Uncemented Acetabular Revision with Hemispherical Cups
Craig J. Della Valle
Erdan Kayupov
INDICATIONS AND CONTRAINDICATIONS
A hemispherical cementless acetabular component can be used for most acetabular revisions that the surgeon will encounter in practice. We prefer to use the Paprosky classification (1) for acetabular defects, and in this classification, a cementless hemispherical acetabular component, with or without some particulate bone grafting, is appropriate for almost all type 1 and 2 defects as well as some type 3A defects.
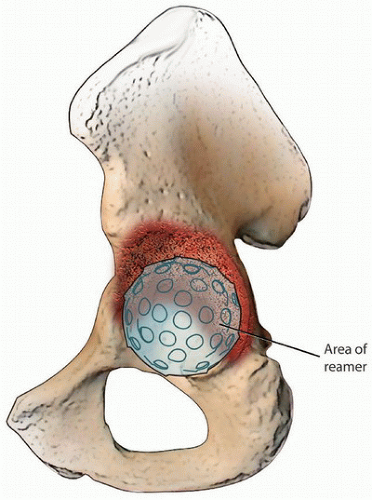
Type 1 and 2A/2B defects are similar defects that are characterized by less than 3 cm of proximal migration of the failed acetabular component with intact acetabular columns. Type 2C defects are characterized by central protrusion of the component beyond Kohler’s line; however, the anterior and posterior columns are typically intact, although there can be damage to the anterior wall of the acetabulum (Fig. 23-1). These defects, while having a dramatic appearance, are easily handled with a hemispherical cup and medial bone grafting. Specifically, the acetabular rim is carefully reamed to accept the shell and the medial defect is filled with particulate, fresh frozen cancellous graft that is tightly reverse reamed into the medial defect. The surgeon should be careful if these types of defects are associated with deep infection or acute loosening as this has been associated with a higher risk of vascular injury upon retrieval of the failed cup (2). Finally, 2C defects may occasionally be associated with a pelvic discontinuity, which is covered below under contraindications.
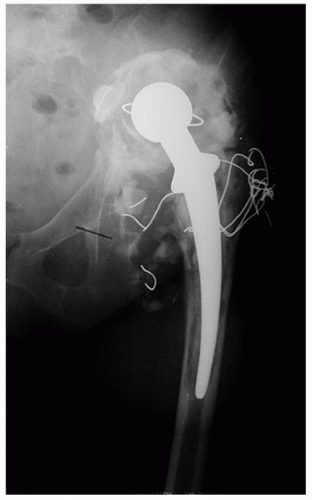
Type 3A defects are characterized by greater than 3 cm of proximal migration with an “up and out” appearance (Fig. 23-2). In some of these cases, a hemispherical cup can be used alone. Specifically, these defects are typically oblong, and if the surgeon can convert this defect to a hemisphere with the reamer, without damaging or sacrificing the anterior and posterior walls, then a hemispherical cup can be utilized alone. In general, most surgeons will accept up to 1 cm of elevation of the center of rotation before some type of augmentation is utilized superolaterally. If, however, the surgeon cannot fill the defect top to bottom without damaging the acetabular walls and/or columns, then
superolateral augmentation is required to restore a reasonable center of rotation and the limits of a hemispherical cup alone have been reached (Figs. 23-3 and 23-4).
superolateral augmentation is required to restore a reasonable center of rotation and the limits of a hemispherical cup alone have been reached (Figs. 23-3 and 23-4).
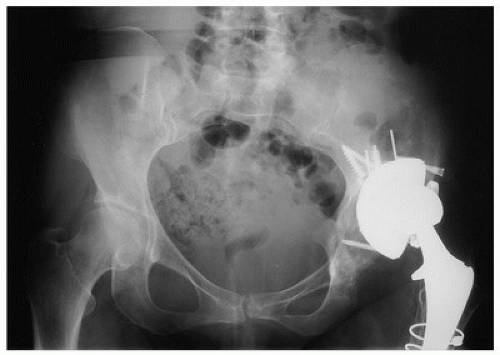 FIGURE 23-2 Paprosky 3A defect with greater than 3 cm of proximal migration of the acetabular component with an “up and out” pattern. |
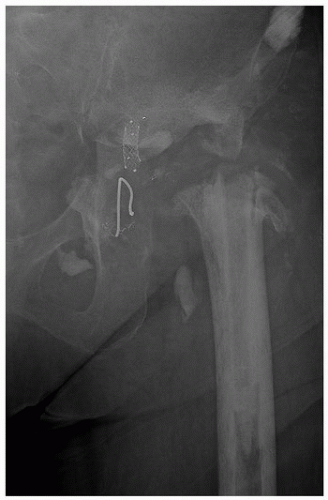
Paprosky type 3B defects are characterized by greater than 3 cm of proximal migration of the failed component combined with substantial damage to the posterior column, which is usually identified as ischial lysis (Fig. 23-5). In this case, given the damage to the posterior column, which is the main stabilizing structure for a cementless cup, some type of augmentation or alternative reconstructive technique will be required. Similarly, the presence of a pelvic discontinuity is a contraindication to the routine use of a hemispherical cementless cup alone and specialized techniques for reconstruction will be required (3). Radiographic signs of pelvic discontinuity include a visible fracture line through the posterior column (oftentimes seen most easily on a Judet view of the pelvis), asymmetry of the obturator foramen when compared to the contralateral side, and medial translation of the inferior hemipelvis (Fig. 23-6). Risk factors for the occurrence of pelvic discontinuity include female sex and rheumatoid arthritis (3).
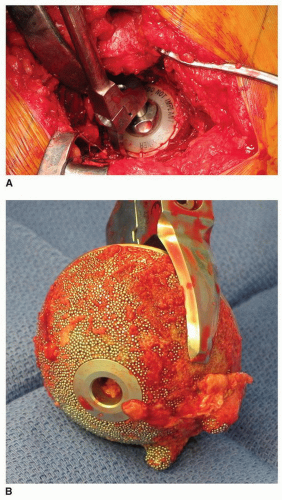
In general, successful osseointegration will occur if the component is mechanically stable and placed in close contact with viable, living bone, and hence, a history of prior irradiation to the pelvis is another contraindication to the use of a cementless hemispherical cup (4); in this situation, a strong mechanical construct (such as a reconstruction cage) is required. While surgeons often reference specific percentages of host bone contact required for the successful use of a hemispherical
cementless cup, this is not only difficult to assess intraoperatively but also not supported by objective data. Hence, as previously described, if the defect encountered can be reamed into a hemisphere and the posterior column is intact to provide long-term support, a cementless acetabular component alone can be used in most cases, so long as the center of rotation is not elevated greater than 1 cm and initial implant stability can be achieved (typically with multiple screws for fixation) so that osseointegration can occur to provide long-term fixation.
cementless cup, this is not only difficult to assess intraoperatively but also not supported by objective data. Hence, as previously described, if the defect encountered can be reamed into a hemisphere and the posterior column is intact to provide long-term support, a cementless acetabular component alone can be used in most cases, so long as the center of rotation is not elevated greater than 1 cm and initial implant stability can be achieved (typically with multiple screws for fixation) so that osseointegration can occur to provide long-term fixation.
PREOPERATIVE PREPARATION
As with any revision procedure, preoperative planning is crucial to an efficient operative procedure with the lowest risk of complications and optimal outcomes for the patient.
As in all revision procedures, deep infection should routinely be ruled out, as the treatment of infection is fundamentally different than if the reason for failure is aseptic:
Obtain a serum erythrocyte sedimentation rate and C-reactive protein (CRP).
Aspirate the hip if the ESR and CRP are elevated or if clinical suspicion for infection is high (5).
The fluid obtained should be sent for a synovial fluid white blood cell count (optimal cutoff value approximately 3,000 WBC/µL), a differential (optimal cutoff value approximately 80% neutrophils), and culture.
Next, it is critical to obtain the prior operative note to determine the manufacturer, model, and size of the implants currently in place. Knowledge of the prior implanted cup size is particularly important if the cup being revised is well fixed, as this will facilitate its removal using curved osteotomes that are specifically sized to the diameter of the implanted cup (Fig. 23-7). Similarly, if screws
were utilized as part of the original reconstruction, their number should be known to facilitate cup removal; even a loose cup can be difficult to extract if screws are still in place. Along the same lines, special screwdrivers may be required, and finally, trial liners are once again needed to use the curved acetabular osteotomes previously referenced (Fig. 23-7). Specialized instruments from the manufacturer may also facilitate removal of the liner. The operative note will also yield critical information regarding the make and model of the femoral component so that appropriate trials and replacement femoral heads are available should the femoral component be retained. If the femoral component is to be removed, knowledge of its geometry and extent of coating will determine the strategies for its removal.
were utilized as part of the original reconstruction, their number should be known to facilitate cup removal; even a loose cup can be difficult to extract if screws are still in place. Along the same lines, special screwdrivers may be required, and finally, trial liners are once again needed to use the curved acetabular osteotomes previously referenced (Fig. 23-7). Specialized instruments from the manufacturer may also facilitate removal of the liner. The operative note will also yield critical information regarding the make and model of the femoral component so that appropriate trials and replacement femoral heads are available should the femoral component be retained. If the femoral component is to be removed, knowledge of its geometry and extent of coating will determine the strategies for its removal.
SURGICAL TECHNIQUE
The first step in any hip procedure starts with a decision on which surgical approach to utilize, and our preference is the posterior approach as it is technically easy to perform and easily extensile and allows for exposure of the posterior column if required. It is also compatible with an extended trochanteric osteotomy if required and does not damage the abductors. Once the hip capsule has been exposed, the hip is aspirated and an intraoperative synovial fluid white blood cell count is obtained, if one has not been done preoperatively to evaluate for infection (Fig. 23-8). The hip capsule and short external rotators are then released off of the back of the femur as one continuous layer and tagged for later repair (Fig. 23-9




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree