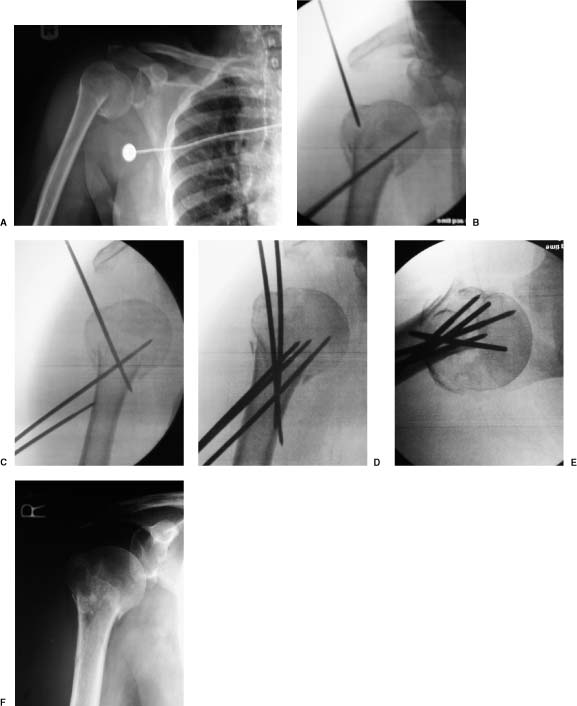
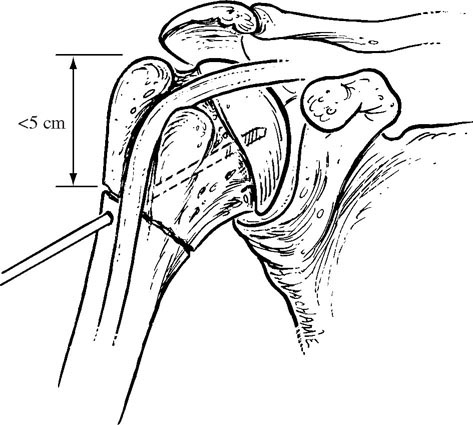
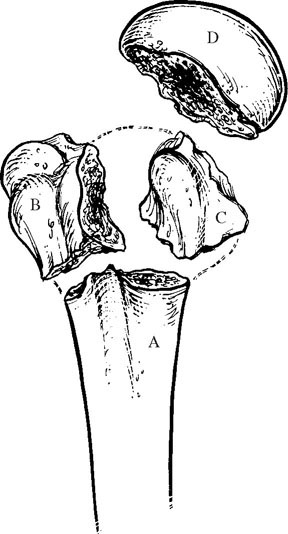
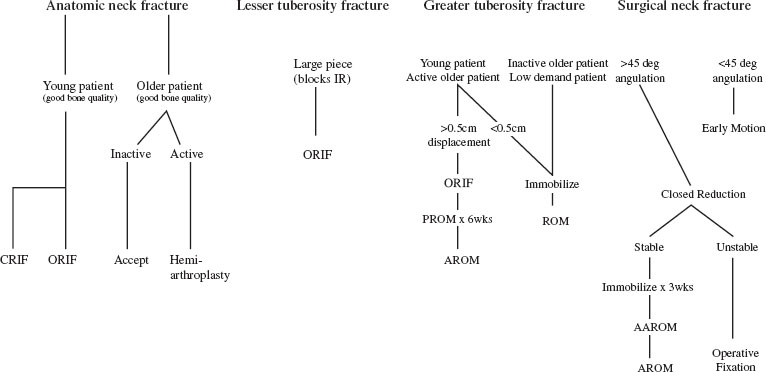
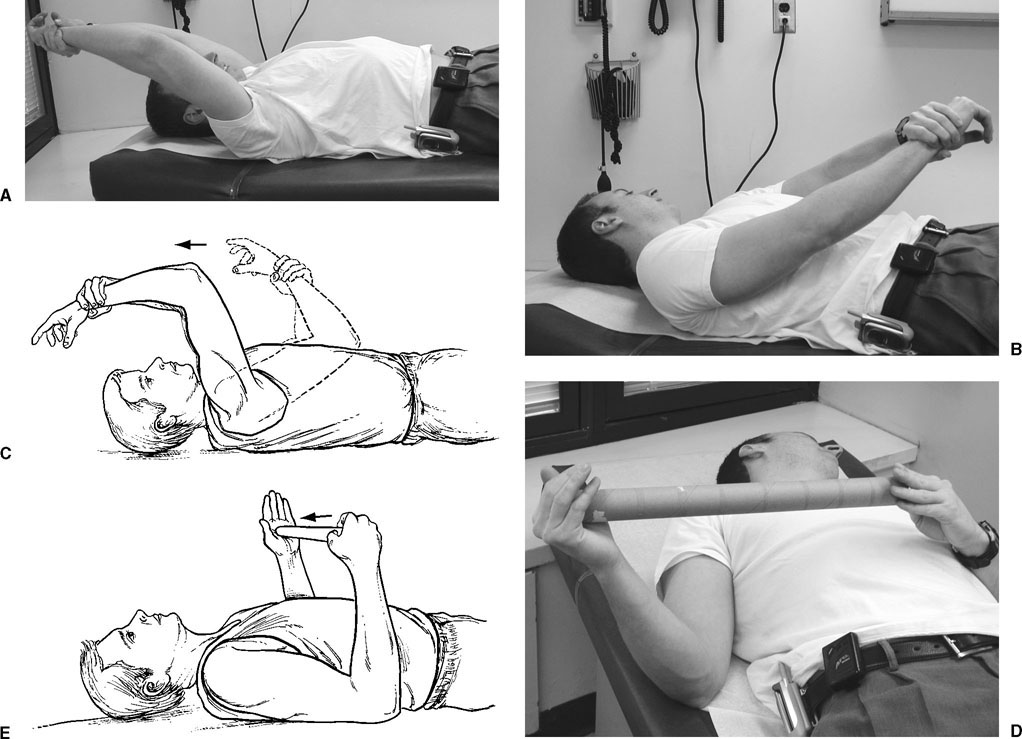
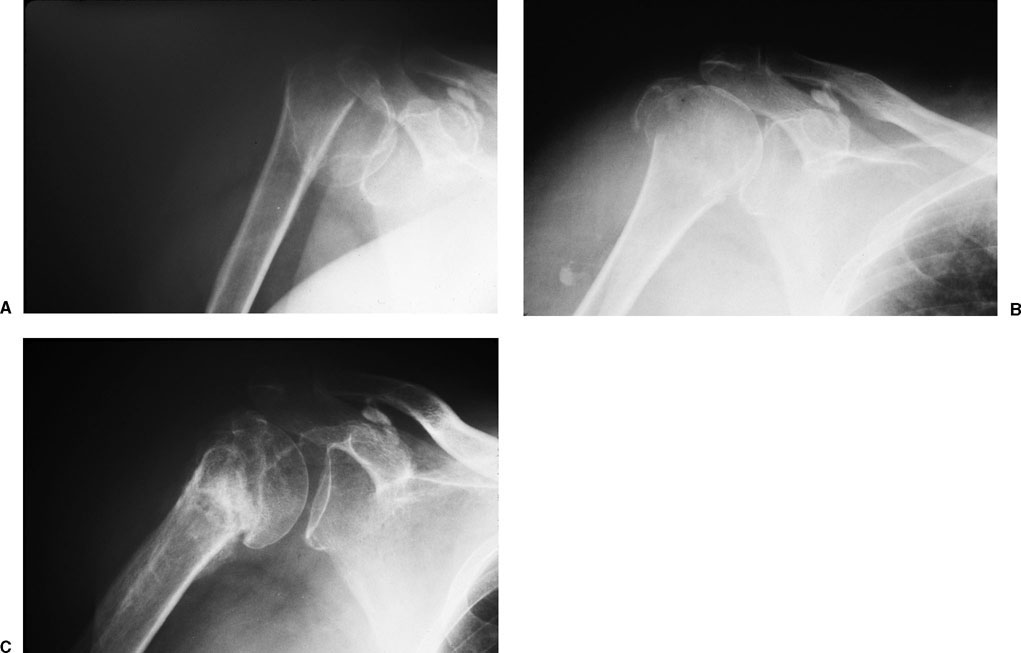
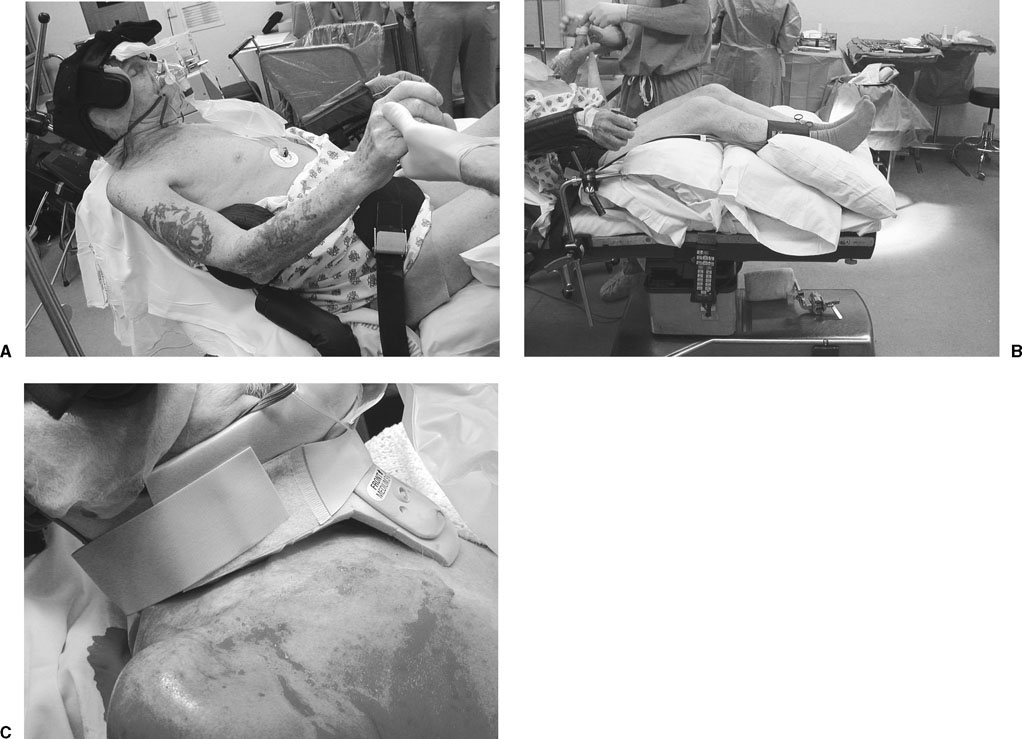
Proximal humerus fractures are most commonly classified according to the number of parts.1,2 According to Neer, a part is defined as a fracture fragment that is at least 45° angulated or 1 cm displaced. Fragments include the humeral shaft, humeral head, greater tuberosity, and lesser tuberosity (Fig. 5-1).1–3 Two-part fractures occur when one of the four fragments fulfills the displacement criteria. All two-part fractures may be accompanied by a concomitant dislocation. Displacement of fragments is influenced by the muscular attachments.1,4 The most commonly displaced two-part fractures are those of the surgical neck.1,5 With a surgical neck fracture, the humeral shaft is displaced anteriorly and medially secondary to the influence of the pectoralis major. The humeral head (with its attached tuberosities) remains in neutral position due to the balanced pull of the rotator cuff. When there is a greater tuberosity fracture, the attached supraspinatus, infraspinatus, and teres minor retract the greater tuberosity posteriorly and superiorly. In a two-part lesser tuberosity fracture, displacement of the lesser tuberosity occurs medially due to the influence of the subscapularis. The majority of patients who sustain two-part fractures are in the older age group.1,6–8 Osteoporosis and sedentary lifestyle frequently play a role by increasing the susceptibility of the proximal humerus to relatively minor trauma. Fractures in the younger age groups are more often a result of higher energy trauma.8–11 The majority of two-part fractures are primarily surgical neck fractures occurring in patients older than 65 years.12–14 Isolated greater tuberosity fractures are responsible for less than 2% of all proximal humerus fractures,12 although this incidence may be underreported.15 Two-part anatomic neck fractures and two-part lesser tuberosity fractures account for less than 1% of two-part fractures. Greater tuberosity fractures have been cited as occurring 5 to 33% of the time in association with anterior dislocations.16–18 Lesser tuberosity fractures also occur in association with posterior dislocations.12 This chapter focuses on the clinical and radiographic evaluations and treatment of two-part fractures and fracture dislocations. After determining the patient’s chief complaint, clinical evaluation should proceed with an account of the events leading to injury. The mechanism can be either direct (i.e., a lateral blow to the shoulder) or indirect (i.e., fall on an outstretched hand, electroconvulsive therapy, seizure, etc.). The indirect mechanism often results in greater fracture displacement than the direct mechanisms.19 Indirect mechanisms are also responsible for fracture-dislocations, often in the younger population.19 A loss of consciousness or other constitutional symptoms should alert the clinician to a possible underlying medical condition, especially in the elderly.19 Patients usually complain of shoulder pain with tenderness to palpation and limited range of shoulder motion. Crepitus may be appreciated when attempting to actively or passively range the shoulder. Ecchymosis may be present and can extend distally. A detailed neurovascular examination is essential, as with all orthopaedic injuries. A careful, sensory examination is necessary to delineate the location of potential nerve injury.20 With proximal humerus fractures, up to a 45% incidence of nerve injury has been reported. This most commonly occurs with surgical neck fractures and fracture-dislocations.21 Older patients and those with clinical evidence of hematoma have an increased risk of nerve injury. The axillary nerve is most commonly involved, followed by the suprascapular, radial, and musculocutaneous nerves. Fortunately, the majority of nerve injuries are neuropraxias from low-energy trauma and resolve within 4 months.22 FIGURE 5-1 The four parts of the proximal humerus. A, humeral shaft; B, greater tuberosity; C, lesser tuberosity; D, articular segment. Although the axillary artery lies just anteromedial to the proximal humerus,23 the incidence of vascular injury in association with two-part fractures is very small. In two studies reporting a total of more than 300 patients, there were no cases of vascular complications in association with proximal humeral fractures.2,24 The proximity of vascular structures and risk of injury is greater with high-energy fractures and fracture-dislocations, particularly with significant medial displacement. With a pure anterior dislocation, damage can occur at the thoracoacromial, subscapular, or circumflex humeral trunks.25 Suspicion of injury should be high in the presence of an expanding hematoma, absent distal pulses, a cold extremity, and a pulsatile painful mass with a bruit.26 Because there is extensive collateral flow in the shoulder, pulses may be palpable in up to 27% of cases with an axillary artery injury.27 A Doppler exam and arteriogram should therefore be performed whenever an arterial injury is suspected.28,29 When a vascular injury is present, the sequence of bone and arterial repair is controversial and is usually based on the degree of ischemia present.28,30 Careful assessment of fracture stability is required. Motion through the distal fragment should be evaluated to determine if the fracture moves as a unit. Also, any abnormal contours, such as a fullness or concavity, either anteriorly or posteriorly, should increase the suspicion for an associated glenohumeral dislocation. Radiographic evaluation of the injury requires the trauma series: anteroposterior (AP) and lateral shoulder views in the plane of the scapula and an axillary view. Classification and treatment is often influenced by the findings in each of these views. The scapula AP can delineate fracture fragment angulation, alignment, and displacement.21,31–34 The scapula lateral is particularly helpful in evaluating shaft displacement and glenohumeral joint orientation, and in visualizing posteriorly displaced fragments. An axillary view provides information about displacement of the tuberosities, associated dislocations, and humeral head impression fractures often seen with fracture-dislocations.27,35–39 When patients are in too much pain to be removed from a sling, the Velpeau axillary view can be obtained by having the patient lean backward 30° over the x-ray table. An x-ray cassette is placed beneath the shoulder and the beam is directed from superiorly to inferiorly, through the glenohumeral joint.32 Computed tomography (CT) scans may be of assistance if the trauma series radiographs are indeterminate and with fracture-dislocations.21,39,40 Fragment rotation, tuberosity displacement, head impression fractures, and head-splitting components can be further delineated with CT scans.21 Although CT scans may clarify certain injuries, their effect on intraobserver reliability and interobserver reproducibility for classification of injuries has been questioned.41 Bernstein et al41 found that the addition of CT scans to plain radiography increased the kappa coefficient for intraobserver reliability from 0.64 (plain radiographs) to 0.72 (plain radiographs and CT scan) but had no effect on interobserver reliability. Additionally, magnetic resonance imaging (MRI) can aid with defining associated soft tissue injuries of the rotator cuff, biceps tendon, and glenoid labrum, although it is uncommon for this information to have a significant impact on the treatment plan selected. The decision to proceed with operative management is based on a careful consideration of patient and fracture factors, including the patient’s physiologic age, arm dominance, associated injuries, fracture pattern, degree of displacement, and bone quality; the decision is also based on the surgeon’s experience.27 Specific guidelines are discussed in the following sections for each fracture. An outline of the principles of treatment is described in the algorithm in Fig. 5-2. FIGURE 5-2 General algorithm for treatment of two part proximal humerus fractures. AAROM, active-assisted range of motion; AROM, active range of motion; CRIF, closed reduction and internal fixation; IR, internal fixation; ORIF, open reduction and internal fixation; PROM, passive range of motion. With this fracture pattern, the tuberosities and humeral head are one fragment that remains neutral or slightly abducted while the humeral shaft displaces medially and anteriorly as a result of the pull of the pectoralis major. Approximately 22% of proximal humerus fractures are two-part surgical neck patterns.12 Patient age and functional status are important factors in determining treatment. Impacted surgical neck fractures with angulation that approaches or even exceeds 45° can be considered for nonoperative management with institution of an early range-of-motion program. If the examination confirms the fracture is stable, it may be reasonable to accept the angulation in patients whose activities will not be adversely affected. These will usually be older, more sedentary individuals who do not require frequent overhead use of the involved extremity. Although it is true that significant angulation limits forward elevation, there are patients in whom the potential limitations will not have a significant impact on function. Selecting these patients requires a careful assessment of functional needs and treatment expectations. For these selected patients, treatment consists of sling immobilization for approximately 4 to 5 weeks until fracture healing has progressed. Range-of-motion exercises should be initiated as early as patient comfort allows. It is important for the exercises to be structured and supervised to avoid an aggressive approach that could displace the fracture site and interfere with healing. Active range of motion of the elbow, wrist, and hand, with the arm at the side, may begin immediately. Assisted range of motion of the shoulder can be started when the acute discomfort subsides, as can isometric deltoid exercises. Throughout the course of therapy, the patient is instructed to perform a home exercise program four times per day. To perform assisted flexion, the patient is instructed to lie supine and grasp the wrist of the injured extremity with the contralateral hand. Using the unaffected extremity, the injured arm is pulled up and overhead; that is, forward elevation (Figs. 5-3A-C). For assisted external rotation, the patient lies supine with arms at the side and elbows flexed 90°. The patient places a stick or similar object into both hands and uses the uninvolved side to push the injured extremity into external rotation. It is then used in the opposite direction for internal rotation back to the chest (Fig. 5-3D,E). Isometric exercises promote muscle tone of the anterior, middle, and posterior portions of the deltoid, and can be performed as comfort allows. Isometric internal and external rotation exercises can be performed after 2 to 3 weeks as fracture healing progresses. At 4 to 6 weeks, therapy can progress to active range of motion, including forward elevation, external rotation out to the side, and internal rotation behind the back. More vigorous stretching can be initiated 8 to 10 weeks after fracture and resistive strengthening at about 12 weeks postinjury. FIGURE 5-3 Clinical photographs (A,B) and schematic (C) of assisted flexion exercise; and a clinical photograph (D) and schematic (E) of assisted external rotation exercise. Fractures with more than 45° of angulation or greater than 1 cm may require fracture reduction. The typical pattern of these fractures consists of varus and apex anterior angulation that could potentially limit forward elevation. Active patients with a high level of functional demands should undergo closed reduction to improve alignment. Closed reduction is most easily performed under regional or general anesthesia with the aid of fluoroscopy. Adduction of the distal fragment relaxes the pectoralis major. Gentle traction should be applied (to correct the angulation) combined with lateral displacement of the humeral shaft (to correct medial translation) as the humerus is flexed to 90°. In this position a gentle impacting force should be applied to the humerus to engage the two fragments into a stable position (Fig. 5-4). The fracture is then visualized using fluoroscopy, and stability is assessed. Posterior angulation is better tolerated than anterior or varus angulation, so an overcorrection of this nature may be acceptable.27 If the alignment is acceptable, Velpeau immobilization should be used for 2 to 3 weeks. At that time, if follow-up radiographs confirm the alignment, assisted range of motion can be instituted along with a sling. At 6 weeks the sling can be discontinued and active range of motion is started as described previously. Radiographs should be done weekly for the first 2 to 3 weeks to ensure maintenance of reduction. Eighty percent of the stable, reduced two-part fractures will heal by 6 weeks.42 At 12 weeks, strengthening exercises can begin. Closed treatment has yielded a high level of satisfactory or excellent results when reduction can be achieved and maintained. In a study of 80 patients, 81% had good or excellent results overall when treated by closed means.43 FIGURE 5-4 (A) Angulated surgical neck fracture underwent closed reduction (B). At 6-month follow-up, the fracture is healed in acceptable position (C). If reduction cannot be obtained or maintained, operative management should be considered. Treatment options include closed reduction with percutaneous pinning and open reduction and internal fixation (plate and screws, tension-band wiring, suturing, and/or intramedullary fixation).7,44–48 This approach is best utilized in patients with good bone stock and minimal comminution in which the fracture can be adequately reduced by closed manipulation.49 Up to 70% good or excellent results have been obtained when using this technique7; however, biomechanically pin fixation is less rigid than other fixation methods.50,51 The equipment necessary for this technique includes fluoroscopy, terminally threaded 2.5-mm pins, and a tissue protector for pin placement. The patient is placed on the operating table with the injured shoulder off the lateral aspect of the table. Prior to prepping and draping, fluoroscopy is positioned to confirm that adequate AP and axillary images can be obtained by moving the image around the patient. Closed reduction is attempted with longitudinal traction on the arm and laterally directed traction of the shaft (Fig. 5-5). Anterior angulation is corrected with traction and flexion of the humerus.7 While an assistant manually maintains the fracture reduction, the operating surgeon inserts the pins with either a retrograde (lateral, anterior, or anterolateral) or antegrade (superolateral) technique. It has been shown that multiplanar pin constructs in the proximal humerus optimize torsional stiffness, and placement of an antegrade greater tuberosity pin optimizes bending stiffness.51 Placing percutaneous pins superior to the deltoid insertion may help avoid injury to the radial nerve in the spiral groove. Retrograde pin placement requires the use of a soft tissue protector to avoid axillary nerve injury. When pinning retrograde, it is also important to avoid the biceps tendon while ensuring pin placement in both fracture fragments (the anteriorly located shaft and the posteromedially located head). Both goals can be accomplished by aiming pins from anterolateral to posteromedial. FIGURE 5-5 Patient positioning for percutaneous pinning procedure including fluoroscopy setup and reduction maneuver for closed percutaneous pinning. An initial retrograde anterolateral pin can be placed through a small puncture wound in the lateral aspect of the humeral shaft. Due to the humerus’s natural retroversion and posteromedial location of the head relative to the shaft, proper retrograde pin placement is performed from anterolateral to posteromedial directed toward the center of the humeral head. The initial pin is angled 45° to the shaft in the coronal plane and 30° to the shaft in the sagittal plane. Under fluoroscopic guidance, the pin is placed just beneath the subchondral bone without penetrating the articular surface. A second pin can be placed parallel (either superior or inferior) to the first. If adequate space exists, a third retrograde pin may begin more anteriorly to allow for wide pin placement within the head. Care must be taken to avoid the biceps tendon when placing this pin. Finally an antegrade superolateral to inferomedial pin may be placed. Other pins may be added for further stability if necessary (Fig. 5-6). All pins should be shortened to a subcutaneous position just under the skin. Multiplanar fluoroscopy should then be instituted, while moving the shoulder through a range of motion, to ensure that the fracture is adequately stabilized and that there are no pins violating the articular surface. A Velpeau dressing is applied and the arm is immobilized for 3 weeks. Patients are followed with weekly radiographs, to ensure that pin migration has not occurred. Formal therapy should not be started until the proximal pin(s) is removed. With clinical and radiographic evidence of healing, assisted range of motion is begun. The pins are usually removed 4 to 6 weeks after surgery. Care must be taken to avoid the axillary nerve, cephalic vein, biceps tendon, and the posterior humeral circumflex artery when performing this procedure. A cadaveric study has shown that all of these structures are located between 2 and 11 mm from the placement of the pins as described (Fig. 5-7).52 These authors recommended that lateral pins should be placed distal enough to avoid the axillary nerve, and the greater tuberosity pins should be placed with the arm in external rotation and directed to a point 20 mm from the inferior aspect of the humeral head.52 An alternative method of percutaneous fixation utilizes cannulated screws (Fig. 5-8). Patient positioning and fracture reduction are performed in a similar fashion to that described earlier; however, instead of placing a larger diameter pin, guidewires for 4.5-mm partially threaded cannulated screws are inserted to the level of the subchondral bone. Screw length can be determined in two ways. The depth gauge for the guidewire can be seated to the bone and confirmed under fluoroscopic visualization, or an equal-length guidewire can be placed alongside the protruding guidewire to the level of the bone. The area that does not overlap is then measured as the appropriate screw length. A 3.2-mm cannulated drill bit is inserted over the guidewire using a dull guide to protect the soft tissues. A partially threaded 4.5-mm cannulated screw is then inserted over the guidewire and the guidewire is removed. This is repeated for the other guidewires. After all screws have been placed, the shoulder is placed through a range of motion and visualized under fluoroscopic guidance to confirm appropriate hardware placement, fracture alignment, and stability of the construct (Fig. 5-8).53 This technique has the potential for earlier passive range of motion without waiting for selective pin removal as when percutaneous pins are used. A report on 19 patients treated with percutaneous cannulated screws for displaced proximal humerus fractures yielded 84% good or excellent results with a 93% union rate.53 When closed reduction is unsuccessful, open reduction with internal fixation should be considered. Success with plate and screw fixation has been reported.54–56 A series of 98 patient with either two- or three-part proximal humerus fractures yielded 76% good to excellent results when fixed with a T-plate.57 In a biomechanical study comparing 10 modes of internal fixation, the plate and screw fixation was shown to be the strongest construct for patients with or without osteopenic bone.58 Plate fixation, however, carries the risk of devascularizing the proximal fragment thereby increasing the risk of osteonecrosis.59,60 Osteonecrosis has been reported up to 3.5 years after injury in the proximal humerus.61,62 The most common complications after open reduction and plating include prominent hardware, loss of fixation, and osteonecrosis.62–65 FIGURE 5-6 (A) A 62-year-old woman sustained a two-part surgical neck fracture as a result of a fall. (B–E) Closed reduction was performed followed by pin placement. A retrograde pin is placed first to secure the head to the shaft followed by a second pin inserted from a superolateral to an inferomedial position to fix the nondisplaced greater tuberosity fragment. Additional threaded 2.5-mm Schantz pins are placed sequentially to enhance fixation. (F) Four months following pin removal, radiographs demonstrate a healed fracture with acceptable alignment. FIGURE 5-7 Pin placement should avoid neurovascular structures based on the described “safe zone.” Biomechanically, interfragmentary suture has been shown to be least effective in stabilizing proximal humeral fractures.58 The addition of intramedullary rods to a figure-of-eight interfragmentary construct significantly improved maximum resistance to load.58,66 This augmented fixation becomes even more important when there is existing comminution.67 Clinically, up to 71% good or excellent results with an average of 145° of elevation, 43° of external rotation, and internal rotation to T11 have been reported with the use of intramedullary rods combined with figure-of-eight tension band.67 FIGURE 5-8 Preoperative (A,B) and postoperative (C) radiographs of a displaced surgical neck fracture treated by closed percutaneous cannulated screw fixation. Locked intramedullary fixation has been used for the treatment of proximal humerus fractures. A biomechanical study comparing tension band wiring supplemented with Enders nails, plate and screws, and a locked intramedullary nail showed that the plate/screw construct and the locked intramedullary nail were superior to the tension band/Enders nail construct. There was no statistically significant difference in the stability provided by the locked intramedullary nail compared with the plate/screw construct.68
Two-Part Fractures and Fracture-Dislocations
 Clinical Evaluation
Clinical Evaluation
Radiographic/Imaging Studies
 Treatment
Treatment
 Two-Part Surgical Neck Fractures
Two-Part Surgical Neck Fractures
Closed Treatment without Reduction
Closed Treatment with Reduction
Surgical Reduction and Fixation
Closed Reduction and Percutaneous Pinning
Closed Reduction and Percutaneous Fixation with Cannulated Screws
Open Reduction and Internal Fixation

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree