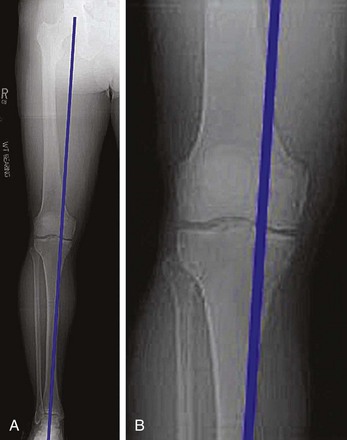
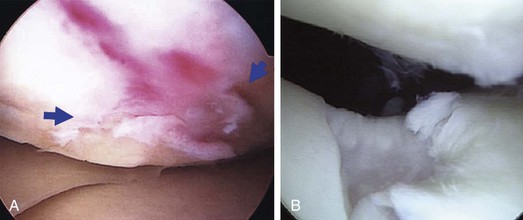
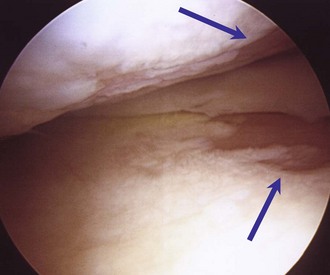
Chapter 69 Articular cartilage defects are often seen during knee arthroscopy and are noted on magnetic resonance imaging (MRI) with relative frequency in young athletes.1,2 When the defects are symptomatic, they can cause disability comparable with that associated with advanced knee osteoarthritis.3 Despite the frequency of articular cartilage injury, methods for treatment of the cartilaginous lesions did not produce good long-term results until the development of the technique by Peterson and colleagues of autologous chondrocyte implantation (ACI), first reported in 1994, which has gained a major role in the treatment of large full-thickness chondral injuries.4 Results are now available with up to 20 years of follow-up, and more than 75% of the patients have had improvement with relatively minor complications.4–11 In this technique, a small biopsy specimen of healthy chondral tissue is obtained arthroscopically; this specimen then undergoes in vitro chondrocyte amplification in cell culture, returning autologous chondrocyte cells available for implantation into the defect at the second stage of the repair procedure. The goal with use of autologous chondrocytes is to produce a repair tissue that more closely resembles the morphologic characteristics of the type II hyaline cartilage, thus restoring the durability and natural function of the knee joint.4,12,13 To adequately evaluate a patient for any cartilage treatment including ACI, it is imperative that weight-bearing anteroposterior (AP) and 45-degree posteroanterior (PA) views be obtained. In addition, patellar alignment radiographs should be obtained with lateral and sunrise views. This allows evaluation of the alignment of the tibiofemoral and patellofemoral portions of the knee and gives an indication of any underlying bone involvement associated with the defect. A long-leg limb alignment radiographic view should be used to assess the mechanical axis and determine the potential need for realignment (Fig. 69-1). The greater availability of office-based digital imaging has made obtaining these long-limb alignment views very practical. As mentioned, MRI can then be used to assess for the presence of both ligamentous injury and damage to the menisci, as well as to define the degree of subchondral bone involvement. Increased signal and edema of a chronic nature in the subchondral bone may indicate persistent overload of the involved compartment and may indicate the need for a realignment procedure in addition to ACI. Bone loss of more than 7 to 8 mm in depth necessitates bone grafting before or at the time of cell implantation. Although MRI is helpful to evaluate subchondral bone loss and the soft tissues of the knee, owing to the wide variations in magnetic resonance field strengths and imaging protocols, at present it does not have consistent sensitivity or specificity to evaluate the full extent of chondral injury or other, more subtle changes to the cartilage. ACI is indicated for symptomatic, full-thickness chondral lesions and osteochondritis dissecans (OCD) lesions of the femoral condyles and trochlea in physiologically young patients (aged 15 to 55 years) who can be compliant with the rehabilitation protocol (Fig. 69-2). Results of treatment of chondral injuries of the patella with ACI have become much more consistently favorable with realignment and appropriate patellar tracking. ACI is not indicated as a treatment for advanced osteoarthritis or in the presence of bipolar sclerotic bone-on-bone lesions (Fig. 69-3). ACI is also contraindicated in active inflammatory arthritis or infection. In summary, the prerequisites for a successful outcome in treatment of a full-thickness focal chondral defect with ACI include appropriate bony alignment, ligamentous stability, meniscal function, adequate motion and muscle strength, and patient compliance without significant arthritic changes.
Autologous Chondrocyte Implantation in the Knee
Preoperative Considerations
Imaging
Indications and Contraindications4,5,8,14,15
Musculoskeletal Key
Fastest Musculoskeletal Insight Engine