11 Trochanteric Fractures
Intramedullary Devices
Intramedullary nailing was introduced in 1940 by Küntscher.1 He advanced the technique of closed intramedullary nailing by using an open section, straight, cloverleaf nail for femoral shaft fractures. Since the 1940s, intertrochanteric fractures have been treated with intramedullary nailing, and intramedullary fixation became standard treatment for femoral shaft fractures in the 1950s. In 1967, Zickel2,3 produced good results with intramedullary nailing for fixation of proximal femur fractures. Antegrade nailing became the standard fixation mode for these fracture types after the introduction of the Gamma nail in 1988, a trochanteric nail with an interlocking lag screw.4
Over the years, intramedullary fracture fixation became increasingly popular, and indications expanded to tibial and humeral shaft fractures. Since 1990, in response to advances in nailing systems, designs, and techniques, the indications for intramedullary fracture fixation have spread to the metaphyseal area of the long bones. Varying the distal and proximal screw positioning within the nail, the use of “Poller” screw techniques5 (using blocking screws to narrow the metaphyseal canal, for increased nail stability), and the availability of nails with percutaneous insertable interlocking screws have made intramedullary nailing the preferred treatment for diaphyseal and metaphyseal fractures in the proximal and distal third of the long bones.
Discussion is ongoing about extracapsular hip fracture treatment in terms of plate or nail preference. The rationale for plating intertrochanteric fractures may be explained by the widespread treatment of intracapsular hip fractures with a sliding hip screw (SHS) system: the technique is familiar. Another reason may relate to problems inherent in early cephalomedullary nail design for the proximal femur.6 Outcomes with the early cephalomedullary nails were not significantly better compared with hip screw outcomes, and the nails commonly produced complications such as femoral shaft fractures at the tips of short nails.7–9
Modern nail design and newer surgical techniques have made intramedullary nailing an increasingly attractive procedure for extramedullary hip fracture fixation.10 The biomechanical advantages of this approach have led to the development of various implants that represent the best current treatment for intertrochanteric fractures in a rising number of hospitals all over the world.
Rationale for Intramedullary Nailing of Extracapsular Hip Fractures
The need for intramedullary nailing fixation of intertrochanteric fractures becomes even more apparent when the effect of local forces is understood. High compressive forces along the medial cortex (Adams arch) and high tensile forces at the lateral cortex of more than 1000 psi create high biomechanical stress in the area of the proximal femur.11,12 The chosen implant must be adequately stable to maintain reduced fracture positioning until the fracture site is consolidated. In these cases, intramedullary nailing is clearly advantageous for fracture fixation. In biomechanical testing, intramedullary nails had greater stiffness and provided more rigid fixation with higher combined bending and compressive loads compared with plates.13 This effect is based on the design and location of the implant. Compared with extramedullary implants, intramedullary devices create a shorter lever arm because of their centered position in the shaft and subsequent position adjacent to the head-neck complex. The shorter lever arm results in decreased torque, which itself reduces the risk of mechanical failure until the fracture is completely consolidated.14
In comparison with extramedullary implants such as plates, intramedullary devices shift the weight-bearing axis and forces to the medial aspect of the proximal femur, with resulting load sharing.15–18 The main advantage of intramedullary fracture fixation in intertrochanteric fractures is the lateral buttress effect provided by the nail itself. The proximal part of the nail acts as an intramedullary brace in the greater trochanter. It provides stable fixation against medialization of the shaft and total collapse of the fracture fragments, fixation that cannot be provided by monocortical plating. This characteristic makes the use of extramedullary implants a suboptimal fracture fixation strategy in unstable and reverse oblique fractures (AO/OTA 31A3 fractures).19 In unstable and reverse oblique fracture types, extramedullary implants do not offer any additional fixation of the proximal fragment besides the lag screw. Unstable intertrochanteric fractures treated with the SHS or other extramedullary implants have significantly higher rates of malunion and shortening of the femoral neck and shaft.20,21 Because of these complications, many investigators have reported that the SHS and other extramedullary implants are not suitable for these fracture types.9,22–27 Based on the known biomechanical advantages of intramedullary nailing in treating femoral shaft fractures, newer-generation cephalomedullary nails have come into use for intertrochanteric fracture treatment.28–32
Indication and Fracture Types
According to the AO/Orthopaedic Trauma Association (OTA) classification, extracapsular hip fractures are classified as 31A fractures.33 Even though these injuries comprise a heterogeneous group of stable and unstable fractures with different mechanical characteristics, intramedullary nailing is indicated for all fractures types in this group. Type 31A fractures are subclassified into groups A1, A2 and A3, which can be further divided into subgroups.
AO/OTA 31A1
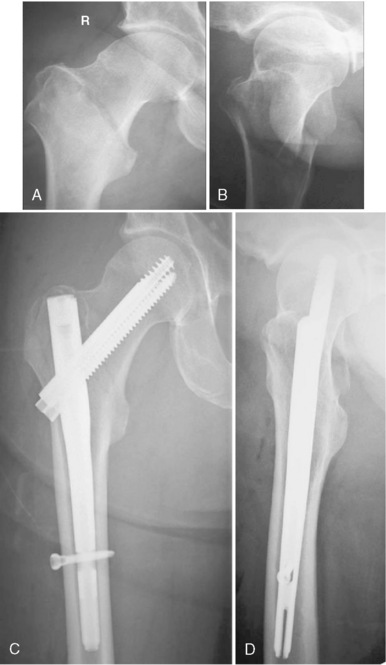
Type 31A1 fractures are simple pertrochanteric fractures with the fracture line running through the greater trochanter. The lesser trochanter is not involved. These stable fractures do not need as much mechanical support as other fracture types in this classification. Usually, type 31A1 fractures can be reduced on the fracture table without additional maneuvers and fixed with an extramedullary or short proximal intramedullary implant. Because of an intact lateral wall, these fractures are not at risk of extensive collapse or medialization of the shaft. For fixation of these fractures, a short nail is sufficient in most cases (Fig. 11-1).
AO/OTA 31A2
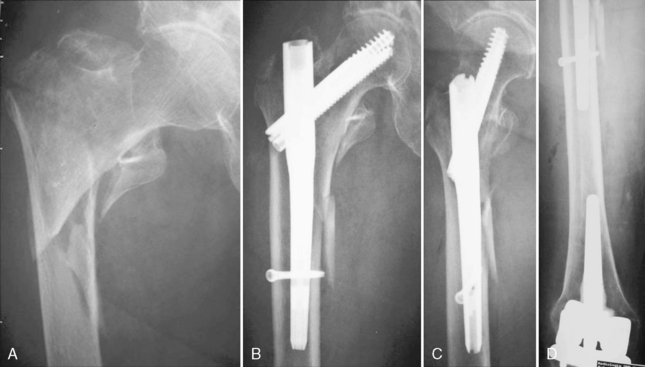
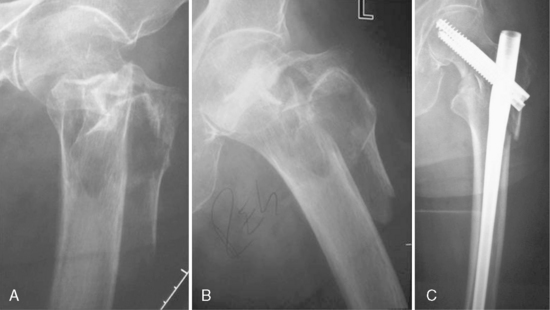
Type 31A2 fractures are pertrochanteric fractures that have more than two fragments, with the fracture line running through the greater and lesser trochanters. Type 31A2.2 and 31A2.3 fractures are defined as unstable. Because of the fractured medial column, mechanical support with a stable implant is required until bony consolidation is achieved. Reduction can be difficult. The proximal fragment can be dislocated in flexion, in varus, or both. Additional reduction maneuvers are commonly required. Fractures involving the lateral wall are at risk of extensive collapse or medialization of the shaft, if the implant supplies no lateral buttress. These fractures are better addressed by intramedullary nails because of the biomechanical advantages of these devices. In fractures with an intact lateral wall in the area of the interlocking screw entry point, short proximal nails can be inserted. If this area is fractured or if a pertrochanteric fracture extends into the shaft region, a long nail is chosen to provide axial stability. The choice of nail is postponed until lateral radiographs are acquired (Figs. 11-2 and 11-3).
AO/OTA 31A3
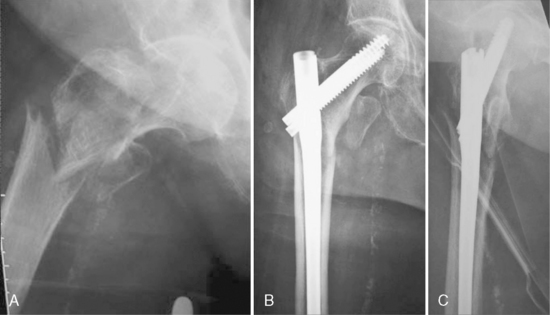
Type 31A3 fractures are classified as intertrochanteric fractures, with the fracture line running between the greater and lesser trochanters and involving the lateral cortex. These fractures are defined as unstable and are difficult both to reduce and to fix. The medial and lateral column is fractured, and the proximal fragment is short and usually dislocated. These fractures often require multidirectional reduction, which can be difficult to achieve because of the short proximal fragment. The special characteristics and biomechanical patterns of these fractures are especially evident in the reversed oblique intertrochanteric 31A3.1 type fracture. For fixation of all intertrochanteric 31A3 fractures, a long nail is required (Figs. 11-4 and 11-5).
Operative Technique
Reduction
Closed and Percutaneous Reduction Techniques
Gaining Control of Flexion Dislocation
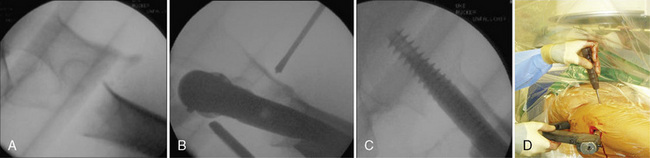
In patients with a remaining proximal fragment in flexion dislocation, the surgeon has several options for fracture reduction. The most elegant one is to insert a ball spike through a 5-mm stab incision over the ventral thigh. The ball spike applies down-vectored force to the malaligned fragment and leads to fracture reduction. Once adequate reduction is obtained, proximal reaming and nail insertion can be performed (Fig. 11-6).
An additional option for fracture reduction in flexion deformity is the use of radiolucent reduction aids mounted on the fracture table that push the shaft upward. If these aids are not available, a wooden crutch can be packed in sterile fashion and positioned under the limb. Reduction is obtained by lowering the table to the crutch (Fig. 11-7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree