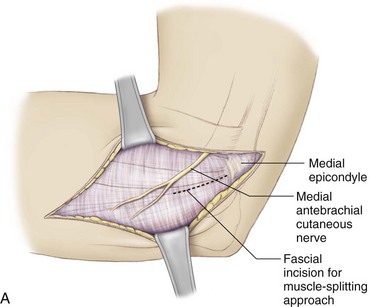
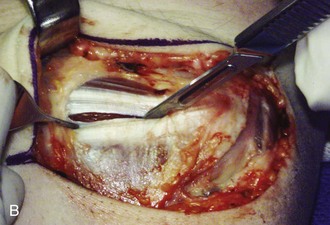
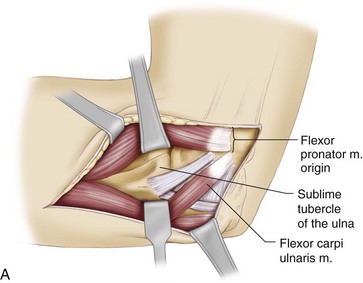
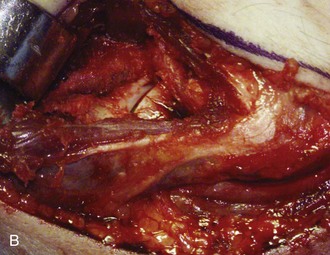
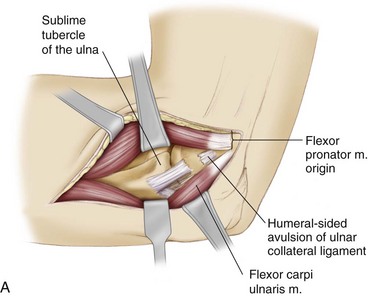
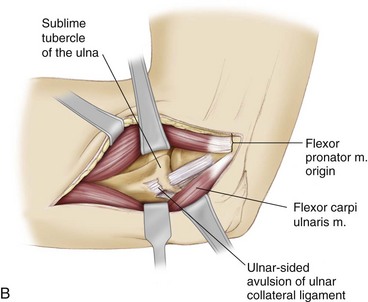
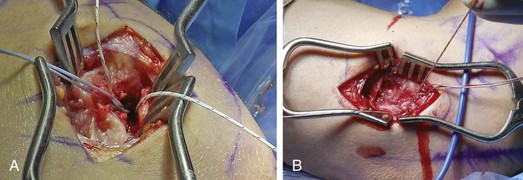
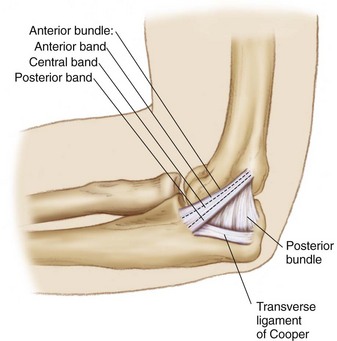
Chapter 46 Part 1 Ulnar Collateral Ligament Repair Injury to the medial side of the elbow is common in overhead athletes, such as baseball pitchers, tennis players, and javelin throwers. The overhead throwing motion places tremendous valgus stress on the elbow that is resisted by the medial structures. The anterior bundle of the ulnar collateral ligament (UCL) has been shown to be the primary restraint to valgus stress about the elbow.1 Repeated high valgus stresses imparted from the repetitive act of throwing can result in chronic attenuation or acute rupture of the UCL. In the throwing athlete, UCL insufficiency can manifest as disabling elbow pain with the inability to compete effectively. Various techniques of UCL reconstruction have been reported with high rates of success in returning the athlete to competition; however, an increased incidence of UCL injuries in younger patients has led to consideration of primary repair as a surgical option. Many young athletes may have injury that is isolated to either the humeral or the ulnar insertion and thus is amenable to direct repair, perhaps allowing earlier return to sport. Recent reports have detailed high rates of success in early follow-up.2,3 Constants in operative management include an accurate diagnosis, careful patient selection, anatomic repair of the UCL insertion, and maintenance of a specific rehabilitation program to allow the athlete to return successfully to sport. The typical history in a throwing athlete with UCL injury is episodic medial elbow pain that prevents him or her from competing effectively. Pain is usually elicited in the early acceleration phase of throwing. Affected pitchers complain of loss of velocity or accuracy. On occasion the athlete will sustain an acute injury with sudden onset of medial pain accompanied by a “pop” followed by an inability to continue throwing. Less commonly, patients report a history of a fall on an outstretched hand or direct trauma to the elbow followed by medial elbow pain and swelling.2 Symptoms of ulnar nerve irritability, such as paresthesias, in the little and ring fingers can also be present. A thorough physical examination of the throwing athlete includes the following: • Evaluation of the neck and entire upper extremity • Direct assessment of the ulnar nerve for subluxation, irritability (presence of Tinel sign), and integrity of distal motor and sensory function in the hand Several tests have been described to evaluate the integrity of the UCL: These tests may elicit medial elbow pain with valgus stress, or the examiner may appreciate medial joint line opening with stress especially in comparison with the contralateral elbow. The possible presence of concurrent posteromedial impingement in the thrower’s elbow can be evaluated with the valgus extension overload test.6 Dissection is carried down to the level of the forearm fascia and the flexor-pronator aponeurosis (Fig. 46-1). We prefer the muscle-splitting approach7 for exposure of the UCL. A fascial raphe can usually be identified in the flexor-pronator mass at the junction of the anterior two thirds and posterior third of the muscle group. This raphe represents an internervous plane between the median nerve–innervated palmaris longus and deeper flexor digitorum superficialis and the ulnar nerve–innervated flexor carpi ulnaris. The fascia is split through the raphe from the medial epicondyle to a point approximately 1 cm distal to the sublime tubercle. The sublime tubercle can be palpated deep under the flexor mass. More distal dissection risks denervation of the surrounding musculature from crossing nerve branches. The muscle is then bluntly divided down to the level of the underlying UCL (Fig. 46-2). Care is taken during the split and division of the muscle because the ulnar nerve lies just posterior to the approach. A blunt self-retainer is used to retract the musculature, and a small periosteal elevator can be used to clean any remaining muscle fibers from the UCL. The UCL is thoroughly inspected for tearing and overall tissue quality. The humeral and ulnar insertions are carefully evaluated based on preoperative imaging (Fig. 46-3). After external inspection of the ligament, a longitudinal incision is made in the direction of its fibers to assess undersurface tears and degeneration. If the ligament is found to have midsubstance tearing, significant degeneration, or poor tissue quality, a reconstruction should be performed instead of repair. For humeral avulsions, the native ligament insertion site is gently prepared with a small rongeur. A small double-loaded suture anchor is placed at the apex of the V junction of the trochlea and medial epicondyle as described by Savoie and colleagues3 (Fig. 46-4A). Currently we use 2.9-mm Bioraptor suture anchors (Smith & Nephew Endoscopy, Andover, MA). Both sets of sutures are placed in horizontal mattress fashion in the proximal ligament and tied (Fig. 46-4B). Similarly, for ulnar avulsions the sublime tubercle is gently prepared with a small rongeur. A double-loaded anchor is placed into the sublime tubercle, and both sets of sutures are passed in mattress fashion in the most distal aspect of healthy ligament and tied. There are limited reports in the literature regarding outcomes after UCL repair (Table 46-1), especially in comparison to results after UCL reconstruction. Several reports detailing results after UCL reconstruction have included small numbers of patients treated with repair.8,9 In the largest series to date, Savoie and colleagues3 reported on 60 patients with a mean age of 17.2 years who underwent repair of the UCL and were followed for an average of 59 months after surgery. Based on the Andrews-Carson rating, good to excellent results were found in 93% of patients, and 58 patients were able to return to the same or a higher level of sport. The results of UCL repair are best measured by the athlete’s return to sport. 1. Callaway, GH, Field, LD, Deng, XH, et al. Biomechanical evaluation of the medial collateral ligament of the elbow. J Bone Joint Surg Am. 1997;79:1223–1231. 2. Richard, MJ, Aldridge, JM, 3rd., Wiesler, ER, et al. Traumatic valgus instability of the elbow: pathoanatomy and results of direct repair. J Bone Joint Surg Am. 2008;90:2416–2422. 3. Savoie, FH, 3rd., Trenhaile, SW, Roberts, J, et al. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36:1066–1072. 4. Veltri, DM, O’Brien, SJ, Field, LD, et al. The milking maneuver: a new test to evaluate the MCL of the elbow in the throwing athlete [abstract]. J Shoulder Elbow Surg. 1995;4:S10. 5. O’Driscoll, SW, Lawton, RL, Smith, AM. The “moving valgus stress test” for medial collateral ligament tears of the elbow. Am J Sports Med. 2005;33:231–239. 6. Andrews, JR, Whiteside, JA, Buettner, CM. Clinical evaluation of the elbow in throwers. Oper Tech Sports Med. 1996;4:77–83. 7. Smith, GR, Altchek, DW, Pagnani, MJ, et al. A muscle splitting approach to the ulnar collateral ligament of the elbow: neuroanatomy and operative technique. Am J Sports Med. 1996;24:575–580. 8. Azar, FM, Andrews, JR, Wilk, KE, et al. Operative treatment of ulnar collateral ligament injuries of the elbow in athletes. Am J Sports Med. 2000;28:16–23. 9. Conway, JE, Jobe, FW, Glousman, RE, et al. Medial instability of the elbow in throwing athletes: treatment by repair or reconstruction of the ulnar collateral ligament. J Bone Joint Surg Am. 1992;74:67–83. 10. Norwood, LA, Shook, JA, Andrews, JR. Acute medial elbow ruptures. Am J Sports Med. 1981;9:16–19. Part 2 Docking Technique The anterior bundle of the ulnar collateral ligament (UCL) of the elbow is the primary restraint to valgus load. It has been well documented that throwing athletes are prone to injury of this structure secondary to the repetitive valgus loads to which the elbow is subjected with overhead pitching.1–6 Originally described in javelin throwers, this injury is almost exclusively seen in overhead throwing athletes, with baseball pitchers being the most prevalent group of patients. Injury to the UCL has also been shown in wrestlers, tennis players, professional football players, and arm wrestlers. Symptomatic valgus instability can arise in these athletes after a UCL injury, necessitating operative intervention.1–6 Although injury to the UCL in the nonthrowing athlete can have excellent results with nonoperative intervention, the overhead throwing athlete may find an injury to the UCL of the elbow to be a career-ending event if surgical intervention is not employed. The UCL complex is composed of an anterior bundle, a posterior bundle, and a transverse bundle7,8 (Fig. 46-5). The anterior bundle has been shown to be the primary restraint to valgus stress at the elbow. Injury to the anterior bundle can cause instability of the elbow with subsequent disabling pain in overhead throwing athletes. The humeral origin of both the anterior and the posterior bundles is the medial epicondyle. The anterior bundle originates from the anteroinferior aspect of the medial epicondyle and inserts at the sublime tubercle of the ulna. The posterior bundle is triangular, smaller, and fanlike in nature; it originates from the posteroinferior aspect of the medial epicondyle and attaches to the medial olecranon margin.7,8 The anterior bundle has separate bands that function as a cam, tightening in a reciprocal fashion as the elbow is flexed and extended. In a cadaveric study, Callaway and colleagues7 performed sequential cutting of the medial collateral ligament (MCL) while a valgus torque was applied. The anterior band of the anterior bundle was the primary restraint to valgus rotation at 30, 60, and 90 degrees of flexion. The posterior band of the anterior bundle was a co-primary restraint with the anterior band at 120 degrees.7 In a separate study, Field and colleagues9 evaluated the laxity seen with UCL injury when viewed through the arthroscope. They found that ulnohumeral joint opening was not visualized in any specimen until complete sectioning of the anterior bundle had been performed. However, only 1 to 2 mm of joint opening was present with complete transaction of the anterior bundle, emphasizing the subtle examination findings in these athletes. It was shown that the maximum amount of valgus laxity was seen best at 60 to 75 degrees of flexion. The flexor carpi ulnaris (FCU) is the predominant muscle overlying the UCL. It is the most posterior structure of the flexor-pronator mass, which places it directly overlying the anterior bundle of the UCL.8 Thus the FCU is optimally positioned to provide direct support to the UCL with regard to valgus stability. Preservation of the FCU is important during reconstruction of the UCL, to maintain one of the secondary restraints to valgus stress. This is further discussed later, when the surgical technique we currently use is described. History and Physical Examination In the evaluation of overhead athletes with medial-sided elbow complaints, it is important to first obtain a detailed history. Questions should be posed regarding the chronicity of the symptoms as well as their effect on overhead activity. Issues regarding velocity, accuracy, and stamina are important to the throwing athlete and should therefore be addressed. It is important to note that many of these athletes will modify their pitching techniques to compensate for the pain; however, these athletes will not be able to reach their maximal throwing velocity secondary to the altered mechanics being implemented. The phase of throwing in which the pain occurs is another important aspect. Conway and colleagues2 have shown that nearly 85% of athletes with medial elbow instability report discomfort during the acceleration phase of throwing, in contrast to less than 25% of athletes who will experience pain during the deceleration phase. This same study also showed that up to 40% of patients with MCL injuries may also have ulnar neuritis; therefore a history of ulnar nerve symptoms should be ascertained as well as information pertaining to the position in which these symptoms are most prevalent.2 Several tests for the UCL have been described. In general, we typically find the valgus stress test and the moving valgus stress test to be the most specific. To perform the valgus stress test, the examiner places the patient’s distal forearm under the axilla and applies a valgus load to the elbow in 30 degrees of flexion while palpating the MCL (Fig. 46-6). If the patient reports increased medial-sided elbow pain or if valgus instability is present, then the test result is considered positive. However, it must be noted that the amount of instability present in these patients is sometimes too small to be picked up by this maneuver. Therefore pain may be the only indication of a UCL injury with this test. The moving valgus stress test was originally described by O’Driscoll.10 This test is performed by applying a valgus stress to the elbow in the flexed position and then quickly extending the elbow (Fig. 46-7). A positive test result occurs when medial pain is produced, typically between 120 and 70 degrees of flexion, as a result of shear stress on the UCL. Finally, we also sometimes use the “milking maneuver,” which is performed by pulling on the patient’s thumb with the forearm supinated, the shoulder extended, and the elbow flexed to 90 degrees. A feeling of instability and apprehension along with pain is a positive finding and indicates insufficiency of the posterior band of the anterior bundle. Plain radiographs remain the gold standard for initial evaluation of the elbow. Routine anteroposterior (AP), lateral, and oblique views should be obtained. These standard radiographic views may reveal calcifications in the UCL, medial spurs on the humerus and ulna at the joint line, spurs on the posterior olecranon tip, or loose bodies in the olecranon fossa (Fig. 46-8). Stress radiographs have been advocated to aid in the diagnosis of UCL tears, but we do not routinely use them. We recommend magnetic resonance imaging (MRI) for every patient with a suspected UCL tear. Both contrast and noncontrast MRI sequences can be used with success. When available, we use three-dimensional volumetric gradient echo and fast spin echo techniques, which enable thin-section (<3 mm) imaging of the elbow, thus improving visualization of partial tears of the UCL and obviating the need for contrast injection.11 Partial tears can be seen on MRI as areas of focal interruption that do not extend through the full thickness of the ligament. Complete tears can be seen on coronal MRI scans as increased signal intensity and focal disruption of the normally hypointense, vertically oriented ligament (Fig. 46-9). In chronic ligament injuries without tears, the UCL will appear thickened without focal discontinuity, but with global increased signal intensity. Because arthroscopic evaluation of the UCL is limited in its ability to visualize the anterior bundle and humeral or ulnar insertions, MRI is an effective technique for distinguishing ligament tears from flexor or pronator tendinopathy. Osteochondral impaction injuries to the radiocapitellar joint may also be seen, which emphasizes the importance of obtaining appropriate cartilage pulse sequencing. Early experience with MCL reconstruction at the Hospital for Special Surgery (HSS) led to some concerns about the original procedure as described by Jobe.2 These concerns included the ability to adequately tension the graft at the time of final fixation; potential complications from detachment of the flexor origin; potential complications from the placement of three large drill holes in a limited area on the epicondyle; complications from routine ulnar nerve transposition; and the strength of suture fixation of the free tendon graft. Therefore in 1996 the senior author (D.W.A.) began to look for alternative methods to reconstruct the UCL to address these concerns. The resulting procedure is referred to as the docking technique and highlights the following: use of a muscle splitting safe zone approach; avoidance of routine transposition of the ulnar nerve; reduction in the number of large drill holes from three to one in the medial epicondyle; and addressing of tendon length to ensure proper tensioning and fixation in bony tunnels.
Ulnar Collateral Ligament Repair and Reconstruction
Preoperative Considerations
Physical Examination
Surgical Technique
Specific Steps
1 Exposure
2 Ligament Assessment
3 Ligament Repair
Results
References
Biomechanics and Anatomy
Preoperative Considerations
Imaging
Development of the Docking Procedure
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Ulnar Collateral Ligament Repair and Reconstruction