CHAPTER 85 Tumors of the Spine
General Information
The spinal tumors may arise from local lesions occurring within or adjacent to the spinal column or from distant malignancies spreading to the spine or paraspinous tissues by hematogenous or lymphatic routes. Local involvement of the spine may result from primary tumors of bone, primary lesions arising in the spinal cord or its coverings, or contiguous spread of tumors of the paraspinous soft tissues and lymphatics. Metastatic disease may occur in the spine with almost any of the solid tumors of the body, with osseous malignancies of the appendicular skeleton, and with systemic lymphoreticular malignancies such as multiple myeloma and lymphoma. Metastatic tumors are far more common than primary lesions in the spine, accounting for 97% of all spinal column tumors. Patients with adenocarcinoma are especially prone to spinal metastases, with primaries from lung, breast, prostate, kidney, gastrointestinal tract, and thyroid making up the majority. It has been estimated that between 50% and 70% of patients with carcinoma will develop skeletal metastases before death, and this number may be as high as 85% for women with breast carcinoma.1 Primary tumors of the spine are rare, and for the most part their relative incidence reflects that seen in the skeleton in general. Some tumors (chordoma, osteoblastoma) do show a predilection for the spinal column, but these still make up a small proportion of all spinal tumors.
Symptoms
The clinical presentation usually provides clues that alert the physician to the presence of a spinal neoplasm. Pain and weakness are the most common presenting complaints. Pain is present in nearly 85% of patients including 20% who report radicular symptoms.2 At the time of initial evaluation more than 40% of patients have subjective complaints of weakness, and objective neurologic deficits can be identified in 35% of patients with benign tumors and 55% of patients with malignancies. A palpable mass is detectable in only 16% of patients.
Although back pain is an exceedingly common and nonspecific complaint, pain associated with neoplasia tends to be progressive and unrelenting and does not have such a close association with activity as does mechanical back pain. Pain at night is particularly worrisome. Pain symptoms may localize to a specific spinal segment and may be reproduced by pressure or percussion over the involved segment. Radicular symptoms are less common but are still frequently seen in patients with cervical or lumbar involvement. Radicular pain in the thoracic region may result in “girdle” pain forming a belt of dysesthesias and paresthesias circumferentially from the level of vertebral involvement. These radicular symptoms may mimic a herniated nucleus pulposus, leading to confusion in diagnosis and treatment. Pain from neoplasia, however, is unremitting, progressive, and not relieved by rest or recumbency.3
Pain may arise from one of a number of causes. Local tumor growth may expand the cortex of the vertebral body, resulting first in thinning and remodeling of the cortex and later in pathologic fracture and invasion of paravertebral soft tissues. As the cortex expands, the overlying periosteum is distorted and stretched, stimulating pain receptors in that tissue. Local tumor extension from a paravertebral mass or following fracture may compress or invade adjacent nerve roots, resulting in radicular symptoms of pain or paresthesias. Pathologic fracture resulting from extensive vertebral body destruction may produce acute pain symptoms similar to those seen in traumatic compression fractures. Fractures may also produce mechanical instability and subsequent pain. Finally, any of these causes of back pain may be associated with acute or chronic compression of the spinal cord or nerve roots, resulting in focal and radicular symptoms of pain, paraparesis, or paraplegia.4
Neurologic deficits are fairly common in patients presenting with spinal tumors; they are most common in rapidly expanding malignant lesions, but any slowly progressive, expansile neoplasm may produce a deficit if left alone long enough. Weakness, usually in the lower extremities, may become apparent months or years after the onset of pain and is rarely the first symptom seen. Nonetheless, up to 70% of patients will manifest clinical weakness by the time the correct diagnosis is made. To avoid this complication, the clinician should maintain a high index of suspicion for patients with persistent back or radicular pain, particularly those with a history of known systemic malignancies.5
Bowel and bladder dysfunction may develop before diagnosis in up to half of patients with cord compression.6 Patients with compression at the level of the conus medullaris may present with isolated sphincter dysfunction, but it is far more common to see associated lower extremity impairments. The neurologic assessment in these patients must include an evaluation of bladder function.
Imaging Techniques
Plain Radiographs
Plain roentgenograms should be the first test in any case where a neoplasm is suspected. Anteroposterior (AP) and lateral views of the involved vertebra can provide considerable information about the nature and behavior of the lesion and may be sufficient to identify some characteristic tumor types. Even when the specific tumor type is not implicated, the benign or malignant nature of the lesion may be deduced from the pattern of bony destruction. Geographic patterns of bone destruction suggest a slowly expanding lesion, typically benign; more rapidly growing tumors produce a moth-eaten appearance; highly malignant, aggressive lesions produce a permeative pattern of destruction.7 However, because radiographic evidence of bone destruction is not apparent until between 30% and 50% of the trabecular bone has been destroyed, early lesions may be hard to detect.8 Twenty-six percent of patients with spinal metastases will have occult lesions undetectable on plain radiographs.9
Bone Scan
99mTechnetium bone scans are commonly used to detect neoplastic disease of the musculoskeletal system. Their superior sensitivity makes them ideal to detect lesions in symptomatic patients with negative or equivocal radiographs. The ability to scan the entire body makes bone scans advantageous to determine the extent of dissemination in patients with known systemic disease and to define the most accessible lesion to biopsy in patients with an unknown primary malignancy. More recently, intraoperative bone scans (IOBSs) have been used for osteoid osteomas. These benign lesions of the spine can cause significant pain and spinal deformity in the pediatric population and are often surgically elusive. IOBSs have been shown to minimize the need for multiple surgical procedures to ensure complete resection. As such, IOBSs have been shown to be highly sensitive for lesion localization and verification of complete surgical extirpation.10 However, the main disadvantage of bone scans is their poor specificity because non-neoplastic pathology, most often osteoarthritis, can also cause focal areas of increased uptake. The addition of single photon emission computed tomography (SPECT), a recent technologic advancement, however, improves the predictive value of planar scans by better defining the anatomic location of uptake.11,12
Computed Tomography Imaging
With the advent of portable CT scanners, expanded use of intraoperative CT scanning for spinal surgery has been reported. Because CT scanning provides excellent visualization of osseous pathology, it can be extremely helpful in the evaluation of tumor resections during complex spinal operations.13
Magnetic Resonance Imaging
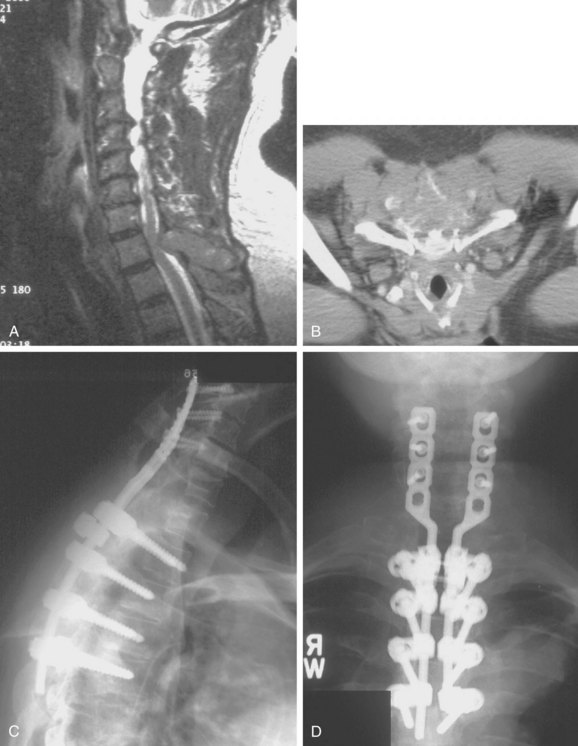
Because of its superior sensitivity and specificity, MRI has become the method of choice to evaluate the spine. It is well tolerated and safe with no exposure to radiation. MRI provides the best imaging of neural structures and can clearly define intramedullary, intradural, and extradural compressive lesions, as well as the extent of the lesion causing the compression, things that myelography cannot do (Fig. 85–1). The ability to obtain multiplanar images and to better delineate soft tissue structures make it invaluable in diagnosis and treatment planning. Whole spine MRI is also the best method to evaluate and direct treatment in a patient with suspected spinal cord compression and known malignancy.
MRI can detect neoplasms in the spine because normal marrow is replaced with tumor tissue with increased cellularity and extracellular water content.14 Thus most neoplasms have low signal intensity on T1 and high signal on T2. Fat suppression techniques combined with intravenous gadolinium further increase the contrast between normal fatty marrow and tumor tissue, making MRI the imaging technique with the earliest ability to detect neoplasm.15
These methods can also help to distinguish pathologic fracture due to osteoporosis versus malignancy. Malignant lesions usually have a more ill-defined margin, involvement of the pedicle, marked enhancement, and frequent paravertebral soft tissue extension while benign causes of vertebral compression usually still have fat present within the body, do not involve the pedicle, demonstrate more focal edema, and do not have an associated soft tissue mass.16,17 Infection can also be differentiated from neoplasm on MRI because infectious processes usually involve the disc space and endplate and incite a significant amount of edema. Neoplastic lesions are often more defined, do not involve the disc or endplates, and are associated with limited edema.14
Summary Imaging Appearance
The imaging appearance of primary bony tumors of the spine and simulating lesions of the spine has been described recently. There are specific imaging characteristics of benign and malignant lesions in the spine that can be described as follows. Benign bone tumors commonly appear as well circumscribed. As slow-growing lesions they may present with a calcified or sclerotic matrix. Malignancy on the other hand is often characterized by aggressive permeative lesions with bone destruction, cortical invasion, and associated soft tissue mass. CT may be helpful in characterization of the tumor matrix, exact location, extension and osseous changes, whereas MRI is superior for evaluation of the associated soft tissue mass, bone marrow infiltration, and intraspinal extension.18
Biopsy Techniques
The importance of a carefully planned biopsy cannot be overemphasized. Once the biopsy incision has been made, there are few choices left in planning the definitive tumor removal. When the surgeon selects an approach for biopsy, he or she is committed to that approach from thereon. The hazards of biopsy seen in musculoskeletal tumors of the extremities are doubly apparent in the axial skeleton. The incidence of inadequate or inappropriate biopsy that significantly alters a patient’s care is greater than one in three overall and probably higher in lesions of the spine.19 This risk is reduced significantly when the biopsy is performed by the treating, rather than the referring, physician.
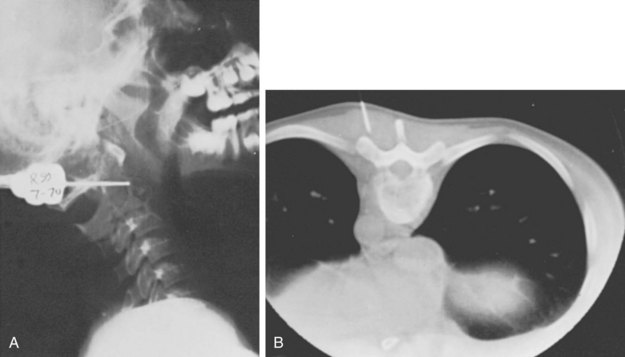
Three forms of biopsy are available to the surgeon: excisional, incisional, and needle biopsy or aspiration. On occasion a posterior lesion may prove suitable for an excisional biopsy, but most lesions of the spinal column will require either an incisional or needle biopsy. Needle biopsies are subject to sampling errors and provide a small specimen for evaluation (Fig. 85–2). The primary role of needle biopsy is confirmation—confirmation of metastatic disease, of recurrence of a known lesion, or of sarcomatous histology in an otherwise classic clinicoradiologic presentation of osteosarcoma.20 Culture results may also be obtained when infection must be ruled out.
The incisional biopsy should be the last step in the staging of the patient, performed just before the definitive surgical resection.21 A number of basic principles should be observed when performing the biopsy. The biopsy incision should be placed so that it may be excised with the tumor during the definitive procedure. Transverse incisions must be avoided, and the tumor approached in the most direct manner possible. Tissues should be handled carefully, and hemostasis should be meticulous so that hematoma does not carry tumor cells distant from the primary site. Bone should not be removed or windowed unless absolutely necessary. The specimen obtained should be large enough to allow histologic and ultrastructural analysis, as well as immunologic stains. The margin of the soft tissue mass is often most diagnostic because central portions are often necrotic. The surgeon should take care not to crush or distort the specimen, so as to maintain its architecture. If a soft tissue component exists, a frozen section should be obtained. Finally, if the definitive excision is to follow the biopsy under the same anesthetic, it is essential that all instruments used during the biopsy be discarded. The field should be redraped, and the surgeons should change gowns and gloves before the excision is begun. This same precaution should be followed in obtaining the bone graft for spinal reconstruction.
A recent review of the literature determined that the Weinstein-Boriani-Biagini tumor staging system accurately predicted the attainment of wide or marginal en bloc resection in 88% of cases.22 There was a clear increase in tumor recurrence when intralesional procedures were performed before the definitive en bloc resection. Tumor recurrence significantly shortened patient survival. Surgical complication rates ranged from 13% to 56%, and mortality ranged from 0% to 7.7%. The authors concluded that (1) incisional biopsy or intralesional resection significantly increases the risk of local recurrence. Therefore transcutaneous CT-guided trocar biopsy was recommended instead.
Tumors
Primary Tumors of Bone
Primary bone or soft tissue tumors arising in the spine are uncommon. In reviewing 82 primary neoplasms of the spine seen over a 50-year period at one center, 31 benign and 51 malignant lesions were identified, representing 8 benign and 9 malignant tumor types.2 All six cervical neoplasms in this series were benign, whereas two thirds of all thoracic, lumbar, and sacral primary tumors were malignant. Seventy-five percent of tumors found in the vertebral body were malignant, compared with only 35% of those in the posterior elements. For patients older than 18 years, 80% of primary tumors proved to be malignant but in children and adolescents only 32% of lesions were malignant. The 5-year survival in this series was 86% in patients with benign tumors and 24% in patients with malignancies.2 Bohlman’s review of 23 patients with primary neoplasms of the cervical spine also showed a marked difference in tumor type with patient age. In that series all patients younger than 21 years old had benign tumors, whereas 10 of 14 (71%) patients older than 21 had a malignancy.23
Benign
Osteochondroma
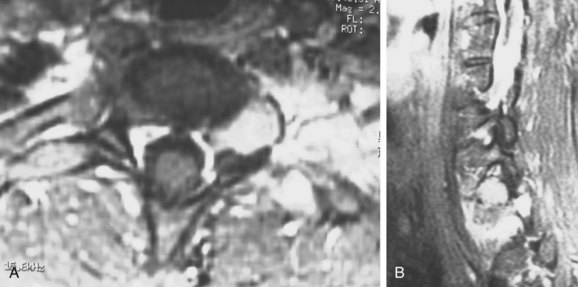
Although osteochondromas are the most common benign tumor of bone, only 3% occur in the spine in the solitary form and only slightly more in multiple osteochondromatosis.24 They are cartilage-capped bony projections arising from an abnormality in the perichondral ring. These lesions are usually asymptomatic in patients in the second and third decades of life, although patients may present with a painless mass. Rarely, patients may have neurologic compromise as a result of the lesion impinging on the canal or a nerve root. This scenario is more common in patients with multiple osteochondromatosis and in cervical lesions. Of osteochondromas presenting with spinal cord compression, 56% were in the cervical spine, 38% were thoracic, and 6% lumbar.25 Most of these lesions are not apparent on plain films. CT is usually necessary to determine the point of origin of the lesion, but MRI is necessary to define the cartilage cap and the proximity of the cord and other soft tissues. Because of the slow progression of the compressive cord lesion, excision of the tumor, en bloc or piecemeal, provides excellent recovery of neurologic function with little likelihood of recurrence (Fig. 85–3).
Although solitary spinal osteochondromas are uncommon lesions of the maturing adolescent skeleton, this lesion is much less common in older individuals. Only a few reports are available on osteochondromas in adults. In rare cases, lesions involving the spinal canal can cause low back pain and neurogenic claudication due to expansion of the lamina and extension into the spinal canal and adjacent facet joints.26 When treating osteochondroma in adolescents, one has to consider the possibility of recurrence if symptoms do not abate. This rare complication of recurrence has only been reported in three cases of cervical osteochondroma.27
Multiple hereditary exostoses with vertebral exostosis into the spinal canal are rare but must be considered if other skeletal lesions are present and multiple cervical exostotic lesions are found. This has been described in 68 of patients in whom exostoses arising from the spinal column have been described. Twenty percent of patients with multiple hereditary exostoses had lesions encroaching into the spinal canal. Patients with lesions inside the spinal canal were typically asymptomatic and neurologically normal, with radiographs that did not demonstrate the lesion. Compared with female patients, male patients were more likely to have spinal lesions and more likely to have lesions encroaching into the spinal canal (P = 0.014). Because of risk of neurologic injury, routine MRI to screen all patients with multiple hereditary exostoses has been recommended at least once during the growing years.28
Aggressive “Benign” Primary Spine Neoplasms
Osteoblastoma, Aneurysmal Bone Cyst, and Giant Cell Tumor
In order to define an improved clinical care plan for osteoblastoma, aneurysmal bone cyst, and giant cell tumor, these lesions have been grouped together in a category of “aggressive, benign, osseous neoplasms.”29 A panel of spine experts including oncologists, surgeons, and radiation oncologists graded the literature as either strong or weak. No prospective or randomized studies were found, reflecting the limited number of patients with aggressive primary osseous tumors. However, the osteoblastoma initial search identified 211 articles, of which 17 addressed spinal issues. The initial search for aneurysmal bone cysts revealed only 6 of 482 articles were pertinent, and only 8 of 178 articles on giant cell tumors focused on the treatment of spinal lesions. Authors found differences in clinical care but concluded that “surgical treatment should be directed at gross resection of the tumor, understanding that this may be limited by anatomic confines and the potential for morbidity.”
Osteoblastoma and Osteoid Osteoma
Osteoblastoma and osteoid osteoma are osteoblastic lesions differentiated primarily by size. These benign lesions show a propensity for spinal involvement, usually the posterior elements. Osteoid osteoma occurs in the spine in approximately 10% to 25% of cases, and osteoblastoma occurs in roughly 32% to 46% of cases.30–33 Patients usually present in their second or third decade, and the most common complaint is of back pain. The pain is typically persistent and unrelated to activity and often is most noticeable at night. Although aspirin classically provides dramatic relief of symptoms, this is not universal. Patients with osteoblastomas may have dull, achy pain typical of other benign lesions.
Painful scoliosis can be another presenting symptom. In a large review,34 78% of patients with osteoid osteoma and 54% of those with osteoblastoma were found to have scoliosis. The lesions were almost entirely on the concave side of the curve and were more commonly in the thoracic and lumbar rathern than cervical regions. The scoliosis is thought to result from muscle spasm on the side of the lesion. Most curves will improve or resolve after removing the lesion. This may not be the case, however, if the scoliosis has been present for a prolonged period of time.
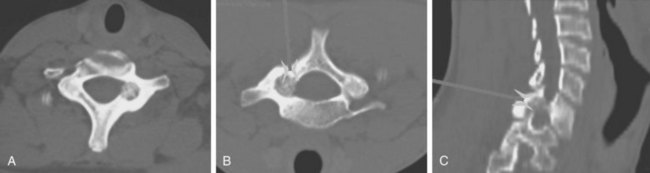
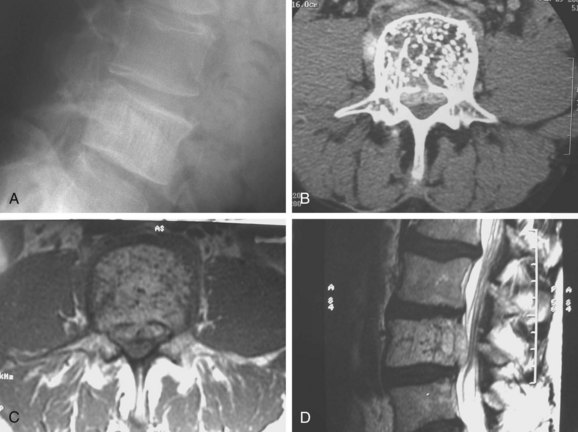
Radiographic demonstration of osteoid osteoma is difficult (Fig. 85–4). The lesion, by definition less than 2.0 cm in diameter, is easily obscured among the overlapping shadows of the vertebral column. CT demonstrates the lesion well, but if the cuts are at the wrong level or too wide, the tumor may be missed completely. The most sensitive method of locating an osteoid osteoma is by bone scan. The technetium bone scan provides accurate localization of the lesion, decreasing the average duration of symptoms by providing an early diagnosis and allowing prompt treatment.35
Osteoblastomas become considerably larger than osteoid osteomas and may be quite apparent on plain radiographs. The lesion is characterized radiographically by the expansion of the cortical bone, maintaining a thin rim of reactive bone between the lesion and the surrounding soft tissue. There is often a rim of reactive bone separating the tumor from the rest of the medullary bone. Although the tumor may show stippling in some cases, there is rarely if ever a lobulated or soap-bubble appearance to these lesions.32 When involvement of the vertebral body is seen, it is limited and results from extension of tumor into the body from the pedicle (Fig. 85–5).
MRI appearance of osteoblastoma is characterized by the localized inflammatory response the tumor causes. These inflammatory features can simulate malignant behavior on MRI, and an aggressive resection could be prompted for an otherwise benign lesion. Therefore it is critical to corroborate MRI findings, with other imaging and clinical data. Osteoblastoma is characterized by classic benign features on CT. In a recently reported case, a lumbar MRI revealed a sacral tumor with malignant features of marrow edema and enhancement, whereas a CT showed a well-circumscribed lesion without lytic changes or malignant bone formation.36 A conservative resection was performed, and histopathology confirmed the diagnosis of osteoblastoma. The authors concluded that the MRI findings for osteoblastoma can be misleading and cautioned that CT should be used when evaluating benign tumors with known inflammatory responses on MRI.
The treatment for both osteoblastoma and osteoid osteoma is by excision. Excision provides reliable pain relief, and the spinal deformity is improved or disappears in the majority of patients.30,37 Although a complete excision is desirable, it is not always feasible in the spine. Curettage and bone grafting of vertebral osteoblastomas have provided satisfactory long-term results in the vast majority of cases.32,37 Intraoperative CT guidance or preoperative CT localization may aid in complete resection of these lesions with the least amount of destruction to normal tissues. Osteoid osteomas in particular are treated commonly in other areas of the body with radiofrequency ablation. Although concern for thermal damage to neural structures is quite valid, recent reports of its safe use in spinal lesions may lead to its careful use in this setting.38 In other instances, stereotactic guidance systems may be used to provide a precise excision through a minimally invasive approach.39
Aggressive osteoblastoma is another variant of osteoblastoma. It is more aggressive and has higher recurrence rates and is considered to be a borderline or intermediate osteoblastic tumor. Although the true incidence and distribution of this rare tumor is not known, complete surgical excision by en bloc resection and spondylectomy is indicated because recurrence rates of 10% to 15% have been reported. Transformation to osteosarcoma has been reported and is associated with multiple recurrences. A recent article reported a rare case of recurrent aggressive osteoblastoma of the thoracic spine and accomplished successful treatment by total en bloc spondylectomy.40
Aneurysmal Bone Cyst
Aneurysmal bone cysts (ABCs) involving the spine are rare lesions that may be found at any level. They involve the posterior elements nearly 100% of the time (Fig. 85–6), but they may also commonly extend into the vertebral body. These benign, highly vascular osseous lesions of unknown origin may present difficult diagnostic and therapeutic challenges.41,42 ABCs are often expansile lesions containing thin-walled, blood-filled cystic cavities that cause bone destruction and sometimes spinal deformity and neurologic compromise. ABCs occur mostly in children and young adults, and 75% of patients are younger than 20 years old at presentation. In the lumbar spine, vertebra plana as a result of an ABC has been described and the authors pointed out that an ABC should be considered in the differential diagnosis when vertebra plana is seen in pediatric patients.43

FIGURE 85–6 A-B, Plain anteroposterior and lateral radiographs of L4 tumor involving the left L4 transverse process and pedicle. Diagnosis was osteoblastoma with elements of aneurysmal bone cyst (solid ABC). C-D, Preoperative computed tomography and magnetic resonance imaging scans of lesion. E-F, Anterior posterior and lateral radiograph views after resection of tumor involving zones II, III, and IVA (see Fig. 85–12).
The treatment of spinal ABCs remains controversial according to the literature. Treatment options include simple curettage with bone grafting, complete excision, embolization, and radiation therapy. Reconstruction and stabilization of the spine may be warranted if deformity and instability are present. Preservation of neurologic function may dictate surgical management. Nonetheless, complete excision offers the best chance of cure and spinal decompression if neurologic deficits are present. Treatment strategy should be aimed at complete excision whenever possible. Aggressive intralesional curettage and bone grafting may have higher local recurrence rates than complete excision of the lesion.42 Instrumented fusion will be necessary if the lesion or surgical excision compromises the stability of the spine. Preoperative selective embolization is helpful, especially in larger lesions.44
More recently, selective arterial embolization with N-2-butyl cyanoacrylate has been described.45 The study population comprised 20 male and 16 female patients with an age range of 3.3 to 60.8 years.5 Nine lesions were localized in the appendicular skeleton (1 in the upper and 8 in the lower limb), 4 in the thoracic cage (1 rib lesion and 3 scapular lesions), 17 in the pelvis and 6 in the spine (1 thoracic and 5 sacral localizations). Of the 55 embolizations performed, only 1 embolization was necessary in 22 cases (61%), 2 were necessary in 9 cases (25%), and 3 were necessary in the remaining 5 patients (14%). In ninety-four percent of patients, treatment was found to be effective with follow-up ranging from 0.9 to 5 years. Only seven patients underwent surgery during the embolization study. The authors reported on three complications (5%)—two cases of skin necrosis and one case of transient paresis—and concluded that arterial embolization with cyanoacrylate was a viable treatment for aneurysmal bone cysts. They recommended embolization as a less invasive, lower-cost, easily repeated, simpler procedure than surgery and it does not preclude surgery later.45
In children, aneurysmal bone cysts may represent a particular challenge because fusion and stabilization with instrumentation are often avoided due to concerns over instability following future axial skeleton growth. Recently, two case reports of aneurysmal bone cyst in the cervical spine of children were published.46 They both demonstrated deeply involved lesions with extensive bone destruction. Both were treated aggressively with resection, fusion, and stabilization with instrumentation. Both patients were reported to have had an uncomplicated postoperative course. At 36- and 18-month follow-up, both patients had no cervical spine instability or recurrence of tumor. The authors concluded that treatment of aneurysmal bone cyst in the cervical spine is challenging when it occurs in close proximity to neural and vascular structures.
Hemangioma
Vertebral hemangiomas are common lesions, occurring in approximately 10% of all patients, but they are rarely symptomatic or of clinical importance. They usually occur in the vertebral body but can extend to the posterior elements. Reports of deformity or pain associated with vertebral hemangiomas are uncommon, but cases of nerve root and cord compression have been documented, predominantly in the thoracic region (Fig. 85–7).47 The diagnosis of vertebral body hemangioma can usually be made on plain radiographs, although cross-sectional imaging will provide more information about cord impingement or fracture. Plain films classically show prominent vertical striations produced by the abnormally thickened trabeculae of the involved vertebral body.
Occasionally, spinal osseous hemangioma can mimic metastasis of a malignant tumor. This has been reported recently in a 44-year-old woman where the lesion was located in the seventh cervical vertebra.48 On histopathologic examination the lesion showed reactive osteoid formation and nontypical osteolytic radiologic findings, strongly suggesting a metastatic process. This case report underlined the importance of including hemangioma into the differential diagnosis even if it is found in the cervical spine. Although hemangioma is rarely found in the cervical spine, treatment of supposedly malignant metastatic lesions could expose the patient to the risks of unneeded aggressive local and adjuvant treatments.
Spinal hemangiomas are radiosensitive and frequently respond to radiotherapy alone. Alternatively, ethanol injection into the lesion or traditional embolization are other minimally invasive methods of treatment, although careful technique is required.49 When cord compression develops and surgical treatment is considered,50 angiography is indicated to establish the vascular source for the tumor, to identify the primary vascular supply to the cord (the artery of Adamkiewicz), and for consideration of preoperative embolization. Smaller symptomatic lesions may be managed with vertebral augmentation. Recently, percutaneous treatment with vertebroplasty for aggressive and symptomatic vertebral hemangiomas has been reported in 24 patients.51 The authors reported the utility of vertebroplasty with good clinical results in all patients with pain relief within 24 to 72 hours even when epidural extension was present. They concluded that percutaneous vertebroplasty “is a valuable, mini-invasive, and quick method that allows a complete and enduring resolution of the painful vertebral symptoms without findings of fracture of a vertebral body adjacent or distant to the one treated.” Large destructive lesions occasionally require anterior reconstruction.
Giant Cell Tumor
Although rare reports of malignant giant cell tumors exist, the vast majority of these lesions are slow-growing, locally aggressive tumors that do not metastasize. Spinal involvement is usually seen in patients in their third and fourth decades, and symptoms may exist for many months before the patient sees a physician. Plain radiographs usually demonstrate an area of focal rarification, though some present with a more geographic lytic appearance and marginal sclerosis. Giant cell tumors are most commonly found in the vertebral body and may expand the surrounding cortical bone extensively as the tumor enlarges (Fig. 85–8). CT is especially important in the evaluation of these tumors preoperatively because complete resection is critical to the eradication of local disease. CT is also crucial in the early identification of recurrences and should be used in postoperative follow-up on a routine basis. Complete excision is the treatment of choice and should be attempted en bloc whenever feasible in the spine.
Giant cell tumors involving the spine have a poorer prognosis than extremity lesions due to their locally invasive nature and the difficulty in obtaining a wide margin. This results in high local recurrence rates.2,52 Adjuvant treatment with radiation therapy was associated with unacceptably high rates of postirradiation sarcoma, often leading to the patient’s death. Recent reports have demonstrated favorable responses using megavoltage radiation therapy with low or no risk of radiation-induced sarcoma.53,54 With more aggressive surgical resection, radiotherapy is unnecessary and good disease-free survivals have been obtained without the risks of irradiation (Fig. 85–9).52,55

FIGURE 85–9 A, Giant cell tumor at T12. B, Lateral view radiograph 5 years after total vertebrectomy with no recurrence.
A series of 22 consecutive giant cell tumors (GCTs) of the cervical spine reviewed56 the clinical patterns and follow-up data of GCT arising in the cervical spine, correlating treatment and outcomes over time.1 Patients underwent surgical treatment from 1990-2003. The choice of surgical intervention was based on the Weinstein-Boriani-Biagini tumor staging system. The authors employed two different protocols of surgical treatment: Eight patients underwent subtotal resection, there were 13 cases of total spondylectomy, and one additional patient had en bloc resection for a lesion in the posterior element of C7. Spinal reconstruction was done with autograft and anterior instrumented fusion or anterior and posterior combined instrumented fusion. Eighteen patients received postoperative adjunctive therapies. Twenty-one patients were available for mid- and long-term follow-up (average of 67.8 months, ranging from 36 to 124 months). They reported satisfactory neurologic recovery, and fusion rates were 100%. The local recurrence rate was 71.4% in patients who underwent subtotal resection but only 7.7% for total spondylectomy. Four patients died within follow-up, and all of these deaths were in recurrent cases. One patient developed pulmonary metastases. The authors recommended strictly en bloc resection but recognized that it is often not a feasible option in the cervical spine because of the involvement of critical neurovascular structures.
Eosinophilic Granuloma
Eosinophilic granuloma is a benign, self-limiting condition that produces focal destruction of bone. A process of unproven etiology, eosinophilic granuloma is most commonly seen in children before the age of 10 years, when treatment can be challenging because preservation of neurologic function is of imminent concern.57 It can, however, occur in the adult spine as well, where it may present with local osteolysis.58 Lesions of the skull are most common, but any bone may be affected; vertebral involvement occurs in approximately 10% to 15% of cases. Spinal involvement can be seen in any of the triad of syndromes in which the disease manifests itself—isolated eosinophilic granuloma; the multifocal, chronic, and disseminated form, Hand-Schuller-Christian disease; or the acute disseminated or infantile form, Letterer-Siwe disease. The vertebral body is typically involved, usually in the thoracic or lumbar spine. Patients usually present with pain, focal spasm (torticollis is common in cervical lesions), and mild to moderate kyphosis. Neurologic compromise develops in a significant number of patients and may be severe.
Early in the disease process radiographs show a central lytic lesion with poorly defined margins and permeative bone destruction. At this point the lesion may produce a marked periosteal reaction, and distinguishing it from osteomyelitis or Ewing sarcoma may be impossible. As the vertebral body collapses and settles, radiographs demonstrate the flattened disc of dense cortical bone retained between the two intact intervertebral discs. This “coin-on-end” appearance of vertebra plana (Fig. 85–10) is a classic finding in eosinophilic granuloma but is not pathopneumonic; a similar appearance can be produced by either infection or high-grade sarcoma. With such a broad differential, the importance of obtaining an adequate biopsy specimen before beginning treatment cannot be overstated.59
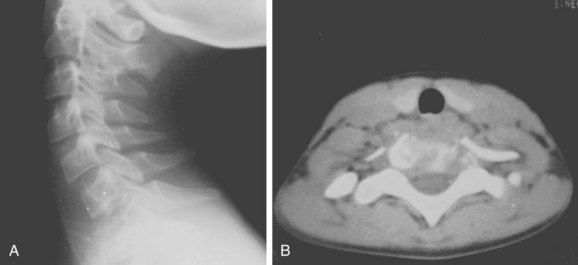
FIGURE 85–10 A, Lateral radiograph view of eosinophilic granuloma at C7. B, Computed tomography scan.
The treatment of eosinophilic granuloma is somewhat controversial, but it is clear that many patients will heal their lesions without any treatment other than biopsy, often reconstituting much vertebral height.60 Low-dose radiotherapy (500 to 1000 rads) has been advocated in the past, but this may be avoided in most patients. In those who present with a neurologic deficit, the established course of biopsy followed by irradiation and immobilization remains the most widely accepted.61
A retrospective case review of seven children with eosinophilic granuloma of the cervical spine identified therapeutic goals as spinal stability, preservation of neurologic function, and relief of pain, while keeping in mind that patients are still growing.57 There were five boys and two girls (mean age: 10 years; range 4 to 16) with a mean follow-up of 19 years (range 8 to 29). The symptoms at presentation varied according to the localization of the tumor and treatment varied from observation alone, prolonged immobilization, systemic chemotherapy, curettage with or without bone grafting, corticosteroid injection, and low-dose radiation therapy depending on the severity of clinical presentation. The authors recommended surgery for a child presenting with neurologic involvement. On the basis of their experience, they concluded that children with vertebral interbody fusion can show normal alignment of the neck and maintain normal motion at long-term follow-up.
Malignant
Osteosarcoma
Approximately 2% of all primary osteogenic sarcomas arise in the spine, 95% from the anterior elements. Patients present with pain and often with neurologic compromise. A palpable mass may be a late finding. Metastatic lesions are also commonly present on diagnosis. Vertebral osteosarcoma (especially in the sacrum) is frequently secondary to previous Paget disease or radiation therapy, in which case prognosis is even more grim.5,62,63 The radiographic findings include both lytic and sclerotic lesions, with cortical destruction, soft tissue calcification, and collapse in advanced cases. CT and MRI demonstrate intraspinal and paraspinal soft tissue masses more clearly, allowing more accurate preoperative planning.
Treatment of lesions in the spinal column is usually difficult, and the outcome in these tumors has traditionally been poor. Therapy consisting of limited tumor excision and radiotherapy provided median survival ranging from 6 to 10 months.5,62 In hopes of improving survival in this and other spinal malignancies, a more aggressive surgical approach has been advocated in recent years. For osteosarcoma, this has resulted in longer survival times and some cures.2,63–65
A systematic review of the literature and consensus recommendations by an international expert focus group has recently reviewed and classified “evidence in the literature regarding (1) the role of neoadjuvant chemotherapy and (2) impact of extent of surgical resection on clinical outcome, particularly survival and local control, in patients with spinal Ewing sarcoma (ES) and osteosarcoma (OS).” This study revealed moderate-level evidence suggesting that neoadjuvant chemotherapy offers significant improvements in local control and long-term survival in osteosarcoma of the spine. This multimodality management is essential in lieu of weak evidence suggesting that en bloc resection provides improved local control and potentially improved overall survival. Neoadjuvant therapy portends the most favorable local control and long-term survival. En bloc surgical resection may improve overall survival and decrease risk of recurrence.66
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree