Tapered Fluted Titanium Stems in Revision Total Hip Arthroplasty
Nemandra A. Sandiford
Clive P. Duncan
Bassam A. Masri
Donald S. Garbuz
INTRODUCTION
A wide variety of tapered fluted titanium stems are currently used in the setting of revision total hip arthroplasty (THA). There are no prospective studies comparing all available designs; hence, no clearly superior stem has been demonstrated.
Irrespective of design, the aim of revision THA is to accurately restore the center of rotation and produce a pain-free stable hip.
Modular components allow the surgeon to independently achieve stable diaphyseal fixation while optimizing anteversion, horizontal offset, and leg length. Such intraoperative versatility has made them an attractive option for use in the revision setting. Choosing the correct indication for their use, careful preoperative planning, and good surgical technique have led to promising clinical outcomes with the use of these components (1,2).
ADVANTAGES OF MODULAR TAPERED FLUTED STEMS
Modular tapered fluted stems are ideally suited to cases with Paprosky types II and III bone deficiencies (3,4). They offer the following advantages in the revision setting.
Excellent axial and rotational diaphyseal fixation is achieved with the tapered fluted distal stem segment. The tapered stem forms a wedge that provides axial stability within the femoral isthmus while the cutting flutes engage the endosteum and create rotational stability.
Modular proximal segments with variable offset and length options allow for optimization of length, offset, soft tissue tension, and anteversion.
Independent sizing of the proximal and distal segments facilitates optimization of bone contact with the entire surface area of the implant. This is thought to contribute to the reconstitution of proximal femoral bone stock observed with the use of these stems (5).
Titanium is more flexible than the previously popular cylindrical chrome-cobalt stems, contributing to less flexural stiffness and less stress shielding.
PREOPERATIVE PLANNING
Careful preoperative planning allows anticipation of technical difficulties that can be encountered during the procedure, choice of the surgical exposure, and availability of the appropriate implant sizes and design to enable restoration of the center of rotation and normal biomechanics of the hip. Accurately templated radiographs are a prerequisite in the revision setting. The entire in situ component must be visible as well as the distal extent of any existing cement mantle. The femoral metaphysis, diaphysis, and isthmus must be clearly visible.
Our practice is to use calibrated digital images, which correspond to the magnification of our template overlays. A transischial line is drawn first to assess for true leg length discrepancy. The acetabulum is templated first and the center of rotation determined. On the femoral side, the type of implant, mode of fixation, degree of fixation, and its location relative to the center of the canal are noted. The risk of cortical perforation and an iatrogenic fracture during stem extraction is increased in the presence of an eccentric stem or cement mantle as well as in the presence of varus remodeling or greater trochanteric position over the medullary canal.
The point where maximal fixation will be achieved is clearly marked. The need for an extended trochanteric osteotomy (ETO) can also be predicted and is built into the preoperative planning. Our indications for an ETO are
Presence of a well-fixed uncemented component.
Varus (coronal plane) and/or flexion (sagittal plane) remodeling of the proximal femur. This will be recognized during templating on both the anteroposterior and lateral radiographs.
Presence of a well-fixed cement mantle is a relative, yet common, indication.
Placing overlay templates on the lateral radiograph gives an indication of the degree of femoral bow and the need for a bowed or beveled component or the need for a corrective osteotomy in that plane as well. A number of the stems available have an anterior bevel to minimize the risk of perforating the anterior cortex. This also provides another guide to the orientation of the component during the stem insertion.
Once the region of optimal fixation is marked out, the anticipated stem size is chosen. The overlay has a cutout, which allows one to mark the most proximal extent of the stem. This is further referenced from an intact bony landmark such as the greater or lesser trochanter. The proximal (body) segment is templated from this point. The ideal length and offset are also determined. The authors use a large head whenever possible (36 or 40 mm) to reduce the risk of instability. Also, to prevent the risk of junctional fracture, we prefer to use the largest body at the junction that is offered by the manufacturer.
OPERATIVE PROCEDURE
Surgical Setup
The patient is positioned in the lateral decubitus position.
If acetabular reconstruction is contemplated as well, great care must be taken to position the patient so that the coronal plane of the pelvis is positioned perfectly perpendicular to the operating room table. This is achieved by centering the posterior support on the sacrum and the anterior support on the lateral 1/3 of the iliac crest. This anterior support is placed at the level of the umbilicus and angled distally to the iliac crest in order to allow greater than 90 degrees flexion during the procedure. The entire limb is prepped to the iliac crest. It is draped free allowing access to the entire thigh. Old incisions are marked out prior to placing the iodine-impregnated skin drape.
Incision
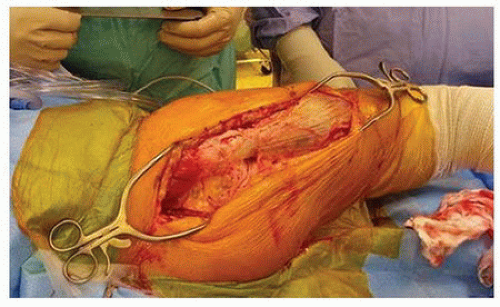
We routinely use a posterior approach incorporating the old scar if possible. This is extensile, enables exposure of the entire femur if necessary, and allows clear visualization and protection of the sciatic nerve (Fig. 28-1). This also allows an extended femoral osteotomy should that be necessary.
Surgical Procedure (See Videos 28-1 through 28-5)
After extraction of the failed prosthesis, acetabular revision, if required, is the next step followed by insertion of the femoral component, which is the focus of this chapter. Femoral component insertion can be performed with or without an ETO. Both techniques are described in this chapter.
Technique without an Extended Trochanteric Osteotomy Endofemoral Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree