Fig. 49.1
(a) Anteroposterior and (b) lateral radiographs of fully cemented stems used for revision TKR

Fig. 49.2
(a) Anteroposterior and (b) lateral radiographs of a revision TKR using a hybrid cement technique, with cement visible around the metaphyseal portion of the implant and a diaphyseal filling press-fit stem distally
Stemmed implants are inserted using either a fully cemented technique or a so-called hybrid technique, where the undersurface of the implant and the metaphyseal region of the stem are cemented and the distal portion of the stem is press fit tightly into the diaphysis.
49.1 Press-Fit or “Cementless” Stems
Proponents of a hybrid technique, where the stem is tightly press fit in the diaphysis, argue that this provides diaphyseal engagement of the stem while minimizing the problems associated with fully cemented stems, particularly difficulty of removal if required. Among the advantages of a cementless stem is an easier surgical technique. Full engagement of the tibia canal will lead to a neutral position of the tibial component with appropriate slope (Fig. 49.3). Similarly, engaging the femoral isthmus will position the femoral component in the amount of valgus as determined by the femoral stem (5–7º depending on the manufacturer) and allow for the simple identification of need for distal femoral augmentation with the trial in place to restore appropriate alignment. However, canal engagement does often lead to the need for an offset stem as the center of the canal and the center of the cut surface of the epiphysis may not be the same, particularly on the tibial side where the tibial canal is typically posteromedial to the tibial plateau.
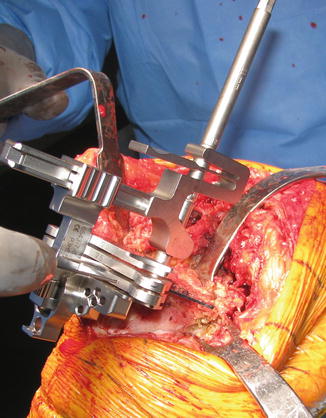
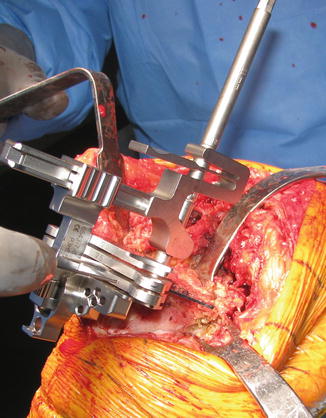
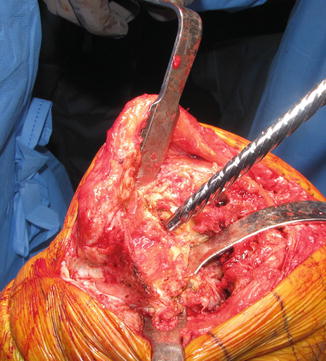
Fig. 49.3
After a secure fit is obtained with the hand reamer in the tibial canal, the proximal tibial cutting guide is pinned into position. Pinning the cutting guide with the intramedullary reamer in place allows the proximal tibia to be cut perpendicular to the mechanical axis of tibia
Press-fit stems can be associated with end-of-stem pain, due to the elasticity modulus mismatch of the metal with the cortical bone [3, 4]. The end-of-stem pain has been associated with older age, female sex, and poor bone quality and is more often seen in the tibia. Symptoms, however, are intermittent and usually resolve within a year or two of occurrence [5]. The prevalence of end-of-stem pain also seems to be highly dependent on the materials that the stems are made of, with cobalt chrome alloy stems having a much higher reported prevalence than ones made of titanium, which are much more commonly used in contemporary practice [4]. Finally, there is a small incidence of fractures associated with press-fit stems which is approximately 3 % in our experience. These fractures are more commonly seen on the tibial side and are typically only seen as incidental findings on the postoperative radiographs. These rarely require specific treatment as they are often minimal or nondisplaced (Fig. 49.4a–c) and heal uneventfully with no evidence of loosening at a mean of 23-month follow-up [6]. In some cases, we have used fracture braces such as a “PTB” or patellar tendon-bearing braces for tibial fractures for patient comfort, but it is unclear if these are necessary.
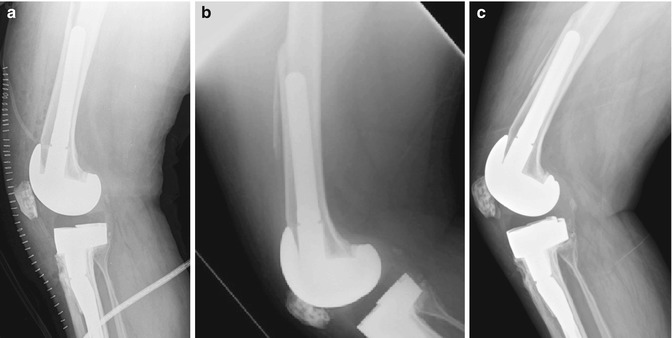
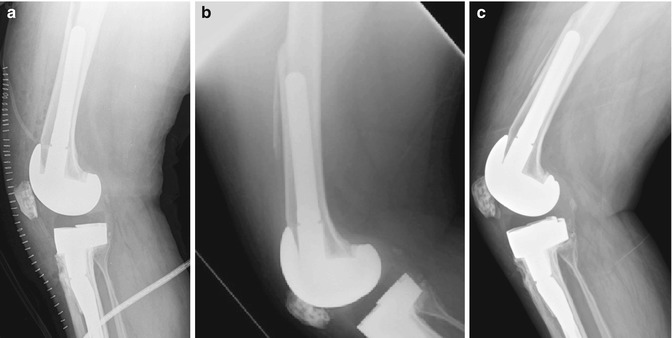
Fig. 49.4
(a) Initial postoperative lateral radiograph of a patient after revision total knee replacement using a press-fit technique into the femoral canal. The radiograph demonstrates an anterior fracture in the femoral cortex. (b) Follow-up radiographs at 5 months postoperatively showed interval healing of the fracture without any radiographic signs of loosening. (c) Without any intervention, the patient went on to heal the fracture, as is shown, at her 27-month follow-up visit
Press-fit stems can be associated with end-of-stem pain, which is more frequently seen in the tibia. It is due to the elasticity modulus mismatch of the metal with the cortical bone.
The fixation strength of fully cemented and diaphyseal-engaging stems has been studied. In a cadaveric study of 12 knees, Jazrawi et al. found that implants with cementless stems demonstrated more micromotion than cemented components of the same length [7]. However, the difference was eliminated by using a longer cementless implant that engaged the diaphysis distally. The authors concluded that cementless implants offer similar stability to shorter fully cemented designs and may reduce or eliminate long-term problems associated with cement use. Another cadaveric study of 20 knees confirmed the improved stability of a so-called hybrid technique of cementing only the surface of the implant and leaving the stem uncemented compared to full cementation [8].
49.1.1 Clinical Results of Press-Fit Stems
In a recent review of 88 revision TKRs, Sah et al. documented a 5- and 10-year survival rate of 100 and 90 %, respectively, using aseptic loosening as the endpoint [5]. The end-of-stem pain occurred in 2 patients but resolved by 1 year postoperatively. Radiosclerotic lines were seen commonly in 75 % of tibial and 65 % of femoral components but were nonprogressive and had no impact on pain or function. The results of additional studies detailing the results of this technique are shown in Table 49.1 [1, 5, 9–13].
Table 49.1
Results of revision TKR using cementless stems
Author | Year | Number of patients | Mean follow-up (range) | Survivorship (endpoint) | Complications/complaints |
|---|---|---|---|---|---|
Wood et al. [10] | 2009 | 127 (135 knees) | 5 years (2–12 years) | 87 % at 12 years (re-revision), 98 % at 12 years (aseptic loosening) | 6 revisions at a mean of 3.5 years, 13 % nonprogressive radiolucent lines |
Peters et al. [11] | 2005 | 47 (50 knees) | 2.5 years | 91 % (infection), 100 % (aseptic loosening) | 4 % thigh/leg pain |
Bottner et al. [12] | 2006 | 33 | 38 months | 93 % (aseptic loosening), 97 % (infection), 91 % (re-revision) | 87 % moderate/occasional pain during walking |
Shannon et al. [1] | 2003 | 60 (63 knees) | 5.75 years (2–10) | 81 % (re-revision), 90 % (aseptic loosening), 96 % (infection) | 2 revised for instability |
Sah et al. [5] | 2011 | 83 (88 knees) | 65 months (24–126 months) | 100 % at 5 years (aseptic loosening), 90 % at 10 years (aseptic loosening) | 2 patients had end-of-stem pain; radiosclerotic lines seen in 75 % of tibial stems and 65 % of femoral stems but did not affect outcome |
Peters et al. | 2009 | 184 knees | 49 months | 100 % at final follow-up (aseptic loosening), 91.% (all re-revisions) | 13/15 failures were secondary to deep implant infection |
49.1.2 Surgical Technique: Press-Fit Stem
After the original components have been removed, the tibia is prepared first as the tibia effects both the flexion and extension gaps. Fibrous tissue within the canal is removed, and the pedestal is penetrated if one exists usually with a crochet hook. The tibia is then reamed by hand until a secure fit is achieved within the tibial canal (Fig. 49.5). At that point, the tibial cutting guide is pinned into position to recut the epiphyseal surface; this typically involves removal of minimal bone (Fig. 49.3). We prefer to make our cut in neutral slope so that rotation is more easily adjusted later. The intramedullary reamer is left in position while pinning the cutting guide to ensure that the cut is perpendicular to the mechanical axis. Once the cut has been made and the tibial component sized, we use a trial to determine appropriate stem length and diameter, which will not necessarily correlate with the last reamer utilized. Specifically, the stem is chosen to obtain 1–2 cm of press fit within the canal so that the final implant requires forceful insertion with a mallet (Fig. 49.6). As previously mentioned, an offset stem is typically required on the tibial side to optimize coverage and prevent component overhang (Fig. 49.7a). The offset is almost always anterior and lateral as the tibial canal is centered medially and posteriorly with regard to the tibial plateau (Fig. 49.7b).