Synovectomy and Tendon Reconstruction
Andrew L. Terrono
Indications and Contraindications
Frequently performed operations for patients with rheumatoid arthritis affecting the digital extensor tendons and wrist joint are dorsal tenosynovectomy, wrist joint synovectomy, extensor tendon reconstruction, and reconstruction of the distal radioulnar joint (DRUJ). We usually combine wrist denervation with any dorsal wrist surgery. This chapter addresses the operative indications, surgical techniques, and expected outcomes of each of these procedures.
Dorsal Tenosynovectomy
Dorsal tenosynovectomy is indicated for wrists with tenosynovitis that persists despite several months’ adequate medical treatment, which includes systemic medications plus one or two steroid injections. An even more compelling indication is aggressive disease in a patient who has an enlarging mass despite adequate treatment. An absolute indication for surgery is a tendon rupture, because one rupture often foretells a second. Patients with mild disease under good control tolerate dorsal tenosynovitis well without tendon rupture, thus careful observation should be considered instead of surgery.
Synovectomy
The indications for synovectomy remain controversial; no long-term studies have shown that this procedure changes the natural history of the disease. This is certainly true for the wrist joint, in which the surgeon’s technical ability to carry out a complete synovectomy is limited because of the anatomic configuration of the joint.
The indications for synovectomy, therefore, are few. Wrist synovectomy is recommended for patients whose arthritis is under relatively good medical control and whose radiographs show minimal changes in the radiocarpal joint, but who continue to have isolated synovitis despite two to three steroid injections over a 6- to 9-month period. If other wrist surgery, such as dorsal tenosynovectomy or distal ulnar excision, is being considered and there is clinical evidence of radiocarpal synovitis, especially with pain, a synovectomy is performed even on patients whose radiographs reveal more advanced destruction.
Indications for isolated radioulnar synovectomy are more limited. Radioulnar joint synovitis causes destruction of the triangular fibrocartilage complex (TFCC) very early during the disease, leading to instability of the distal ulna with relation to the distal radius. Destruction of the TFCC is an indication for distal ulna excision with reconstruction of the DRUJ.
Extensor Tendon Reconstruction
Tendon rupture necessitates extensor tendon reconstruction. Tendon ruptures are secondary to direct invasion, attrition, or ischemia. Most frequently, patients with dorsal tenosynovitis or caput ulnae syndrome (1) suddenly notice the inability to extend a single digit, usually one of the two ulnar digits. Sometimes when there is a rupture of the extensor digiti minimi (extensor digiti quinti), the patient may not notice any dysfunction or may note only that the control of the digit is not normal. Extensor pollicis longus (EPL) rupture, which occurs frequently, may go unnoticed until a physician discovers it.
When a tendon rupture occurs, prompt exploration, tenosynovectomy, and removal of osteophytes, as needed, are advisable to prevent additional tendon ruptures. When a rupture is detected on routine examination, treatment depends on the situation. Often, a ruptured extensor digiti minimi or ruptured EPL is seen without dorsal tenosynovitis and is secondary to attrition rupture. In such a case, when no functional impairment exists, no treatment is needed.
Reconstruction of the Distal Radioulnar Joint
Involvement of the radioulnar joint by rheumatoid arthritis is one of the most frequent findings in the rheumatoid hand; it may cause significant disability. For this reason, distal ulna excision, with reconstruction of the triangular fibrocartilage and DRUJ, is a frequently indicated operative procedure.
The most compelling reason for surgery is a painful dislocated or subluxed distal ulna with limited rotation and tendon ruptures. Another indication is a dislocated distal ulna with persistent pain unresponsive to nonoperative treatment without extensor tendon ruptures. Painless limited rotation is a relative indication and surgery is recommended only if it impairs a patient’s function. Minimal loss of rotation, especially pronation, is compensated for by shoulder abduction, and may not lead to functional impairment.
Tendon Transfers to Restore Wrist Balance
Tendon transfers to restore wrist balance are indicated in patients undergoing dorsal wrist surgery who have a passively correctable radial deviation deformity. In these cases, relocation of the extensor carpi ulnaris (ECU) tendon or transfer of the extensor carpi radialis longus (ECRL) tendon to the ECU insertion is performed. This may be helpful in preventing further deformity when simultaneous metacarpophalangeal (MP) joint surgery (either extensor realignment or arthroplasty) or wrist synovectomy is performed (4).
Preoperative Planning
Begin by asking the patient to describe all problems, including pain and functional deficits—specifically, what he or she cannot do but would like to be able to do.
Perform a physical examination of the entire upper extremity. Record active and passive range of motion of the digits, wrist, forearm, elbow, and shoulder. Seek out areas of tenosynovitis, synovitis, tenderness, and instability.
Take routine neutral posteroanterior, lateral, and oblique radiographs, including the wrist and hand, to evaluate the MP, radiocarpal, and distal radioulnar joints.
Because dorsal tenosynovitis is painless, its major clinical significance is its propensity to cause tendon rupture. The configuration of swelling is usually oblong along the direction of the extensor tendons and may move with the extensor tendons. Tenosynovectomy is performed to prevent tendon rupture.
Synovitis associated with rheumatoid arthritis usually causes pain that helps differentiate it from tenosynovitis. Radiocarpal synovitis may present with a painful dorsal wrist mass; the synovium, however, may not be palpable. Synovitis is suspected when flexion and extension cause pain and the radiocarpal joint is tender. There should not be a fixed deformity, and radiographs should show minimal changes. If there is a passively correctable radial deviation deformity, add an ECU tendon relocation or an ECRL tendon transfer.
Synovitis involving the DRUJ invades the ulnar styloid, the ulnar head, and TFCC early in the disease, destroying the joint and the supporting structures. The DRUJ is tender and rotation is limited. Radiographs show only mild changes and extensor tendon function is intact.
Extensor Tendon Surgery
The diagnosis of tendon rupture is made by the absence of the tenodesis effect, a difference between active and passive MP joint motion, and the inability to maintain a corrected position of digital MP joint extension, often with associated dorsal tenosynovitis. Seek out sources of attrition ruptures, such as the distal ulna or Lister’s tubercle of the radius. Evaluate the number of ruptures and sources for tendon transfer (extensor indicis proprius [EIP], wrist extensor if a simultaneous wrist fusion is performed, EPL if thumb fusion is performed), or graft (e.g., the palmaris longus). Passive MP joint motion should be good; if not, consider simultaneous MP arthroplasty. If the cause is attrition rupture on the distal ulna, perform reconstruction of the DRUJ simultaneously. Use radiographs to evaluate the patient for sources of attrition ruptures or a need for a simultaneous procedure (wrist fusion, DRUJ reconstruction, MP arthroplasty).
Reconstruction of the Distal Radioulnar Joint
The DRUJ often has synovitis and is incongruous; it causes the patient to have pain with rotation and palpation. The distal ulna often is unstable, snaps during rotation, and is prominent. A supination deformity of the carpus that often is seen in conjunction with the final result of synovitis of the DRUJ is the caput ulnae syndrome (1), manifested by dorsal dislocation of the distal ulna, supination deformity of the carpus, and frequent tendon ruptures. Radiographs document these changes and are helpful in evaluating the wrist for ulnar translocation (Fig. 37-1). Often, a small shelf of bone supports the lunate (Fig. 37-2). Sometimes this shelf of bone cannot be seen until after the
distal ulna is excised (7). If the radius no longer supplies any support to the lunate, a partial or total radiocarpal fusion is performed (9).
distal ulna is excised (7). If the radius no longer supplies any support to the lunate, a partial or total radiocarpal fusion is performed (9).
 Figure 37-1 Radiograph showing ulnar carpal impingement with carpal erosion into the radius without ulnar translocation. |
Tendon Transfers to Restore Wrist Balance
The most important part of the preoperative planning is to ensure that the radial deviation deformity is passively correctable, to decide if relocation of the ECU or ECRL transfer to the ECU is appropriate, and to ensure the ECRL and extensor carpi radialis brevis are working. The effect of ECU relocation can be tested preoperatively: The wrist is placed in supination, and if the ECU can ulnar deviate the wrist in this position, then surgical relocation of the ECU dorsally is performed to help correct the radial deviation deformity. If the ECU cannot ulnarly deviate the wrist with the forearm in supination, an ECRL to ECU tendon transfer is performed. This transfer maintains the ECU in the dorsal position, augments active ulnar deviation, helps prevent carpal supination, and opposes ulnar translocation. Otherwise, plan as you would for the other surgery that is being performed (4).
Technique
Dorsal Tenosynovectomy Technique
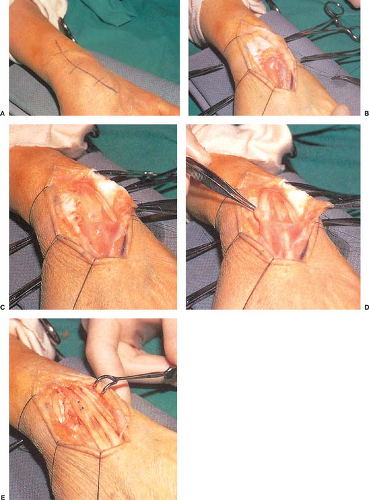
Use a dorsal longitudinal incision (Fig. 37-3A).
Take the incision to the level of the dorsal retinaculum, and form radial and ulnar skin flaps as required for the proposed surgery. The dorsal branches of the radial and ulnar sensory nerves frequently are seen as the flaps are formed; note and protect them. Section transverse communicating veins.
Preserve longitudinal veins.
After the skin flaps are formed, place retraction sutures in the skin edges (Fig. 37-3B).
Make a longitudinal incision into the fourth or sixth extensor compartment; I prefer to enter the fourth compartment. Alternatively, the fourth compartment can be opened in a “Z” fashion to allow closure of the retinaculum in a lengthened fashion. Raise radial and ulnar flaps (see Chapter 1).
Make transverse incisions proximal and distal to the retinaculum, allowing the retinaculum to be reflected as a flap as the vertical septum between each compartment is opened (Fig. 37-3C).
Identify the EPL tendon and open the septum.
With evidence of tenosynovitis around the wrist extensor tendons, open the second compartment. If needed, the second compartment can be evaluated by incising only part of the septum. If there is no evidence of tenosynovitis, the tendons are not disturbed. In routine dorsal tenosynovectomy, the first compartment is not opened unless there is clinical evidence of involvement (Fig. 37-3D, E). The posterior interosseous nerve is resected to partially denervate the joint.
After the radial tendons are exposed, incise the vertical septum separating the fourth and fifth compartments, exposing the extensor digiti quinti tendon.
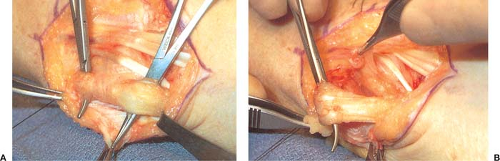
Carefully dissect the retinaculum off the radioulnar joint until the subsheath of the ECU is identified (Fig. 37-4A). If the ECU is subluxed palmarly, careful dissection is necessary to isolate and expose both the tendon sheath and tendon. In these cases, leave the ulnar retinacular flap attached to the septum between the fifth and sixth compartments to use later to relocate the ECU tendon dorsally.
Open the ECU sheath, perform a tenosynovectomy with sharp dissection, and open the subsheath if necessary to perform the tenosynovectomy (Fig. 37-4B).
When there is invasive tenosynovitis, open the roof of the tendon longitudinally to remove diseased tissue (Fig. 37-3E).
Remove as much of the tissue as possible; adherent tissue is sometimes impossible to remove.
Repair frayed tendons; when imminent rupture is apparent, carry out side-to-side suture.
After completion of the tenosynovectomy, close the retinaculum. Rarely, part of the retinaculum or the entire retinaculum is placed deep to the tendons to cover bone spurs and thereby protect the extensor tendons (Fig. 37-3E). If the retinaculum was opened in a “Z” fashion, it is closed in a slightly lengthened side-to-side fashion to prevent overtightening.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree