Chapter 20 Whiplash
After reading this chapter you should be able to answer the following questions:
| Question 1 | How do the atypical cervical motion segments differ from the typical cervical motion segments? |
| Question 2 | Which cervical motion segments most commonly subluxate with whiplash injuries? |
| Question 3 | Which muscles are most likely to be strained when the patient is involved in a rear-end collision? |
Whiplash is not a diagnostics term but is descriptive of the mechanical action whereby the body comes to a sudden stop followed by a sudden snap of the unsupported neck and head. This chapter is focused on the ramifications of whiplash that produce subluxations in the cervical spine.
Anatomy and Kinesiology of the Cervical Spine
Typical Cervical Vertebra
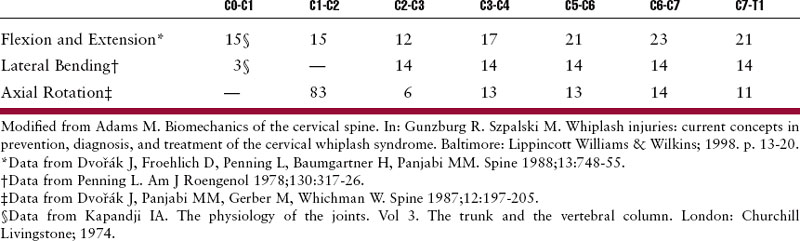
The lower cervical spine is composed of typical spinal motion segments from C2-3 to C7-T1. Each motion segment is made up of two adjacent vertebral bodies, two posterior spinal joints, the elements confined within the two lateral recesses, and the intervertebral foramina, plus all the connective and muscular tissues supporting and limiting intersegmental movement. The typical cervical vertebra is wider than it is high, with comparatively large vertebral foramina. Almost 40% of the height of the cervical spine from C2 to C7 is made up of intervertebral discs so it is not surprising that this is the most mobile region of the spine.1 Each typical motion segment contributes 20 degrees flexion-extension, 14 degrees lateral flexion, and 10 to 15 degrees side-to-side axial rotation (Table 20-1). The superior surface (superior plateau) of each vertebra is raised laterally to form the uncinate processes. These projections harbor the corresponding articular facets in the lateral inferior plateau of the vertebra above forming the uncovertebral joints (joints of Luschka).2 Like other synovial joints, they are of clinical significance because they are subject to degenerative changes. The anterior inferior surface of the body exhibits a lip that projects downward and fits together with the transversely concave superior surface of the vertebra below. This creates a “saddle” effect that limits lateral flexion and guides anteroposterior movement during flexion-extension. The pedicles project somewhat laterally as well as backward, and the laminae are angled from them in a medial direction. The spinous processes are short and frequently bifid. The articular pillars extend from the lamina-pedicle junction and support cartilage-lined facets. The superior facets are directed backward and upward, reciprocating with the inferior facets that face forward and downward.3 These oblique articular surfaces promote a high degree of coupled motion predominantly in lateral bending and rotation.
Atypical Cervical Vertebrae
The atypical vertebrae of the cervical spine are C1 (atlas), C2 (axis), and C7 (vertebra prominens). The first cervical vertebra is called the atlas because it supports the “globe-like” head. It differs significantly from all other vertebrae in that it lacks a body. Its centrum fuses with the body of the axis to form a projecting pivot (the dens) around which the atlas rotates over 80 degrees. According to Kapandji,1 flexion and extension movements of this joint involve rolling and sliding of the lateral masses similar to the movements of the femoral condyles. The curved shape of the lateral masses ensures that axial rotation is accompanied by a vertical separation of the two vertebrae, resulting in a slight helical movement rather than pure rotation. The articulations formed by the condyles of the occiput and the superior articular facets of the atlas provide for a slipping motion with a total range of flexion-extension of 15 degrees and approximately 3 degrees of lateral flexion.1
The seventh cervical vertebra is atypical in that the transverse foramina are small relative to the large transverse processes, and the vertebral arteries do not normally pass through these foramina as they do in the other lower cervical vertebrae. The vertebral arteries pass upward through the transverse foramina of the typical cervical vertebrae along the uncovertebral joints looping over the posterior arch of the atlas and continuing through the foramen magnum. They are vulnerable to injury throughout their course in the cervical area when significant trauma to the cervical spine occurs. Confusing symptoms can arise inasmuch as plexuses of postganglionic sympathetic nerve fibers surround the vertebral arteries on their back surfaces, at least from C4 to C7.4
Stability of the Cervical Spine and Whiplash injury
The wide range of motion of the cervical spine makes stability problematic.5 When the physiologic limits of cervical structures are exceeded, anatomical disruption of the soft tissues of the neck including muscles, ligaments, and joint capsules results. This combined with the “whip-like” mechanism of action creates a situation that facilitates subluxation of the cervical articulations.
Muscles of the cervical spine offer the first line of defense from whiplash injuries. Injury results when the neck musculature is unable to compensate for the rapidity of head and torso movement caused by the acceleration forces generated at the time of impact.6 When the cervical muscles contract rapidly in response to impact, the potential exists for muscle injury due to lengthening contraction.7
Structure Injured during the Four Phases of Whiplash
When a vehicle is struck from behind, the occupant’s torso is accelerated while the unrestrained head and neck lag behind.8 As the head and neck are forced into extension, the anterior cervical muscles are stretched while contracting in an effort to prevent hyperextension. Most frequently injured by this phase are the “anterior strap muscles,” including the sternocleidomastoid and scalene muscles. The splenius capitus muscles are frequently injured especially if the head and neck are rotated at the time of impact. Having the head turned at time of impact increases the risk of injury.8
Structures injured during the second phase of whiplash from a rear-end collision are those vulnerable to shear strain. Penning9 speculates that the primary mechanism of injury in whiplash is actually hypertranslation of the head backwards. He notes that it is the overstretching of the ligaments of the upper cervical spine, especially of the atlantoaxial segment (including the alar ligament), that leads to disorders of proprioceptive information. It is this phase during which translation occurs that most likely contributes to subluxation of the upper cervical articulations seen clinically. When ligaments and joint capsules are stretched, the axial traction permits the joints to separate and then subsequently compress with jamming and altered alignment. Ligamentous injury occurs when the cervical muscles become stretched to the point that the ligaments are called into play to stabilize the spine. When the ligaments become stretched, further injury to the discs and articular capsules can ensue. Disc injury usually consists of a disruption of the anulus fibrosus viewed on radiographs as a widening of the posterior disc space, a narrowing of the anterior disc space, and often a concomitant anterior hypermobile subluxation caused by disruption of the posterior elements.8(See Chapter 8.) During phase 3, acceleration is diminished with the head and torso thrown forward straining the superficial posterior cervical muscles including the upper trapezius. During phase 4, if the body is restrained by a seatbelt, the head will continue to move forward until it strikes the chest or an external object. This is the phase when the upper cervical posterior muscular and ligamentous elements of the cervical spine become injured including the suboccipital muscles. Croft8 maintains that it is the upper cervical spine that sustains the greatest injury from whiplash because it tends to be the biomechanical pivot point.
Mechanics of Whiplash
Initially, in a rear-end impact, the torso of the victim translates backward while the head and neck remain stationary and the vehicle moves forward underneath. This is followed by the abrupt upward movement of the torso as the thoracic kyphotic curvature is straightened. This sets the head into vertical acceleration that straightens and compresses the cervical spine. This is followed by a series of abnormal distortions of the neck. First there is an initial flexion of the upper cervical spine, followed by extension of the lower cervical segments. This induces an S-shaped distortion in the entire cervical spine.10–12 This is then followed by extension of all levels of the cervical spine.12 Yang and King13 also found significant posterior shear deformation present with large facet capsular stretch. They considered this to be a major source of pain. Following the extension phase, the head is cantilevered forwards into flexion with fanning of the spinous processes.
Subluxation following Whiplash
Cervical subluxation following whiplash may take the form of simple joint locking or, more likely, be accompanied by hypermobility in other motion segments. The biomechanical injuries seen clinically that result from whiplash tend to follow a characteristic pattern. The torque and lofting of the head tends to produce hypomobility and subluxation of the upper cervical and lower cervical joints with hypermobility common in the midcervical region.14 Jackson4 noted that the greatest amount of soft tissue injury occurs at the C4-5, C5-6 motion segments. Jaeger’s report15 on 11 cervicogenic headache patients related to whiplash noted that tenderness and misalignment around the transverse process of C1 was the most frequent finding. Next to upper cervical subluxations, C7-T1 and first rib subluxations are most commonly seen. Movement of spinal motion segments may be blocked anywhere in the spine with whiplash injuries,14,16,17 but most commonly seen clinically are upper cervical subluxations followed by fixation at the C7-T1 spinal motion segment, and first costovertebral articulation.14
Clinical Considerations
History
It is important to obtain as much information as possible about the whiplash injury. The direction of force, position, relationship of the head and spine, and state of tension of the neck muscles all help to determine the location of stress. The position of the patient at the time of impact should be noted. Typical questions asked of whiplash-injured patients are included in Box 20-1. These questions aid in the assessment of the severity of injury, in addition to indicating which structures are involved.
• Was the patient looking straight ahead or positioned with the head or body turned? Was the patient driving?
• Did the head or another body part strike something? Did something loose in the vehicle strike the patient?
• Was the patient wearing a seat restraint (lap type or combined lap-shoulder harness), and what was the nature of the head support?
• Was there loss of consciousness or mental confusion? Was the patient thrown from the car?
• What were the relative sizes of the involved vehicles, make of the vehicles, and type of suspension in the injured party’s vehicle?
• What was the approximate speed involved? Was the patient’s foot down hard on the brake pedal or floorboard?
• Was the seat torn loose? Did the backrest break away? Had there been a previous or old neck injury?14
The patient with whiplash most commonly gives a history of minor to moderately severe rear-end collision.18 Other types of vehicular crashes such as a head-on or side collision or a history of a fall can produce a whiplash mechanism. A sideways fall on the outstretched arm can produce a lateral whiplash effect on the cervical spine similar to the side impact vehicular collision. A blow such as from a swinging object4 may also produce whiplash. A severe form of whiplash-induced injury occurs with the “shaken baby syndrome” or “whiplash–shaken infant syndrome.” Injury occurs when an adult shakes an infant repeatedly in the fore and aft direction. This mechanism can cause severe injuries and can even be fatal.8
Symptoms of Whiplash Injury
Patients suffering from whiplash injuries complain of a large variety of symptoms typically more broad than other neck injuries. Frequently they are not aware of significant injury immediately following the accident, but after a few minutes they can develop a feeling of discomfort in the neck, associated with some degree of nausea.19 This is typically followed by a feeling of tightness and stiffness. After several days a broad symptom complex may develop.18 It is wise to inform the whiplash patient who is treated immediately following a whiplash injury that he or she may gradually feel worse for several days to prevent the perception that the treatment has made the condition worse. After 72 hours, a gradual decrease in symptoms can be expected. The delay in symptoms is thought to be due to the time required for traumatic edema and hemorrhage to occur in injured soft tissues.20
Neck pain with limited motion is the most common complaint following whiplash injury. Neck pain may occur at the back, front, and sides of the neck.4 The pain may radiate into the shoulders and arms to the fingers. The radiation may be unilateral or bilateral. Chest and back pain may also be present. The character of pain may be described as burning, sharp, throbbing, or stabbing, or as a dull ache. A deep, aching, or dull pain is common with joint lesions. Nerve irritation produces a stabbing or lightning-like pain that radiates in specific patterns. A sharp, localized pain may indicate a fracture. Throbbing pain is indicative of vascular involvement.8
Headaches are a frequent complaint with cervical spine disorders. (See Chapter 19.) The pain may be at the back of the head, the top of the head, or in the temple area.4 It may be unilateral or bilateral, intermittent or constant, localized or generalized. Muscle contraction headaches are generally associated with occipital pain, or pain radiating to the frontal area. Often referred to as tension headaches, they may be caused by spasm, injury, or inflammation to the muscles or myofascial connection to the cranial periosteum. The greater and lesser occipital nerves may be irritated by the clinically contracted muscle or by irritating substances (bradykinins, proteolytic enzymes, etc.) that accompany inflammation. Ischemia that can accompany chronic muscle spasm frequently activates a reflex whereby the pain-spasm-pain cycle becomes chronic. Vascular headaches may occur in patients with head injuries, but they represent a small fraction of those patients suffering from posttraumatic headaches as a result of whiplash. A common source of postwhiplash head pain is subluxation (jamming) of the zygapophyseal joints referred to as a cervicogenic (vertebrogenic) headache. (See Chapter 19.) Technically all headaches arising from the neck including those caused by the cervical muscles are cervicogenic in nature, and much confusion surrounding the classification of headache remains. An accurate palpatory diagnosis can determine if the cervical motion segments are involved.
Stiffness following injury usually limits motion in the direction opposite that of the muscle spasm. Weakness of the muscles of the neck, arms, and hands may be noted by the patient, and the patient often complains of difficulty balancing the head or the neck because of weakness of the neck muscles.4 Complaints of loss of grip strength and things slipping from the hands are common. Sensory complaints include numbness and tingling, frequently without actual demonstrable hypesthesia or sensory changes. Numbness of the neck, shoulders, arm, forearm, and fingers may be the result of nerve root irritation or compression, circulatory embarrassment, or referral from trigger points in the strained muscles.6 Visual disturbances are frequent following trauma to the neck. Blurred vision is a common complaint and usually of short duration. It may be due to damage to the vertebral arteries or may reflect damage to the cervical sympathetic chain.21,22 Other visual complaints can include “eye strain,” fatigue, diplopia, and photophobia.4
Occasionally symptoms of irritation of the sympathetic nerve supply in the neck occur. This can produce dilation of one pupil with irritation of the sympathetic fibers surrounding the internal carotid arteries and their branches to the eye. Horner’s syndrome is occasionally seen due to sympathetic ganglion damage around the sixth cervical level.22 Complaints of instability or dysequilibrium with a tendency to list to one side have been reported.4 Disruption of the proprioceptive system from injury to muscles and joints of the cervical spine or vasospasm or vasodilation with edema affecting labyrinth function may result in dizziness, unsteadiness, or lightheadedness.22 Dysphagia (complaints of difficulty in swallowing) and other laryngeal disturbances, with compulsive clearing of the throat,23 may be the result of swelling of the anterior neck structures or to retropharyngeal hematoma. The latter can be seen on routine lateral radiographs as forward displacement of the air shadow of the pharynx.22
Less common complaints include dyspnea or shortness of breath that may be the result of pain in respiratory muscles. Heart palpitations (tachycardia) from irritation of the fourth nerve root or irritation of the cardiac sympathetic supply should be investigated thoroughly. Vertebrobasilar arterial insufficiency can precipitate drop attacks or black out sensations. Nausea and vomiting, and complaints of irritability, insomnia, and lightheadedness may also be noted. Low back pain is frequently reported in cases of moderate to severe injury resulting from rear-end collisions, and occasionally a patient complains of leg symptoms. Sprain of the lumbar region may occur from acute flexion of the low back at the time of the accident.22 It is frequently overlooked initially because of the more severe cervical complaints at the onset.
Grieve17 stresses the vulnerability of the whiplash victim to rough handling. He describes this as a highly reactive “brittleness” during the early stages. He notes that this is quite different from the irritability of a single peripheral joint. He states,
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree