Chapter 6 The Role of Radiography in Evaluating Subluxation
After reading this chapter you should be able to answer the following questions:
| Question 1 | What are the common clinical indications for obtaining radiographs? |
| Question 2 | What are the clinical findings that indicate functional radiography may be useful? |
| Question 3 | What are the clinical indications for full-spine radiography? |
The role of radiography in the evaluation of the chiropractic spinal vertebral subluxation has evolved considerably over the years.1,2 Both static and functional radiographs are used in chiropractic to evaluate posture and biomechanics. In clinical practice, emphasis on one method or the other appears to depend largely on the individual practitioner’s concept of a subluxation. Although some chiropractors view subluxation as a purely static phenomenon of vertebral misalignment, more recently an increasing number of chiropractors have begun to view the subluxation as a more dynamic, functional concept encompassing abnormalities of articular motion.3–5
Chiropractors use radiography for several reasons. Sherman6 identifies the following clinical reasons for taking radiographs:
1. To establish a clinical (pathologic) diagnosis
2. To evaluate biomechanics and posture
4. To screen for contraindications
Nonclinical reasons for taking radiographs are inappropriate and include the following6,7:
Current epidemiologic studies examining the role of lumbar spine radiography question the value of taking radiographs for many clinical situations. Howard and Rowe8 and Deyo and Diehl9 recommend several criteria for selecting low-back pain patients for radiography (Box 6-1).
BOX 6-1 Spine Radiography: Clinical Indications for Patient Selection
Patient history
Physical findings
Adapted from Deyo RA, Diehl AK. J Gen Intern Med 1986;1:20-5; and Howard BA, Rowe LJ. Spinal x-rays. In: Haldeman S, editor. Principles and practice of chiropractic. 2nd ed. East Norwalk, CT: Appleton and Lange; 1992. p. 361-4.
Some chiropractors argue that these recommendations ignore factors unique to the chiropractic approach to patient care.6,10 For instance, Gatterman11 identifies 31 conditions that contraindicate or require modification of spinal manipulation and suggests that in at least 20 of those conditions radiographic examination is part of the standard of practice for establishing the diagnosis. The fact remains that radiography should never be used as a general screening procedure without specific clinical indication.9,12 Howe13 stresses that routine or stereotyped methods of radiographic examination do not serve the best interests of the patient.
Static Radiography and Spinographic Analysis
Spinography, the procedure of analyzing spine radiographs for postural and structural abnormalities, dates from 1910 when it was first introduced at Palmer School of Chiropractic by Dr. B.J. Palmer.1 Marking radiographs to identify misalignments was a natural extension of the popular static concept of subluxation in the early 1900s. From 1918 until 1936, full-spine radiographic techniques were developed.1,2,14 Texts on chiropractic spinography have been published by Thompson,15 Hildebrandt,16 and Winterstein.17 In addition, technique systems using spinographic analysis have been developed by several chiropractors, including Clarence C. Gonstead10,18 and Hugh B. Logan.14,19
The utility of many spinographic methods requires more study. One fundamental criticism of measuring misalignments on radiographs is the problem of anatomic asymmetry. Asymmetric developmental anomalies are common and can simulate true misalignments.20 The role of full-spine radiographs in chiropractic analysis remains controversial.2 Opinions held by chiropractors vary widely and include those who consider full-spine radiography a routine procedure and those who consider it an overused procedure that never should be used. The literature suggests, however, that with proper patient selection, careful attention to technical detail, and use of several technologic advancements, full-spine radiography is a diagnostic and analytic procedure with an acceptable risk/benefit ratio.2 The circumstances in which full-spine radiographs might be preferred over sectional radiographs are as follows: (1) cases in which clinical examination discloses the need for radiography of several spinal sections; (2) cases in which severe postural distortion is evident; (3) for scoliosis evaluation after clinical assessment; (4) cases in which a mechanical problem in one spinal area adversely affects other spinal regions; (5) to specifically evaluate complex biomechanical or postural disorders of the spine and pelvis under weight-bearing conditions.2,16,21,22
Many chiropractors agree that full-spine radiography should be reserved for evaluating scoliosis after a thorough clinical evaluation. Scoliosis measurement using the Cobb method is well established (Figure 6-1). This measurement is reported to be accurate to within 2.8 to 11 degrees.23–25 Mehta concluded that rotation of up to 15 degrees is necessary for clear-cut identification of vertebral rotation on scoliosis radiographs.26 This observation calls into question many of the methods used to measure millimetric changes in vertebral rotation. A high correlation has been demonstrated between Cobb’s angles measured on posteroanterior (PA) and anteroposterior (AP) radiographs.27
Conflicting evidence regarding the reliability of pelvic spinographic analysis has been reported. Plaugher and Hendricks28 found excellent interobserver and intraobserver reliability, and Phillips29 found very little consistency between the various methods used. Many errors arise from faulty patient positioning.30
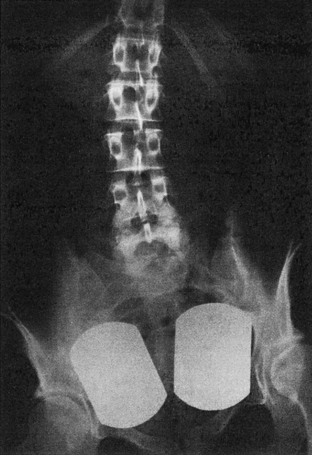
Leg length inequality (LLI) can be measured reliably from spine radiographs,31 but most authors agree that specialized orthoradiography or clinical examination is more accurate in the assessment of LLI (Figure 6-2).31–34
Some chiropractic analytical procedures are based on the premise that static misalignments can be confirmed by radiography and that these misalignments can be corrected by chiropractic adjustments. In one large study,35 the only demonstrable postmanipulation change was a 34% reduction in retrolisthesis. No posttreatment change was observed in cervical lordosis, sacral base angle, lumbar lordosis, scapular angle, or Cobb’s angle.
This study35 raises the question of the clinical validity of spinographic analysis. Phillips et al.36 concluded that spine radiographs, analyzed by measurements, have minimal value in predicting the presence or absence of low-back pain complaints. Mootz and Meeker37 and Phillips agree that the use of radiography for biomechanical (postural) evaluation requires further clarification and research. Evidence is lacking that these parameters demonstrate any clinical significance.
Owens’s review of the literature and summary of the role of line drawing analyses of static cervical radiographs used in chiropractic38 is consistent with those of Phillips et al.36 and Mootz and Meeker.37 Owens concludes that, although some studies demonstrate reliability of some of these procedures, the accuracy and clinic significance remain in question:
The major question should no longer be if x-ray analysis can be used as a tool in the scientific investigation of chiropractic subluxation. Rather, studies should be designed, using x-ray analysis, to test the fundamental hypothesis of the analysis techniques, that static structural misalignment in the neck and occiput can be a causative factor in the chiropractic subluxation.38
In his review, Owens lists 15 named chiropractic radiographic analysis techniques that are “systems” taught primarily through entrepreneurial postgraduate weekend seminars. Of the 15 techniques, only two (Gonstead and upper cervical specific-hole in one [HIO]) are taught as part of the curriculum at more than one accredited chiropractic college.38
In addition to the many “systems approaches” to marking radiographs, several lines and angles of measurement have been developed in the fields of radiology and chiropractic for assessing static and functional radiographs.39,40 Table 6-1 outlines some of the more common procedures and their clinical significance, and Box 6-2 lists the classification for intersegmental subluxations that sometimes can be seen on static and functional radiographs (Figure 6-3).41 Figures 6-4 to 6-10 illustrate some of the more commonly used lines, angles, and measurements. It should be emphasized, however, that the clinical significance of static misalignment subluxations has never been clearly established. Many of the patterns listed in Box 6-2 actually only occur as a result of articular derangements, such as severe inflammatory or degenerative disc and apophyseal joint disease, or long-standing developmental articular changes.
Table 6-1 Commonly Used Radiographic Lines, Angles, and Measurements
| Line, angle, measurement | Figure | Proposed clinical significance |
|---|---|---|
| Lumbar Spine | ||
| Lumbar gravitational line | 6–5 | Anterior or posterior weight-bearing on lumbosacral disc |
| Lumbar lordosis angle | Hyperlordosis or hypolordosis determines stress on discs or facets | |
| Lumbosacral base angle | 6–7 | Determines shearing or compressive forces on discs and facets |
| Lumbosacral disc angle | Can be increased in facet syndrome | |
| Lumbar intervertebral disc angles | 6–7 | Can be increased in hyperlordosis |
| McNab’s line | Unreliable method of assessing facet impingement or imbrication | |
| Flexion-extension analysis | 6–12 | Measure of instability on lumbar flexion-extension views |
| Hadley’s “S” curve | Method of assessing facet impingement or imbrication | |
| Ullman’s line | For assessing presence of L5-S1 anterolisthesis | |
| Meyerding’s grading | 6–4 | Method of grading spondylolisthesis (Grades 1-5) |
| Eisenstein’s method | Lumbar sagittal canal diameter: stenosis or widening | |
| Interpediculate distance | Lumbar coronal canal diameter: stenosis or widening | |
| Canal/body ratio | Combined sagittal and coronal canal diameter | |
| George’s line | 6–6 | Disrupted in anterolisthesis or retrolisthesis |
| Cervical Spine and Skull Base | ||
| Chamberlain’s line | Basilar invagination, cranial settling, basilar impression | |
| McGregor’s line | Basilar invagination, cranial settling, basilar impression | |
| George’s line | Cervical or lumbar, anterolisthesis or retrolisthesis | |
| Posterior cervical line | Anterolisthesis or retrolisthesis or neural arch fracture | |
| Jackson’s lines | Alterations in physiologic stress lines on flexion-extension views | |
| Angle of cervical lordosis | 6–11 | Hypolordosis or hyperlordosis measurement |
| Cervical gravity line | 6–10 | Anterior or posterior weight-bearing |
| Cervical range of motion | Measurement performed on flexion-extension views | |
| Atlantodental interval (ADI) | Indicates atlantoaxial instability from transverse ligament damage | |
| Sagittal canal diameter | 6–8 | Stenosis or widening from intraspinal mass |
| Prevertebral soft tissue spaces | 6–9 | Inflammation, hemorrhage, or mass in soft tissues |