Chapter 13 Three Neurophysiologic Theories on the Chiropractic Subluxation
Chiropractic theory, subluxation, intervertebral foramen encroachment, joint receptors, proprioception, spinal cord traction, dentate ligaments
After reading this chapter you should be able to answer the following questions:
| Question 1 | Are the neural contents of the intervertebral foramen (nerve roots and dorsal root ganglion) equally sensitive to compression? |
| Question 2 | By what neurologic mechanism may nonvertebral joints such as the sacroiliac, ankle, or temporomandibular joint produce long-term influences on the central nervous system? |
| Question 3 | What are two ways in which traction through the dentate ligaments may influence neural impulses within the spinal cord? |
This chapter reviews three theories that are incorporated into our neurophysiologic model of the chiropractic subluxation. The name of each of these theories tells something of the mechanism by which we think the subluxation affects the nervous system:
Defining the term subluxation is necessary, even if a bit difficult. Chapter 1 on terminology introduced us to the scope of the problem. Chiropractic educators, legislators, philosophers, scientists, and practitioners hold tenaciously to a wide range of definitions. Here is a small but influential sample:
A vertebral subluxation is any vertebra out of normal alignment, out of apposition to its co-respondents above and below, wherein it does occlude a foramen, either spinal or intervertebral, which does produce pressures upon nerves, thereby interfering and interrupting the normal quantity flow of mental impulse supply between brain and body and thus becomes THE CAUSE of all disease. A vertebral subluxation IS a vertebral subluxation whenever it IS what is stated above, ALL elements being present. It is NOT a subluxation unless the interference to transmission is present. There can be no pressure upon nerves unless the size, shape, diameter, or circumference of the foramen is changed. There can be no change in the normal size, shape, diameter, or circumference of the foramen unless one vertebra is subluxated between its co-respondents above and below [emphasis by Palmer].1
Subluxation is an aberrant relationship between two adjacent articular structures that may have functional or pathological sequelae, causing an alteration in the biomechanical and/or neurophysiologic reflections of these articular structures, their proximal structures, and/or body systems that may be directly or indirectly affected by them.2
…interference with nerve transmission and expression, due to pressure, strain or tension upon the spinal cord, spinal nerves, or peripheral nerves as a result of a displacement of the spinal segments or other skeletal structures.3
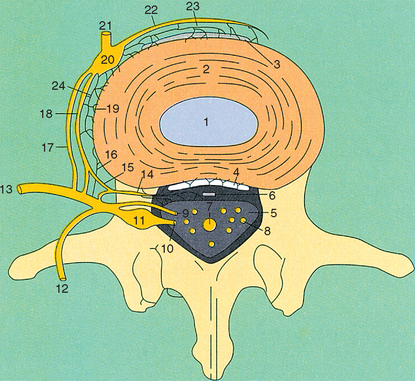
Intervertebral Encroachment Theory
It is now well established in the clinical literature that encroachment of neural structures within the intervertebral foramen (IVF) may produce pain and paresthesias, as well as changes in muscle tone and autonomic activity. The working assumptions are that pressure on the contents of the IVF either increases or decreases neural activity. Increased neural activity produces paresthesias, pain, hypertonic muscles, vasoconstriction, and sweating. Decreased neural activity produces numbness, muscle weakness/paralysis, vasodilation, and dry skin.
It is reasonable to ask, “Just how sensitive are the contents of the IVF?” We have learned that normal dorsal root ganglia (DRG), but not the spinal roots, may be stimulated by encroachment of the IVF. In small animal studies, compressive forces rapidly applied to normal dorsal roots (10 mg) produced only brief bursts (one to two seconds) of activity.4,5 Moreover, slowly increased pressure eventually produced a conduction block, but it did not evoke an active response within the root fibers. By contrast, DRG responded to small, slowly applied compressive forces (100 mg) with prolonged repetitive firing. Most ganglia neurons fired for at least 4 to 7 minutes; a few fired for 25 minutes.
Chronically injured dorsal nerve roots behave very differently.5 Injured roots may respond vigorously to mechanical pressure. Rapidly applied forces produce long bursts of activity (15 to 30 seconds), and even very slowly applied 10-mg pressures fire nerve root fibers. In addition, chronic peripheral nerve injury produces spontaneous discharges within DRG. Wall and Devor5 suggest that radiating limb pain reported during a Lasegue straight leg test could be caused by shifting the DRG to a position of increased mechanical stress. These investigators suggest that DRG discharges associated with peripheral nerve injury may explain phantom limb sensation and pain. They also comment:
These small animal studies are consistent with clinical experience.6,7 Slowly applied compression to a normal peripheral nerve (for example, the peroneal nerve is compressed by crossing legs) produces no pain but does produce numbness, paresthesias, and muscle weakness. By contrast, rapidly applied compression to an inflamed nerve produces pain and paresthesias (Tinel’s sign). At surgery, mechanical compression of normal spinal nerve roots produces sensory and motor impairment without pain. However, even minimal mechanical deformation of inflamed nerve roots produces radiating limb pain.
Recent studies demonstrate that small-caliber afferent nerve fibers do more than simply conduct impulses to the central nervous system. Stimulation of these primary afferents promotes the release of histologically potent neuropeptides such as substance P (SP) and vasoactive intestinal peptide (VIP) at their peripheral terminals.8,9 This observation has striking implications. It suggests that the peripheral origins of sensory fibers are important sites for neurologically mediated effects. We will consider the possible consequence of such a mechanism on back pain. As shown in Figure 13-1, the posterior anular fibers of the intervertebral disc are innervated by the recurrent meningeal (sinuvertebral) branch of the spinal nerve.10,11 Figure 13-2 demonstrates that the zygapophyseal joints are richly innervated by the medial branch of the posterior primary ramus of the spinal nerve.12 Therefore irritation of the DRG caused by intervertebral encroachment may cause release of neuropeptides within the intervertebral disc and the zygapophyseal joints. Earlier studies showed that SP and VIP stimulated breakdown of structural proteins.13,14 Over time, these neuropeptides may produce pathologic changes in the intervertebral disc and zygapophyseal joints.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree