Volar Wedge Graft for Scaphoid Non-Union with Humpback Deformity
Reid Abrams
Indications
Ruby and Mack independently reported the natural history of symptomatic scaphoid nonunions, presenting evidence that nearly all progressed to arthritis within 5 to 10 years after the original fracture and to generalized arthritis by 20 years (1,2). These studies have been extrapolated to justify surgical repair of all scaphoid nonunions due to the notion that if left untreated, arthritis will ensue (3). The logic of applying this treatment to all nonunions may not be entirely sound since the natural history of asymptomatic un-united fractures is unknown (4). The road to radiographic posttraumatic arthritis and associated symptoms may not be certain for all nonunions. For example, nondisplaced fibrous nonunions or un-united fractures not associated with carpal collapse may be at less risk.
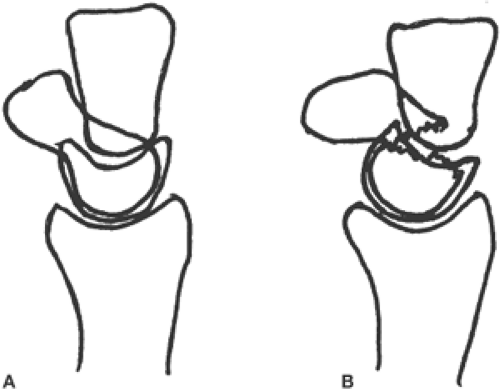
One consequence of a scaphoid fracture can be carpal instability. After a displaced scaphoid fracture, a flexion or so-called “humpback” deformity of the scaphoid occurs when the distal scaphoid fragment flexes anteriorly and the proximal pole, influenced by its attachment to the lunate, dorsiflexes (3,5,6) (Fig. 15-1). An ominous sign for the development of a nonunion is a scaphoid flexion deformity in the acute setting (7,8).
Fisk was among the first to emphasize the necessity of correcting carpal malalignment by reestablishing scaphoid length (5). In 1984, Fernandez distinguished different treatment strategies for scaphoid nonunions with and without carpal collapse (9). He promoted treating nonunions without carpal collapse with the Russe (10) technique. For those with carpal collapse, where restoration of scaphoid length is required, Fernandez proposed using a volar approach with iliac crest
corticocancellous structural graft, shaped to fill the triangular or trapezoidal defect missing from the volar side of the scaphoid (9).
corticocancellous structural graft, shaped to fill the triangular or trapezoidal defect missing from the volar side of the scaphoid (9).
While the treatment of asymptomatic long-standing nonunions may be controversial, the indications for repair of scaphoid nonunions with the “humpback” (or flexion) deformity with carpal collapse are less equivocal. There is evidence that if union is achieved and carpal collapse is corrected, the odds of developing posttraumatic arthritis can be diminished (11,12). Some authors believe that correction of carpal collapse is so critical that they have suggested corrective scaphoid osteotomy in cases of flexion malunion with residual carpal collapse, due to the notion that even if the scaphoid has healed but still has a flexion deformity, the malalignment leads to abnormal wrist kinematics, pain, and arthritis (13,14).
Contraindications
Generally, avoid surgery in patients unlikely to derive sufficient benefit to justify the risks. Surgeons should consider medical comorbidities, psychosocial and patient compliance issues, and patient needs and expectations when considering treatment options.
Volar wedge grafting is contraindicated in cases where it is deemed inappropriate, such as nonunions without carpal collapse (5,9).
Volar wedge grafting is not indicated in cases where there is already significant posttraumatic arthritis, or scaphoid nonunion advanced collapse (SNAC wrist) (15). However, it can be argued that in cases where only the tip of the radial styloid is involved and there is no midcarpal arthrosis, an attempt at achieving union is justified. In this case, radial styloidectomy should be part of the procedure to eliminate the arthritic part of the articulation.
Volar wedge grafting is probably not the optimal technique for treating scaphoid nonunions with a small proximal pole fragment. While this type of nonunion is problematic using any technique, volar wedge grafting probably is contraindicated for mechanical reasons because screw thread purchase in a diminutive proximal pole is suboptimal with distal to proximal screw insertion. Most surgeons endorse the use of a dorsal approach with antitrade screw insertion in this setting. While many hand surgeons also advocate vascularized bone grafting in the face of small proximal pole fragments and avascular necrosis (AVN), it is in this setting that vascularized bone grafts did the worst, with only about 50% of cases achieving union (16).
While not truly contraindications to surgery, there are some factors that may affect outcome adversely and that should be considered when assessing the probability of surgical success. These factors include smoking, fragment vascularity, patient age, and nonunion chronicity (3,16,17,18,19,20,21,22).
Preoperative Preparation
Anteroposterior, lateral, oblique, and ulnar deviation scaphoid views are used to assess nonunion location, displacement, angulation, carpal collapse, and the presence of arthritis. Coronal and sagittal computerized tomography (CT) scans may also assist in understanding fracture anatomy.
Watson et al. described a pattern of posttraumatic arthritis arising from scapholunate rotatory instability (scapholunate advanced collapse [SLAC] wrist) (23) as well as a similar type of arthritis associated with scaphoid nonunion with concomitant carpal collapse (SNAC wrist) (15). A characteristic of both entities is arthritis between the distal pole of the scaphoid and the radial styloid and sparing of the lunate fossa. In contrast to SLAC wrist, SNAC wrist has additional sparing of the articulation beneath the proximal pole of the scaphoid. In both SNAC wrist and SLAC wrist, as the process advances, there is progression to involvement of the midcarpal joint and eventually to pancarpal arthritis.
Before considering scaphoid nonunion repair, evaluation for the presence of arthritis is imperative, because if missed, even successful union may not fully alleviate the patient’s symptoms. In the setting of long-standing nonunion (more than 1–2 years), the status of the cartilage in the radial carpal joint should be evaluated. As mentioned previously, if a small portion of the radial styloid is involved, scaphoid nonunion grafting with radial styloidectomy can be considered. However, if a large portion of the radial styloid is involved or if there is midcarpal arthrosis, other reconstructive options are more appropriate, including scaphoid excision and proximal row carpectomy versus four-corner fusion (24,25,26). In the setting of pancarpal arthritis, total wrist fusion is the most reliable definitive treatment, but as the results of total wrist arthroplasty improve, this may also be a consideration in selected cases. Because routine radiographs may underestimate the amount of arthritis, arthroscopy has been a reliable adjunct in the evaluation prior to definitive reconstruction.
Some imaging findings have prognostic significance and are worth noting in the preoperative evaluation. There is a lower likelihood of healing with conventional bone grafting with increasing nonunion instability particularly apparent on traction radiographs (27). The more proximal the nonunion, the more guarded is the success of conventional bone grafting (18,27). The presence of proximal pole avascularity negatively affects union rate (19,22,28,29




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree