The Tapered Stem
Peter Pyrko
William J. Hozack
Cementless fixation in total hip arthroplasty emerged as a result of the perceived need for more durable long-term fixation. Cementless stems have yielded variable results depending on surgical technique, implant, and patient population. Results with tapered stems, however, appear reproducible and require fewer surgical steps (1,2). This surgical simplicity produces more predictable results. Ten-year results in a number of patient groups seem to indicate that the technique is more versatile than is cemented stem fixation (1,3,4,5,6). Recent study with 20 to 25 years of follow-up also yielded excellent results (7). In addition, the use of second-generation stems in younger patients has also been recently shown to result in positive results (8). While cemented total hip arthroplasty continues to have its advocates, it has been largely replaced by cementless technique using a taper stem in North America. Initial experiences with cementless fixation yielded results that were marred by a number of problems such as femoral fracture, subsidence, thigh pain, and stress shielding. Many of these problems associated with early cementless femoral components have been since addressed (9,10). Currently, cementless femoral fixation with a tapered prosthesis is a straightforward and reliable alternative to more technically demanding cemented femoral fixation.
INDICATIONS/CONTRAINDICATIONS
The tapered stem is ideally suited to provide fixation in femora with a broad spectrum of bone stock, bone quality, and underlying patient biology. Dorr types A and B femora have been considered the best bone types for cementless fixation. Initially, cementless fixation was thought unsuitable for the patients with Dorr type C proximal femora (such as in patients with rheumatoid arthritis and osteoporosis). The Dorr type C osteoporotic femur has an increased risk of intraoperative femoral fracture. Additionally, a larger stiffer implant is required to produce primary stability, which can result in thigh pain and greater stress shielding especially when cobalt chrome implants are utilized. Experience and published results have shown this not to be as common with a tapered titanium implants (6,7). Currently, successful results are possible in Dorr type C bone with tapered titanium stems. Of course, if there is any concern about the stability of initial fixation, then a cemented implant should be utilized. There have also been some concerns about cementless fixation in type A femora, where the traditional cementless prosthesis might engage distally and toggle loose proximally when the patient mobilizes. Design changes in cementless stems that focus on metaphysical fixation to facilitate more anatomical load transfer and reduce distal diaphyseal fixation seem to have addressed this particular femoral morphology (11).
PREOPERATIVE PLANNING
Preoperative templating should determine the appropriate center of rotation of the hip and femoral neck resection level (Fig. 16-1). This can assure reproducible results (12). Both standard acetate templates and computer templating software can be used. AP view of the pelvis centered over the sacrum is used with legs in 15 degrees of internal rotation to provide en face view of the anteverted femoral necks and allow correct evaluation of the femoral offset. Radiographic preoperative leg length discrepancy (LLD) is measured. Templating should follow typical surgical sequence: cup first and then the femur. The cup is placed at the level of the teardrop with approximately 40 degrees of abduction and medialization
to the ilioischial line. The size is determined by adequate lateral coverage without removal of excess subchondral bone. Special consideration may have to be undertaken for protrusio acetabuli and dysplastic hips. If the contralateral hip is not affected by disease, templating can be performed on the contralateral side. The goal of templating of the femur is to predict the implant of appropriate size for the femoral canal, to predict the neck cut length, and to restore femoral offset and equalize the limb length. Leg length is reestablished by placing the center of rotation of the femoral head above the center of rotation of the acetabular component for a shortened limb and below the center of acetabular component for a limb that needs to be shortened. The vertical distance between the two centers of rotation is the numerical correction of LLD in millimeters. These measurements, of course, are approximations that must be confirmed intraoperatively. The horizontal distance between these two centers on medial to lateral axis signifies the increase or decrease in femoral offset after the surgery. Standard or higher offset stems can be then used as needed based on radiographic evaluation. In general, templating should estimate and record the following parameters: preoperative LLD, length of the neck cut, estimated sizes of the femoral and acetabular components, and estimated femoral offset.
to the ilioischial line. The size is determined by adequate lateral coverage without removal of excess subchondral bone. Special consideration may have to be undertaken for protrusio acetabuli and dysplastic hips. If the contralateral hip is not affected by disease, templating can be performed on the contralateral side. The goal of templating of the femur is to predict the implant of appropriate size for the femoral canal, to predict the neck cut length, and to restore femoral offset and equalize the limb length. Leg length is reestablished by placing the center of rotation of the femoral head above the center of rotation of the acetabular component for a shortened limb and below the center of acetabular component for a limb that needs to be shortened. The vertical distance between the two centers of rotation is the numerical correction of LLD in millimeters. These measurements, of course, are approximations that must be confirmed intraoperatively. The horizontal distance between these two centers on medial to lateral axis signifies the increase or decrease in femoral offset after the surgery. Standard or higher offset stems can be then used as needed based on radiographic evaluation. In general, templating should estimate and record the following parameters: preoperative LLD, length of the neck cut, estimated sizes of the femoral and acetabular components, and estimated femoral offset.
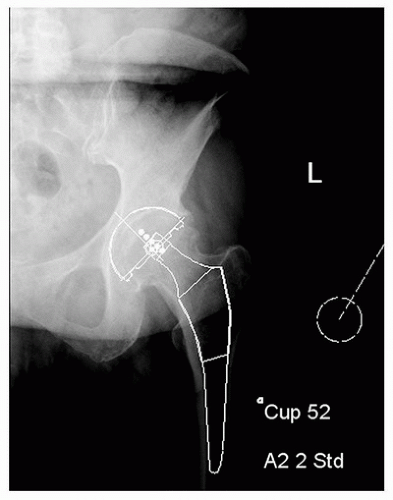 FIGURE 16-1 Careful templating offers a guide to femoral and acetabular sizing, and it can predict if a stem with a standard or high offset should be used. |
Multiple studies have shown that well-performed templating can predict LLD correction in more than 90% of patients based on the preoperative plan and that in majority of patients, LLD will be less than 1 cm (13,14,15). The most common errors in execution of a template are lengthening due to inferior cup positioning and increased offset due to inadequate medialization (16).
Design Rationale
The double-tapered design is ideally suited to permit fixation within the proximal femur and to provide immediate axial and rotational stability. Cadaver studies by Sharkey et al. (17) have demonstrated that initial axial and rotational stability following implantation of a tapered stem was comparable to that of a cemented prosthesis. Should initial stability be insufficient for bone ingrowth, the component will subside. Unlike some alternative designs, subsidence of a tapered stem may reestablish implant stability within the proximal femur, providing again the environment for bony ingrowth. The disadvantage is that the restoration of leg length and stability might be compromised. Hence, only small amounts of subsidence should be tolerated.
The wide variation in proximal femoral anatomy and concerns about creating an excessively stiff prosthesis are a further advantage of the tapered stem. A tapered titanium stem provides a progressive transition from bulky and relatively inflexible proximal segment to the narrower and more flexible distal section. This, in turn, permits the loading of the proximal femur and theoretically protects against the effects of stress shielding. Redesign of the tapered femoral components, focusing on proximal metaphyseal fixation and minimization of diaphyseal engagement, also has proven to reduce stress shielding (11).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








