1. A sinus tract communicating with the prosthesis
2. A pathogen is isolated by culture from two separate tissue or fluid samples obtained from the affected prosthetic joint
3. Four of the following six criteria exist:
(a) Elevated serum erythrocyte sedimentation rate (ESR) or serum C-reactive protein (CRP) concentration (CRP can be normal in low-grade infections!)
(b) Elevated synovial white blood cell (WBC) count
(c) Elevated synovial neutrophil percentage (PMN%)
(d) Presence of purulence in the affected joint
(e) Isolation of a microorganism in one culture of periprosthetic tissue or fluid
(f) Greater than five neutrophils per high-power field in five high-power fields observed from histologic analysis of periprosthetic tissue at 400 times magnification
Concerning tissue samples, it is advisable to stop antibiotics 14 days before taking the tissue biopsy because antibiotics can prevent isolation of intraoperative organisms on bacterial culture [13]. For the culture, the biopsy should be taken from deep tissue and not from superficial swab due to a low sensitivity (68 %) of the latter [10]. In the AAOS diagnostic criteria, isolating a pathogen from two separate intraoperative tissue samples is considered enough to make the diagnosis. Yet, there is other evidence for requesting at least three positive samples [9]. Obviously, obtaining more samples will increase the sensitivity of the detection of TKR infection at cost of increased work to perform. There is no agreement about the duration of the bacterial culture. Recent evidence recommends prolonged aerobic and anaerobic culture up to 14 days in order to find slow-growing anaerobic microorganisms such as Propionibacterium and Peptostreptococcus species [11, 12]. Unfortunately, prolonged incubation also means increasing risk of contamination.
Erythrocyte sedimentation rate (ESR) and especially C-reactive protein (CRP) have been shown to be excellent biomarkers of PJI. The kinetics of the CRP over time can give important information on the presence or absence of infection. Next to ESR and CRP, interleukin-6 is another promising biomarker that can be used in diagnosing PJI as shown in a systematic review in 2010 [14]. Synovial fluid should be analysed for leukocyte count and its neutrophils percentage (PMN%). The cutoffs of WBC count and PMN% differ in the knee and the hip joint. For the knee joint, WBC count >1.7 × 109/L showed a sensitivity of 94 % and specificity of 88 %. When this WBC count is combined with PMN% >65 %, the sensitivity and specificity become 97 and 98 %, respectively [15].
Several novel diagnostic methods are not included in the AAOS proposed criteria of PJI, such as sonication and polymerase chain reaction (PCR), but are worth mentioning. Sonication is a method used in the microbiology laboratory to dislodge microorganisms from the biofilm formed on the surface of the prosthesis [13]. This technique has been shown to have higher sensitivity for the microbiologic diagnosis of PJI than tissue culture. Sonication is particularly helpful in detecting bacteria in a patient recently treated with antibiotics. It is also useful to detect microorganisms that cause low-grade infection that are otherwise undetected using periprosthetic tissue culture such as Propionibacterium acnes [16]. A combination of sonication with microcalorimetry, an instrument that continuously measures heat production, has been shown to further increase the sensitivity and specificity of prosthetic joint infection [17]. PCR is a molecular technique that amplifies 16S rRNA gene of bacteria [18]. Multiplex PCR (meaning that multiple primers are used to amplify larger 16S rRNA gene in order to detect multiple bacteria types) has been developed and is shown to increase the sensitivity and specificity of PJI detection. The increase in diagnostic performance is more compelling when multiplex PCR is performed on the sonication fluid [18].
American Academy of Orthopedic Surgeons (AAOS) criteria can be used to define prosthetic joint infection.
60.4 Definition and Classification
Infection of TKR can be classified as early, delayed, and late (Table 60.2) [2]. Early infections occur within 3 months after implantation. The germs causing early infections are usually acquired during the implantation of the TKR. Delayed infections occur between 3 and 24 months after implantation. The germs causing delayed infections are also acquired during surgery, but they are usually less virulent, like Propionibacterium acnes or Staphylococcus epidermidis. Late infections are generally hematogenous and occur later than 24 months after implantation surgery. Staphylococcus aureus is the most frequent cause of hematogenous TKR infection [19]. In the majority of the cases, no primary focus of infection can be found.
Classification | Beginning of the infection after implantation | Pathogenesis | Typical germs |
|---|---|---|---|
Early infection | <3 months | During surgery | Highly virulent germs like S. aureus, Enterococci, or Gram-negative bacilli |
Delayed infection | 3–24 months | During surgery | Less virulent germs like S. epidermidis or P. acnes |
Late infection | >24 months | Mainly hematogenous | Typically highly virulent germs like S. aureus, streptococci, or Gram-negative bacilli |
Infection of TKR can be classified as early, delayed, and late.
After the classification, the next step in the decision making is to differentiate whether the infection of TKR is acute or chronic. This differentiation is important for the choice of the treatment option. Debridement with retention can be performed only in acute infection. Other conditions: stable implants, absence of sinus tracts, and susceptible microorganisms to antibiotics do need to be fullfilled (see further below). In acute infection, the beginning of the symptoms is less than 3 weeks before the diagnosis. Infection is considered to be chronic when the beginning of the symptoms goes back more than 3 weeks.
60.5 Patient-Tailored Treatment
Once the diagnosis has been made and the type of infection has been determined, the orthopedic surgeon together with the infectious disease specialist must make a treatment plan to achieve painless, functional, and infection-free TKR.
Medical treatment alone will not lead to eradication of the infection. Therefore, it should be only used in patients with multiple comorbidities (e.g., patients too sick to endure surgery), in patients who refuse surgery, or when surgery is too technically challenging [2, 20]. In all other situations, surgery in combination with appropriate antibiotics is the way to reach the treatment goal. The choice of surgical treatment is determined by several factors: the type of infection (acute versus chronic), the state of the soft tissue, the type of pathogens and their susceptibility to antibiotics, and patient’s expectation. There are five surgical options (Table 60.3).
Table 60.3
Five surgical options in treating TKR
1. Debridement and retention |
2. Single-stage exchange |
3. Two-stage exchange |
(a) With short interval (2–4 weeks) |
(b) With long interval (6–8 weeks) |
4. Arthrodesis |
5. Amputation |
Surgical options for treatment of infected TKR are debridement and retention, single-stage exchange, two-stage exchange, arthrodesis, and amputation.
60.5.1 Debridement and Retention with Exchange of Mobile Parts
Initially, it was thought that debridement and retention of the implant was a surgical procedure to be done by arthroscopy. Today, it has been shown that adequate debridement and retention with good results can only be done through an open procedure [21]. It consists of arthrotomy, extensive synovectomy, irrigation with 9 l of saline, and debridement of all infected soft tissue followed by exchange of the polyethylene (Table 60.4) [1]. The removal and exchange of the polyethylene is important to facilitate synovectomy in the posterior parts of the TKR and because there is a higher concentration of biofilm on the polyethylene than on the metal of the prosthesis (Fig. 60.1). Intraoperative cultures are taken, and mobile parts are sent for sonication. The patients are further treated with antibiotics for 3 months.
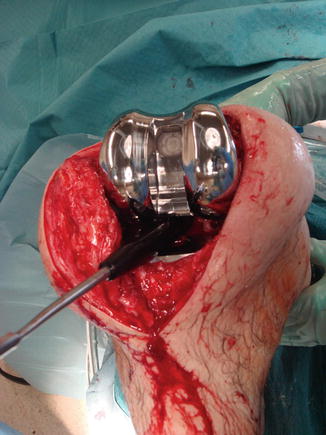
Table 60.4
Key points in the treatment of infected TKR using debridement and retention
1. Wide debridement of all infected tissue |
2. Removal of mobile parts |
3. Extensive synovectomy |
4. Cultures and sonication |
5. Low-pressure pulsed lavage |
6. New polyethylene block |
7. Antibiotics (systemic) for 3 months |
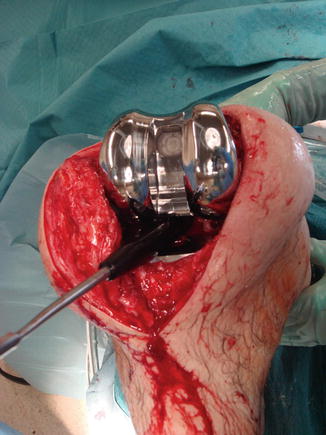
Fig. 60.1
Arthrotomy and removal of polyethylene block allows for best possible debridement
Compared to one- or two-stage exchange, there are several potential advantages of this method. Firstly, many patients can return to full activity quickly as the surgical aggression and the blood loss are more minor than in exchange procedures [21]. Secondly, surgical time and costs (only one surgery is performed and only mobile parts are exchanged) are lower. Thirdly, the risk of intraoperative fracture of the femur, the tibia, or the patella is low since the bone stock is left intact unlike in removal of a well-fixed prosthesis where bone loss occurs. Lastly, there will be no soft tissue distension or retraction, unlike in two-stage exchange where spacers are implanted. These possible advantages should be weighed against the low number of successful outcomes. The success percentage for this procedure is mainly reported just below 50 % [1, 21–23]. When debridement and retention fail, there will be also consequences concerning further surgical treatment. Sherrell and coworkers showed that two-stage revision replacement in patients who had previous debridement and implant retention had a high risk of failure (34 %) [24].
There are several requirements for a successful outcome when debridement and retention is performed [1, 2, 25]. Firstly, the implant should be stable. Secondly, the infection should be acute (i.e., less than 3 weeks). Thirdly, the soft tissue should be intact. Lastly, the pathogens should be sensitive to biofilm active antibiotics (i.e., rifampin, ciproxin, phosphomycin).
60.5.2 Single-Stage Revision
This surgical option consists of removal of the prosthesis, debridement of infected soft tissue, and reimplantation of a new prosthesis [2]. Intraoperative cultures are taken, and the removed prosthesis is sent for sonication. The patients are further treated with antibiotics for 3 months.
The most important theoretical advantage of this procedure compared to two-stage exchange is the elimination of the demanding second surgery that could result in complications [26], prolonged hospital stay, and increased patient morbidity related to the spacer. A disadvantage is the need to do more aggressive debridement and often the need for more constrained implants.
There are several requirements in performing single-stage exchange. Firstly, the soft tissue condition should be satisfactory (Fig. 60.2). If soft tissues are not sound, the risk of wound breakdown and persistence of infection or superinfection are increased. Secondly, like in debridement and retention, the pathogens should be sensitive to biofilm active antibiotics (i.e., rifampin, ciproxin, phosphomycin) [2].


Fig. 60.2
Long-term vacuum treatment led to superinfection and difficult soft tissue management
The success rate of single-stage exchange is high. A study by Jenny and coworkers showed that 87 % of the patients treated with single-stage exchange were free of any infection during 3 years follow-up [26].
60.5.3 Two-Stage Revision
This procedure has become the gold standard treatment in the United States [24, 27] and appears to be the most effective surgical management for infected TKR, with a success rate of 88–96 % [2] if debridement and retention are not possible.
In the first stage, the prosthesis is removed. It is important to choose the right surgical exposure. In general, the former incision should be used; in knees with multiple surgical scars, the most lateral incision should be chosen. Sinus tracts in line with the incision and away from the incision should be excised. It is advisable to discuss the surgical exposure with a plastic surgeon in case of difficult soft tissue situations in order to have a plan for how to cover the knee by a local or a free muscle flap. Once arthrotomy has been performed, systematic aggressive debridement and radical synovectomy should be done. It can be started from one side of the knee until only healthy-looking tissue is seen.
Once the soft tissues look clean, the implant can be removed. First, the polyethylene insert is removed, followed by removal of the femoral part. It is preferable to start with the femoral part because the exposure of the femoral part is easy and removal of the femoral part allows for better exposure of the tibia. Also, no debris or small cement fragments will fall into the tibial medullary canal during the removal of the femoral part. Osteotomes or a Gigli saw can be used to remove a stable uncemented prosthesis. During the removal of a cemented femoral prosthesis, detachment usually occurs at the cement-metal interface that can lead to less bone loss (Figs. 60.3 and 60.4). Additional bone loss can also occur during the removal of the cement. All macroscopically infected bone must be removed together with small cement fragments as they are covered with biofilm and might become a reservoir of infection and increase the risk of persistent infection. After removal of the tibial component, debridement should be performed to remove all foreign bodies, including nonabsorbable sutures, as they can be colonized. Intraoperative cultures are taken, and the removed prosthesis is sent for sonication (Fig. 60.5).




Fig. 60.3
While removing the femoral part of the TKR, the interface between cement and bone will usually give way

Fig. 60.4
On the tibial side, the interfaces between bone, cement, and tibial component are clearly individualized

Fig. 60.5
The prosthesis is put in a plastic box and later sent for sonication
In the first stage, a cement spacer is implanted. Among the general benefits of cement spacers are prevention of abundant scar tissue formation, maintenance of joint space, prevention of contraction of the collateral ligaments, facilitation of exposure and revision, and improvement of patient comfort between the stages [28, 29]. In current practice, cement spacers for two-stage exchange are impregnated with antibiotics because they can deliver local antibiotics in much higher dose than using intravenous administration [30, 31]. There are two types of cement spacers: non-articulating (fixed) [32, 33] and articulating (dynamic) spacer (Figs. 60.6, 60.7, 60.8, and 60.9) [31–33]. Fixed spacers (Figs. 60.10 and 60.11) have some shortcomings, such as inability for the patient to bend the knee, potential increase of bone loss, and quadriceps scarring and arthrofibrosis [34]. In contrast, dynamic spacers allow for joint motion. Moreover, due to less bone loss and decrease in scar formation, dynamic spacers facilitate exposure during reimplantation [29, 33–35]. Due to these characteristics, dynamic spacers also improve patient satisfaction [29, 33, 35]. Grossly, there are two types of articulating spacer: one that is made completely of antibiotic-impregnated cement using preformed molds and one made of metal and plastic coated with antibiotic-impregnated cement [32, 36]. Antibiotic concentration in the cement spacer is higher (>1 g per batch cement) when it is used to treat infection than when it is used as prophylaxis (≤1 g per batch cement) [30]. In two-stage exchange, 2 g of vancomycin and 4 g of tobramycin/gentamicin should be added to 40 g pack of bone cement [37, 38]. If the surgeon chooses not to create the spacer, preformed shelf spacers can be used as well. After the first stage, intravenous antibiotics are given to the patient.










