligament are seen. Careful evaluation of the rotator interval capsule, however, will often demonstrate laxity or frank tearing of the capsular tissue. Scar formation and fibrosis is often seen as well. The indications for arthroscopic rotator interval plication include a degree of multidirectional instability in patients who have shown no improvement with an extensive nonoperative treatment program. Patients with high degrees of inferior instability (examinations that demonstrate more than a 2+ sulcus sign) are not good candidates for isolated arthroscopic rotator interval plication. However, they may benefit from an arthroscopic rotator interval plication performed to supplement other stabilization procedures. In fact, arthroscopic rotator interval plication has proven to be a valuable supplement to other arthroscopic stabilizations. This is especially true when an element of increased inferior translations is present, or when arthroscopic evaluation demonstrates patulous, thin, or poorly defined glenohumeral ligamentous tissue. Arthroscopic rotator interval plication can be easily accomplished with the patient in either the lateral decubitus or beach chair position. With a standard posterior portal the rotator interval is carefully visualized and assessed for laxity, either within the interval tissue itself or in the area of the superior glenohumeral ligament. Significant inferior laxity in the glenohumeral joint capsule is important to identify in the absence of a Bankart lesion or other obvious pathologic soft tissue injury. Following the completion of a thorough diagnostic arthroscopy, an anterior instrument portal is established using an outside-in technique. This anterior portal is placed inferiorly within the rotator interval capsule adjacent to the subscapularis tendon. Care is taken to avoid injury to either the superior or middle glenohumeral ligament. If there is anterior labral and/or inferior capsuloligamentous damage, requiring arthroscopic repair or reconstruction, then this portion of the procedure should be carried out first. Once the arthroscopic stabilization procedure has been completed, attention is turned to the rotator interval capsule. The rotator interval capsule may be plicated arthroscopically by using several methods. With one technique, the arthroscope is used to visualize the rotator interval through the posterior portal. An arthroscopic suture transporter or suture retriever is inserted anteriorly through the capsule adjacent to the subscapularis tendon. A small portion of the superior border of the subscapularis may also be included in the plication. A spinal needle is then placed through the anterior superior border of the lateral corner of the rotator interval capsule adjacent to the anterior margin of the supraspinatus tendon. A no. 1 Prolene suture is then passed through the spinal needle and retrieved out the anterior portal using the transporter device (Fig. 16–1). This suture is then tagged with a hemostat, and attention is turned back to the rotator interval capsule. The transporter is again placed through the anterior cannula, piercing the capsule medial to the previously placed stitch. The superior glenohumeral ligament can also be incorporated in the plication by using the transporter to pierce it at the same time. The spinal needle is again placed in a similar fashion through the anterior margin of the supraspinatus tendon or at the border of the supraspinatus tendon and superior rotator interval capsule in a more medial position than the initially place stitch. A no. 1 Prolene suture is then placed through the spinal needle and retrieved out the anterior cannula, utilizing the transporter as before (Fig. 16–2). If necessary, a third more medially placed stitch can be placed in a similar fashion. Using this technique, two or three sutures can be placed across the rotator interval capsule. Traction on these stitches will confirm adequate plication of the rotator interval capsule under direct arthroscopic visualization. The arthroscope is then transferred into the subacromial bursa, again using the posterior portal for visualization. The anterior cannula is also repositioned into the subacromial bursa. The superior sutures are readily identified at the anterior margin of the supraspinatus tendon within the subacromial space. A crochet hook can be used to retrieve these sutures out the anterior cannula. Standard arthroscopic knot-tying techniques are utilized to tighten the sutures independently. Following completion of the knot tying, the arthroscope can be repositioned into the glenohumeral joint through the posterior portal. Visualization of the rotator interval capsule intraarticularly will confirm adequate plication. Figure 16–1. Initiation of intraarticular rotator interval repair. Note the suture transport device through the subscapularis tendon and middle glenohumeral ligament, and the spinal needle through the anterior margin of the supraspinatus tendon and adjacent capsule. A no. 1 Prolene suture is being advanced through the spinal needle. (See Color Plate 16–1.) A second method designed by the authors for plicating the rotator interval capsule can be performed exclusively on the bursal side of the rotator cuff within the subacromial space. Following glenohumeral joint arthroscopy, the arthroscope is transferred into the subacromial space. While visualizing from the posterior portal, a complete bursectomy is accomplished utilizing standard arthroscopic instruments. This allows for excellent visualization of the rotator interval capsule. A standard, curved Caspari suture punch device is then loaded with 0 Prolene suture and introduced into the bursa through the lateral portal. The patient’s arm is then slightly externally rotated, so as to improve visualization of the rotator interval capsule. A single bite of the most superior aspect of the subscapularis tendon and adjacent rotator interval capsule is taken. The suture punch is then opened, but this tissue is left engaged on the Caspari suture punch needle. While this tissue is engaged, the patient’s arm is slightly internally rotated, bringing the anterior margin of the supraspinatus tendon and superior border of the rotator interval capsule into the open jaw of the suture punch. Piercing this superior tissue prior to closure and passage of the suture creates a second, more superiorly located bite of tissue in the rotator interval capsule. This double-bite technique serves to plicate the rotator interval capsule. The suture is then threaded within the bursa and removed out the lateral portal. The arthroscope can then be transferred to the glenohumeral joint. Adequate plication can be confirmed arthroscopically prior to knot tying by simply pulling traction on these sutures. Arthroscopic knot tying is then performed in the subacromial space. Using this second technique, each of these steps can be repeated, thereby placing several sutures across the rotator interval capsule. Each suture tightens the rotator interval capsule and facilitates placement of subsequent stitches in a more medial position. Translation testing following arthroscopic plication confirms enhanced stability. • It is sometimes helpful to perform an arthroscopic bursectomy in the subacromial space prior to suture placement in the rotator interval capsule. Performing a bursectomy makes subacromial suture identification and retrieval much easier. • Using the arthroscopic rotator interval plication procedure as a supplement to other arthroscopic stabilization procedures can effectively improve postoperative stability.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree