Wayne G. Paprosky
Michael O’Rourke
Use of Structural Allografts in Acetabular Revision Surgery
INTRODUCTION
The number of acetabular revisions will rise as the incidence of total hip arthroplasty increases. Revision arthroplasty accounted for approximately 17% of the 168,106 hip arthroplasty procedures performed in the United States during 1999, and the volume is expected to increase to 273,819 hip arthroplasties by 2030. Forty percent of these patients are under the age of 65 years.1
Cementless fixation in revision acetabular surgery has improved outcomes over cemented components.2–7 Reliable and durable fixation of cementless acetabular components requires an environment with adequate biologic potential (i.e., intimate contact of viable living bone with the implant) and mechanical stability (i.e., motion <40 to 50 μm) to allow for bone ingrowth.8 The challenge during revision surgery is achieving these prerequisites in the face of bone loss.
To achieve a successful reconstruction, the surgeon must survey the damage (extent and location of bone loss), determine if biologic fixation is achievable based on the remaining host bone surface area for ingrowth, and determine if the initial mechanical cup stability will support ingrowth.
Reconstruction without cementless implants is necessary if the biologic potential for ingrowth does not exist. When adequate surface area for ingrowth is present and the implant has adequate initial stability, a hemispherical cementless implant can be placed. The use of allograft in these circumstances provides a stimulus for bone reconstitution should future procedures be necessary.
In the presence of adequate surface area for ingrowth without initial stability of the cup, the surgeon must decide how to improve the mechanical environment to obtain stability. The options include superior placement of the component,3 jumbo cup,9–12 nonhemispherical components (oblong components),13–15 metal augments, and structural allograft.16–18 The benefits of structural allografting in these situations include restoration of anatomic hip center, maintenance of remaining host bone, and biologic restoration of significant bone loss.
BACKGROUND
Allogenic bone grafting can be used to initiate restoration of host bone through the processes of osteoinduction and osteoconduction. In addition, allograft may provide a mechanical role to support implants. Historically, allograft has been used to provide mechanical support for acetabular components in both primary and revision surgery with the use of cemented acetabular components (Table 18.1).19–21 Although initial successful reconstructions were obtained, longer term follow-up has shown increasing mechanical failure. Presumably, the failure occurs as a result of weakening of the allograft bone during the remodeling process22 or as a result of fatigue failure.23
TABLE 18.1 Summary of the Literature
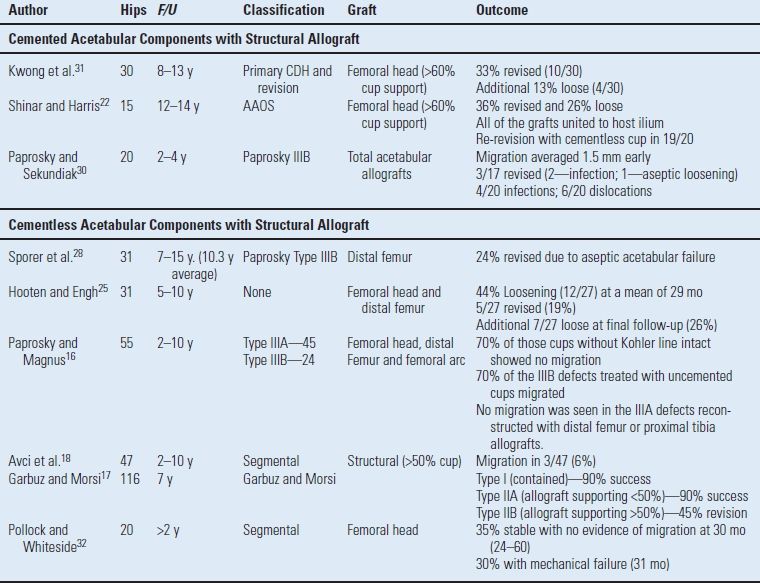
Unlike cemented acetabular reconstruction where the stability is the greatest at the time of surgery, long-term durability of a cementless implant is dependent on the biologic interface that develops between the host and the implant. Ingrowth into a cementless component will not occur in areas of contact with allograft even if the allograft revascularizes and remodels.24 Therefore, successful cementless reconstruction using structural allograft is related to the degree of support the allograft is providing (Table 18.1).16–18,25
It is difficult to compare the results of reconstructive methods in the literature because defining the amount and location of bone loss is difficult and has been inconsistent. Defining the proportion of support from allograft has not been consistent. Some authors define support based on the medial to lateral percentage of coverage seen on an AP pelvis radiograph21,22,25 and others define degree of support based on intraoperative criteria.16,26,27
Exposure Preoperative planning is critical in order to have the appropriate grafting material, tools for implant removal, and components available. If significant medial migration is present on preoperative imaging, additional imaging (angiography or computer tomography with intravascular contrast infusion) is recommended. An extensile exposure is recommended during acetabular revision in order to address unanticipated bone loss. The superior ilium and posterior column are dissected in a subperiosteal plane in order to visualize the anterior and superior ilium. After the removal of existing components, a systematic debridement of granulation tissue and interface membrane is performed to assess the entire remaining acetabular bone stock and rule out the possibility of a pelvic discontinuity.
Structural Allograft Principles As mentioned above, the choice of the graft to match the mechanical demands is very important for optimum outcome. We do not use femoral head allografts when the graft serves a structurally supportive role. Fresh frozen distal femur or proximal tibial allografts are used to orient the trabecular patterns parallel direction of load to optimize stress transfer. The grafts are contoured to maximize contact surface area between the host bone and the allograft to optimize union rates. It is important to have separate fixation between the allograft and host bone outside of the fixation of the implant. The fixation of the allograft is generally with 6.5-mm screws oriented parallel with one another in the direction of loading without interfering with component placement or fixation. Finally, if gross motion from a pelvic discontinuity exists, fixation with a posterior column plate should be performed before proceeding with the allograft.
Distal Femoral Figure Seven Allograft.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








