Scapholunate Advanced Collapse (SLAC) Reconstruction: Four-Corner Arthrodesis with Headless Screws
Kevin J. Little
Peter J. Stern
Indications and Contraindications
Alterations in wrist mechanics because of a functional loss of the scapholunate linkage usually progress to degenerative wrist arthritis. With loss of functional integrity of the scapholunate ligament, the scaphoid flexes and becomes incongruous with the elliptical fossa of the distal radius, leading to scapholunate advanced collapse (SLAC) (1). Similarly, a chronic scaphoid nonunion will lead to comparable radiographic and clinical findings. Classically, degenerative changes begin at the tip of the radial styloid (SLAC stage I) and progress to the obliteration of the entire radioscaphoid joint (stage II). Further collapse results in lunate extension and proximal capitate migration, leading to a dorsal intercalated segment instability (DISI) pattern. Finally, as the capitate migrates proximally, degenerative changes develop at the capitolunate articulation (stage III). The radiolunate articulation is nearly always spared (1).
SLAC wrist reconstruction is a salvage procedure designed to preserve wrist motion. It is indicated in symptomatic individuals who have failed nonsurgical treatment. The best indication is a stage III SLAC wrist where the capitolunate joint is destroyed. The radiolunate cartilage must be intact without carpal subluxation. Patients with avascular necrosis of the scaphoid (Preiser disease) or post-traumatic arthritis from distal radius fractures involving the radioscaphoid articulation are additional candidates for four-corner arthrodesis. Nondegenerative indications include chronic dynamic carpal instability, chronic perilunar instability, and nondissociative carpal instability (2).
The absolute contraindications include radiographic evidence of radiolunate arthritis, Kienböck disease, avascular necrosis of the capitate, and ulnar or volar carpal subluxation on the radius. Relative contraindications include inflammatory arthropathy (with the increased risk of ligament laxity
and carpal subluxation), a wrist arc of motion of less than 50 degrees in flexion and extension, and low demand patients.
and carpal subluxation), a wrist arc of motion of less than 50 degrees in flexion and extension, and low demand patients.
Preoperative Preparation
Obtain a thorough history of the affected wrist along with performing a focused and detailed physical examination. Patients commonly complain of dorsal wrist pain and dorsal-radial swelling with limited use of the affected extremity for work or activities requiring loading the wrist in extension. A wide range of physiologic conditions converge on the final common pathway of degeneration found in SLAC wrist; thus, the clinical history is quite varied. Many patients have undergone previous surgery. Patients with scapholunate ligament dissociation may have undergone a ligamentous reconstruction, whereas patients with scaphoid nonunion have had attempts at internal fixation, often with concomitant bone grafting procedures.
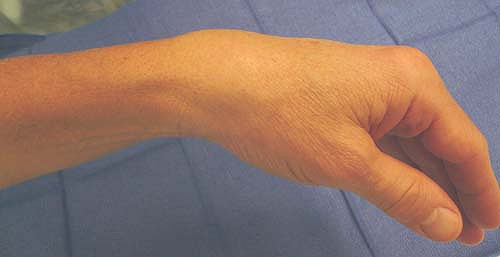
Most patients with SLAC wrist have remarkably similar physical findings (Fig. 25-1). There is dorsal-radial swelling and tenderness, especially with resisted wrist extension. Range of motion is often severely restricted in flexion–extension and decreased in radial and ulnar deviation. The Watson scaphoid shift test (passive radial deviation of the wrist with dorsal pressure on the scaphoid tuberosity) is often painful and may produce a palpable clunk. Document preoperative grip and pinch strength along with performing a thorough neurologic examination, including evaluation for carpal tunnel syndrome.
Standard posteroanterior (PA) and lateral wrist radiographs are mandatory (Fig. 25-2), and dedicated scaphoid views may be obtained if necessary. Occasionally, a computed tomography (CT) scan or magnetic resonance imaging (MRI) may be of benefit to evaluate the extent of degenerative changes.
Surgical Technique
Place the patient supine with the affected extremity on a hand table. Either general or regional anesthesia is appropriate and preoperative antibiotics are given.
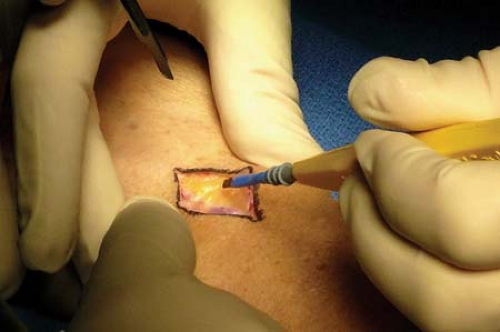
Use an upper-arm tourniquet, and exsanguination with an Esmarch is recommended before tourniquet insufflation. We recommend a midline dorsal longitudinal incision along the axis of the third metacarpal centered over Lister’s tubercle (Fig. 25-3).
Preserve the superficial veins and branches of the radial and ulnar sensory nerves by using blunt dissection (Fig. 25-4).
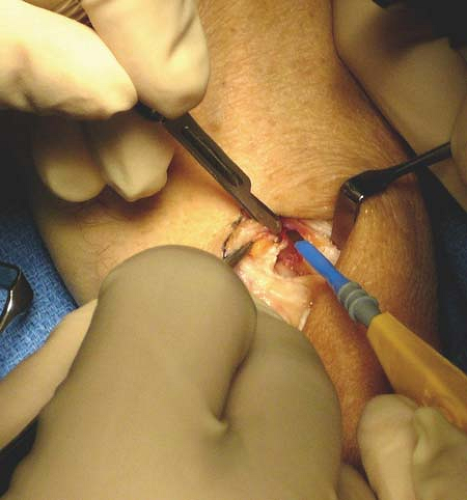
Carry the dissection down to the extensor retinaculum, which is incised longitudinally over the third dorsal compartment and then remove the exposed extensor pollicis longus (EPL) tendon from the compartment and retract it radially (Fig. 25-5).
Perform a longitudinal arthrotomy ulnarly to the extensor carpi radialis brevis (ECRB) tendon (Fig. 25-6).

Figure 25-5 The extensor pollicis longus (EPL) tendon is identified and retracted radially. * EPL; †, Extensor carpi radialis brevis (ECRB).
Utilizing sharp subperiosteal dissection, elevate the wrist capsule radially and ulnarly along the dorsal lip of the distal radius. In so doing, the tendons of the fourth and fifth dorsal compartments are protected in their retinacular envelope.
Take great care not to enter the distal radioulnar joint (DRUJ) when carrying the dissection towards the ulna.
Reflect the capsule from the carpal bones as well, exposing the capitolunate, lunotriquetral, capitohamate, and hamatotriquetral joints that are to be arthrodesed.
At this time, longitudinal traction or hyperflexion of the wrist will expose the radiolunate joint and the cartilage should be assessed for arthritic changes. If present, consider conversion to total wrist arthrodesis.
Expose the scaphoid and incise all ligamentous attachments (Fig. 25-7).
Excise the scaphoid in one piece (Fig. 25-8). A large, threaded Steinmann pin can be inserted down the longitudinal axis of the scaphoid for leverage. A Bennett or Hohman retractor placed under the distal pole also facilitates detachment of the scaphoid tuberosity from the volar wrist ligaments. This can be difficult if scar tissue is present, such as with prior scaphoid surgery.
Preserve the volar wrist ligaments, particularly the radioscaphocapitate ligament, during this stage to prevent postoperative ulnar carpal translocation.
Denude the capitolunate joint of remaining articular cartilage and subchondral bone to expose the underlying cancellous marrow (Fig. 25-9). We prefer the creation of a cup and cone that mimics the patient’s anatomy. The dorsal lip of the lunate should be excised to allow for easier access to this joint. We discourage the use of a high-speed burr because of the risk of thermal necrosis and delayed union.
Remove the dorsal three fourths of the cartilage and subchondral bone in the lunotriquetral (LT) and hamatotriquetral (HT) joints with a rongeur. We do not make an effort to formally arthrodese the capitohamate joint.
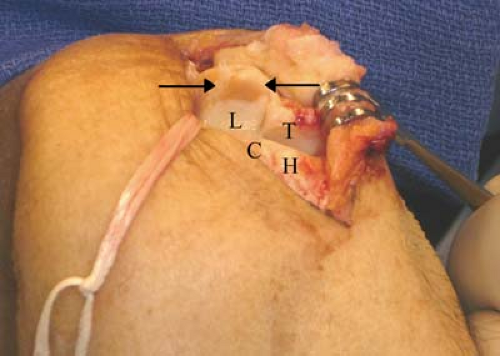
Figure 25-9 Hyperflexion of the wrist exposing the arthritic capitolunate joint. Note arrows indicating dorsal arthritis. L, lunate; T, triquetrum; C, capitate; H, hamate.
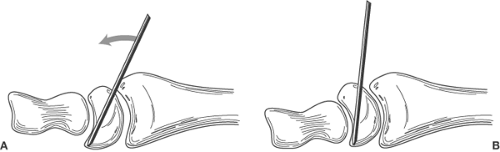
Figure 25-10 Drive a 0.062-inch Kirschner wire (K-wire) antegrade and volar into the lunate (A), and it can be used as a joystick to bring the lunate into an anatomic position (B).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree