The Direct Lateral Approach for Total Hip Arthroplasty
Stuart B. Goodman
The direct lateral approach (DLA) to the hip joint is a versatile surgical exposure that can be used for primary and simple revision total hip arthroplasty (THA), where an extensile dissection to visualize the pelvis or femur is not needed (1,2). It is easily and quickly accomplished, gives excellent exposure both to the native acetabulum and proximal femur, and has few complications (3,4). It is particularly valuable in patients with excessive anteversion because the proximal femur is dislocated anteriorly, directing the femoral head and neck into the wound site.
The approach has been modified dramatically by many surgeons from the original description by Mr. Brian McFarland of Liverpool in 1954 (5) and then termed the “transgluteal approach to the hip joint” by Professor Bauer et al. of Austria (6). The “direct lateral approach to the hip” was popularized in the United Kingdom and worldwide by Mr. Kevin Hardinge in 1982 (7) and by Dr. Desmond Dall (8). Since these descriptions, the surgical approach has been modified for the use of smaller incisions with less dissection but does not sacrifice full exposure of the structures necessary to perform the hip replacement with precision (9,10).
INDICATIONS
Primary THA
Simple revision THA without need for an extensile exposure
Drainage and debridement of an infected THA early when the implants are stable and only liner and head exchange are contemplated
Resection arthroplasty of a native hip joint
CONTRAINDICATIONS
Accepted contraindications to primary THA using any surgical approach (ongoing joint sepsis, severe abductor muscle deficiency, etc.)
Previous adjacent incisions to the one contemplated, that may jeopardize wound healing
Extensive scarring involving the tissues to be dissected due to previous burns, trauma, irradiation, etc.
Complex primary THA where an extensile approach is needed, for example, a Crowe type 4 arthritic hip needing THA with major acetabular and femoral exposure with possible shortening femoral osteotomy
Complex revision THA with the need for an extensile exposure
Revision THA where a previous satisfactory posterior approach has been performed
Resection arthroplasty needing wider exposure, with possible extended femoral osteotomy
PREOPERATIVE PREPARATION
The preoperative preparation for THA using the DLA is very similar to THA using other surgical approaches.
In addition to a complete history, physical examination, appropriate imaging, and blood work studies, a fully informed discussion should take place preoperatively concerning the risks, benefits, and expectations of the patient. As patients are mobilized early after surgery, and hospital stays are very short, preoperative weight loss and strengthening programs may be indicated. In this respect, exercises in a pool may be useful in building flexibility and physical endurance, as well as patient confidence. The patient should undergo comprehensive medical assessment as indicated to help ensure a smooth perioperative course.
As for any THA surgery, preoperative planning is essential to ensure that all appropriate implants and sizes are available for the surgery. Preoperative planning can be performed using computer-assisted methods or simple radiographs and commercially available acetate templates.
TECHNIQUE
The patient is given an anesthetic as recommended by the anesthesia team. This may be a general, spinal, epidural, or other anesthetic or combination thereof. In general, our patients generally elect to undergo spinal anesthesia with sedation ± general anesthesia. A urinary catheter is placed in most patients except the very young. Antibiotics are given prophylactically.
The DLA to the hip may be performed with the patient in the supine or lateral position. I elect to place the patient in the lateral position so that the soft tissues move away from the wound when incised, and all assistants can see the surgical procedure. The patient is positioned in the lateral decubitus position on a pegboard, and an axillary roll is placed so as not to press on the brachial plexus proximally or impede the axillary vasculature. At least four well-padded pegs are used to stabilize the pelvis and torso: one peg at the symphysis pubis, one on the chest wall just superior to the abdomen, one on the pelvis posteriorly just proximal to the anal cleft, and one adjacent to the thoracic spine. The pelvis should be aligned and secured in a direct lateral position and not flexed excessively. I prefer an arm board and two pillows to secure the upper extremities. The operative extremity is widely abducted and held with the appropriate table attachment device. The lower nonoperated limb is padded. A nonsterile U drape is placed around the operative lower extremity, lifting the buttock to attach the drape well posteriorly for wide exposure of the pelvis. Anteriorly, the drape is placed below the anterior superior iliac spine. The operative extremity is then prepared with antiseptic solution from the ankle to the chest, and the limb is draped in sterile fashion.
After a time-out to verify all aspects of the operative procedure, the incision is marked and iodine-impregnated coverings are placed over the wound.
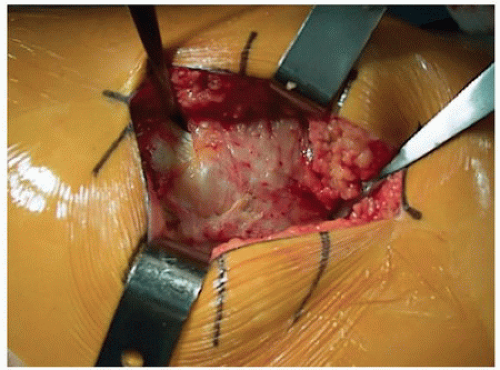
The incision is different for patients with different body habitus. The superior pole of the greater trochanter and proximal femoral shaft are palpated. The incision is centered over the greater trochanter and is as short or long as needed for adequate exposure. In general, the incision begins just proximal and slightly posterior to the superior pole of the greater trochanter and progresses slightly anteriorly to just beyond the palpable trochanteric crest (Fig. 2-1). The fascia lata is incised along this line. The bursa overlying the greater trochanter is incised. This exposes the gluteus medius muscle and tendon, the greater trochanter, and the proximal vastus lateralis (Fig. 2-2). A small Hohmann retractor is placed just superior to the greater trochanter through the musculotendinous junction of the gluteus medius. Distally, a similar Hohmann retractor is placed at the junction of the anterior one-fifth and posterior four-fifth of the gluteus medius several centimeters below the trochanteric line. (Note: One modification is to place the more distal retractor immediately anterior to the vastus lateralis.) An inverted gentle U is made with the electrocautery, connecting the two Hohmann retractors. The vastus-gluteal flap is then created in one of the following ways. If the bone stock is good-excellent, a sharp osteotome is used to take a sliver of bone with the flap so as to decorticate the greater trochanter of small bone chips (Fig. 2-3). This will provide a bone-to-bone attachment during closure. The decortication starts inferiorly and superiorly where the tendon is thickest and proceeds toward the middle (where the tendon is thinnest) from above and below, proceeding medially. Once the trochanter has been traversed medially, one looks for the pericapsular fat from below and then sharply creates the entire flap including anterior iliofemoral
ligaments as one thick flap. If the bone stock is poor or the greater trochanter is small, the risk for trochanteric fracture is higher, so no bone is taken; the flap is developed with a knife or cautery.
ligaments as one thick flap. If the bone stock is poor or the greater trochanter is small, the risk for trochanteric fracture is higher, so no bone is taken; the flap is developed with a knife or cautery.
 FIGURE 2-1 The skin incision is drawn on the upper thigh of the left hip. The dot represents the superior pole of the greater trochanter. |
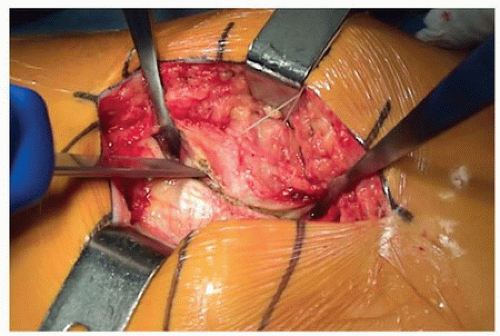
Once the flap is developed, I usually use a tagging suture for later easy identification during closure (Fig. 2-3). Large sharp Hohmann retractors are carefully placed over the anterior lip of the
acetabulum, and a dull Hohmann is placed below the inferior hip capsule (Fig. 2-4). A small sharp Hohmann or Hibbs retractor is placed over the superior capsule. Sometimes the capsular insertion of the gluteus minimus or straight head to the rectus femoris needs to be sharply dissected off the capsule. The capsule is incised in a T fashion and either preserved or excised (I excise it for better visualization). The posterior capsule is left intact for stability. The hip joint is gently dislocated anteriorly using the Hohmann retractors around the femoral neck as guiding levers, with the assistant on the opposite side of the operating table giving slight traction then performing a flexion, adduction, and external rotation maneuver (Fig. 2-5



acetabulum, and a dull Hohmann is placed below the inferior hip capsule (Fig. 2-4). A small sharp Hohmann or Hibbs retractor is placed over the superior capsule. Sometimes the capsular insertion of the gluteus minimus or straight head to the rectus femoris needs to be sharply dissected off the capsule. The capsule is incised in a T fashion and either preserved or excised (I excise it for better visualization). The posterior capsule is left intact for stability. The hip joint is gently dislocated anteriorly using the Hohmann retractors around the femoral neck as guiding levers, with the assistant on the opposite side of the operating table giving slight traction then performing a flexion, adduction, and external rotation maneuver (Fig. 2-5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree