Arthrodesis of the Rheumatoid Wrist
Andrew L. Terrono
Paul Feldon
Indications and Contraindications
Although the radiologic appearance of the wrist joint influences the type of reconstruction, the indications for surgery are clinical. Absolute indications include disabling pain that is unresponsive to nonoperative treatment coupled with deformity or instability that impedes hand function. A painless, well-aligned wrist with minimal motion provides good function regardless of the radiologic appearance and rarely requires operative treatment.
When it has been determined that nonoperative treatment (including splinting, steroid injections, and systemic medication) have failed, consider surgery. Frequently, even with minimal wrist motion and moderate wrist joint destruction, most of the discomfort and functional disability is associated with problems of the distal radioulnar joint (DRUJ). In these cases, distal ulna surgery without radiocarpal reconstruction is advised. Radioulnar reconstruction is less disabling than radiocarpal fusion and is effective in these patients. However, when pain is located in both joints, appropriate radiocarpal and DRUJ reconstruction is necessary.
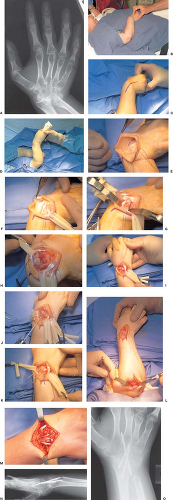
Occasionally, patients require simultaneous wrist arthrodesis and metacarpophalangeal (MP) joint arthroplasty. Such patients should meet the indications for wrist fusion as well as MP joint arthroplasty. The wrist should have minimal deformity and not need to be dislocated to expose the joint surfaces or reduce the joint (Fig. 38-1A). By realigning a deformed wrist, correcting deviation, and eliminating wrist pain, the results of the MP joint arthroplasty are improved (1). This less extensive exposure allows the MP joint arthroplasty to be carried out with minimal risk of excessive postoperative swelling and the attendant risk of skin slough or other complications. A contraindication for the proxcedure is extensive deformity that requires wrist dislocation and major dissection.
In most cases, total wrist fusion is the recommended procedure for radiocarpal reconstruction. It is a safe, well-established procedure with few complications. It is a definitive operation that provides a pain-free, well-aligned, and stable wrist that improves hand function.
Preoperative Planning
Ask the patient to describe all problems, including pain and functional deficits, and to identify specifically what physical activities cannot be done, as well as what activities are desired.
Perform a physical examination of the entire upper extremity. Record range of motion, active and passive, of the digits, wrist, forearm, elbow, and shoulder. Seek areas of tenosynovitis, synovitis, crepitus, tenderness, and instability.
On physical examination of the wrist, determine if pain is primarily caused by radiocarpal or radioulnar joint abnormalities. The radiocarpal joint should be tender and painful when evaluated. Synovitis is not seen in all cases. If the wrist is the major source of problems and is well aligned, evaluate the MP joints for the need for simultaneous MP joint arthroplasty. When a wrist fusion is performed, a DRUJ reconstruction is done simultaneously, if indicated.
Completely evaluate the elbow and shoulder. If the elbow and shoulder have very limited flexion and the flexed wrist allows the hand to get to the mouth, then first address shoulder and elbow function. The wrist is fused in slight flexion in these patients.
Obtain radiographs, neutral posteroanterior, lateral, and oblique views, including the hand, to evaluate the MP joints. However, radiographs do not correlate well in all cases with the clinical picture. The radiographs may show severe destruction when symptoms are minimal. Also evaluate the DRUJ. If an intramedullary pin is going to be used, evaluate the metacarpals and distal half of the radius for deformity and medullary diameter to judge pin size and whether intramedullary fixation is possible.
Technique
Expose the wrist under tourniquet control, using a longitudinal dorsal incision, usually centered in the midline of the wrist (Fig. 38-1C).
Take the incision to the level of the dorsal retinaculum, and form the radial and ulnar skin flaps as required for the proposed surgery. The dorsal branches of the radial and ulnar sensory nerves, frequently seen as the flaps, are formed (Fig. 38-1E), noted, and protected with this approach.
Section transverse communicating veins and preserve the longitudinal veins.
After skin flaps are formed, place retraction sutures (3-0 silk) in the skin edges.
Make a longitudinal incision into the fourth or sixth extensor compartment. In this instance, preferring to enter the fourth compartment, raise the radial and ulnar (Fig. 38-1F). Alternatively, the fourth compartment can be opened in a Z-fashion to allow closure of the retinaculum in a lengthened fashion (see Chapter 37).
Make transverse incisions proximal and distal to the retinaculum, allowing the retinaculum to be reflected as a flap as the vertical septum between each compartment is opened.
Perform tenosynovectomy and distal ulnar excision before arthrodesis (see Chapter 32, 37).
Expose the radiocarpal joint, using a longitudinal capsular incision. If palmar dislocation of the carpus is needed to prepare the joint surfaces and allow proper wrist alignment, elevate the capsular flap to allow complete exposure of the radial styloid. (Fig. 38-1H).
With any difficulty exposing the radius, release and retract the first extensor compartment tendons before releasing the radial capsule from the radial styloid to facilitate exposure and to avoid injury.
Use rongeurs to carry out the synovectomy.
Remove cartilage and sclerotic bone from the radius and carpal bones. This includes the radius; the proximal, distal, and intracarpal surfaces of the scaphoid, lunate, and triquetrum; and the proximal surfaces of the capitate and hamate. The scaphotrapezial, trapezoid, and carpometacarpal
joints are not included routinely. The amount of bone removed depends on the degree of deformity and destruction present. With significant palmar and ulnar erosion of the radius secondary to palmar subluxation of the carpus, more dorsal and radial bone needs to be removed to correct the deformity and realign the wrist. With extensive destruction of the proximal carpal row, these bones can be removed and used for bone graft, and the distal carpus can be fused to the radius. Iliac bone graft is not used routinely; however, local bone grafts (metacarpal heads, distal ulnar) are used when available.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree