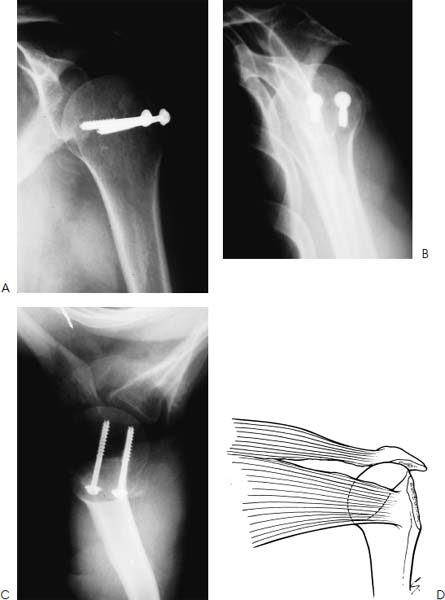
Case 1 A 24-year-old man presents several hours after a fall onto his right shoulder at work. He complains of pain and swelling of the shoulder, along with crepitation to range of motion. He denies any numbness in his right upper extremity and no neck injury. Range of motion is limited to 30 degrees of forward flexion passively and actively because of severe pain. His external rotation and internal rotation are limited as well. Crepitation can be palpated through a range of motion. There is moderate ecchymosis about the shoulder region and tenderness to palpation. Also, a small superficial abrasion is present along the anterior deltoid. Neurovascular function is normal, including axillary nerve function based on sensory testing and isometric deltoid muscle contraction. Figure 1–1. An anteroposterior (AP) (A), scapular Y (B), and axillary (C) view of the shoulder. 1. Shoulder dislocation 2. Proximal humerus fracture 3. Scapular fracture 4. Rotator cuff contusion Radiographs of the shoulder are obtained (Fig. 1–1). Displaced Greater Tuberosity Fracture. Radiographs confirm the diagnosis of a displaced greater tuberosity fracture. One important consideration in the accurate diagnosis of this injury is the axillary view or a scapular Y view, which will demonstrate a shoulder dislocation if present. The great majority of fractures of the proximal humerus present acutely, with the most common symptoms being pain, swelling, and tenderness about the shoulder. Palpation of the bony landmarks is often difficult secondary to swelling. Crepitus is usually present through a range of motion if the fracture fragments are displaced. Ecchymosis usually occurs and can be seen in the arm, forearm, and hand as well as along the chest wall. Patients should be informed of this possibility so as to help avoid undue concern. On presentation, patients find it difficult or impossible to initiate active motion, particularly in forward flexion, and the arm is usually held close to the chest wall. Figure 1–2. Postoperative AP (A), scapular Y (B), and axillary (C) radiographs following screw and supplemental suture fixation of this displaced greater tuberosity fracture. (D) An illustration of a displaced greater tuberosity fracture fragment demonstrating a longitudinal tear in the rotator cuff that permits such displacement. A detailed neurovascular examination is essential in managing all fractures of the proximal humerus. The axillary artery and brachial plexus are in close proximity to the fracture, and injuries to these structures are not uncommon. A careful neurovascular examination including the palpation of distal pulses, the assessment of capillary refill, and a thorough neurologic examination are important. Particular attention should be paid to the axillary nerve as injury occurs quite commonly. Fortunately, this nerve injury usually resolves completely, but failure to identify such an injury prior to surgical intervention may confuse the clinical picture postoperatively. Sensation should be tested over the axillary nerve distribution, as testing for deltoid activity or weakness may be difficult because of pain. However, palpation of the anterior, lateral, and posterior heads of the deltoid will generally demonstrate isometric contraction even in the acutely fractured shoulder. Management of greater tuberosity fractures depends to a large extent on the displacement of the greater tuberosity fracture fragment. When associated with a dislocation, reduction of the glenohumeral joint will often result in close reapproximation of the greater tuberosity fragment. However, even when minimal displacement is present on the initial radiographs, subsequent displacement of the greater tuberosity fracture fragment posteriorly and superiorly can occur because of unopposed pull of the rotator cuff musculature. Therefore, serial X-rays are important in the first 2 to 3 weeks to confirm adequate fracture fragment alignment. The greater tuberosity has three distinct facets for the insertions of the supraspinatus, infraspinatus, and teres minor. Retraction and displacement of the greater tuberosity fracture fragment is pathognomonic of a longitudinal tear in the rotator cuff (Fig. 1–2D). Displacement of this greater tuberosity fracture fragment will severely limit shoulder function because of both the retraction of the rotator cuff musculature and the impingement of the greater tuberosity fracture in the subacromial space. It is generally accepted that more than 1-cm displacement of this fracture fragment in an active patient is best treated using open reduction, fixation, and rotator cuff repair, although less than 1 cm may often be best managed surgically as well (Fig. 1–2A–C). Displacement of the greater tuberosity fracture fragment of more than 1 cm is considered pathognomonic for a rotator cuff tear as well. Routine radiographs of the shoulder may underestimate the amount of posterior displacement of the tuberosity and an axillary radiograph or computed tomography (CT) scan will more accurately demonstrate greater tuberosity position. When open reduction and internal fixation is to be carried out, the patient is placed in a beach chair position and the arm draped free. If cannulated screws or other metallic implants are possibly to be used, the patient must be placed on a frame or bed suitable for fluoroscopy or at least allow for radiographic access. The authors generally use a large beanbag, which allows for translation of the patient off the bed and thus allow free access to the shoulder using the fluoroscopic unit. • Use of a figure-of-eight nonabsorbable no. 5 suture as a supplement to screw fixation is routinely performed by the authors. This is particularly true when bone quality is poor or comminution is present. The suture is usually passed through the rotator cuff tendon itself instead of through the greater tuberosity fracture fragment. • The use of large fragment cannulated screws makes fixation of the greater tuberosity fracture much easier since the cannulated guide wires will effectively hold the fracture reduced while screws are placed. This also minimizes the number of holes drilled through the fracture fragment, decreasing the possibility of greater tuberosity fracture fragment comminution intraoperatively.
History and Physical Examination
Differential Diagnosis
Radiologic Findings
Diagnosis
Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree