Traumatic Tendon Injuries
CASE PRESENTATION
A 14-year-old right hand-dominant male presents for evaluation of a “jammed finger.” While playing football 4 weeks ago, he reported “jamming” his ring finger while making a tackle. There was mild pain and swelling but no laceration, deformity, or obvious dislocation. Attributing it to a sprain, he did not initially seek medical attention. He now presents for evaluation due to persistent discomfort and swelling.
CLINICAL QUESTIONS
What are the mechanisms of flexor tendon injuries in children?
What are the physical examination and radiographic imaging techniques used to diagnose flexor tendon injuries in children?
What are the zones of flexor and extensor tendon lacerations in the hand?
What are the surgical indications and principles for tendon lacerations?
What are the indications for tenolysis?
What are the indications and techniques for reconstruction of chronic flexor tendon lacerations?
How are flexor tendon injuries cared for postoperatively?
What are the complications of flexor tendon surgery?
THE FUNDAMENTALS
Tendon injuries are common in children. Beware of glass lacerations, as the small external wound is not indicative of more extensive deep damage to nerves, tendons, and/or blood vessels. While the vast majority of injuries are due to deep lacerations or penetrations, closed tendon ruptures also occur. In general, tendon laceration or rupture is a surgical condition, but the technique of repair or reconstruction depends upon a host of clinical factors. Acuity or chronicity of injury, level of injury, associated bony or soft tissue lesions, and individual patient characteristics (maturity, hand dominance, functional demands, and ability to comply with postoperative rehabilitation) all play important roles in evaluation and treatment.
Etiology and Epidemiology
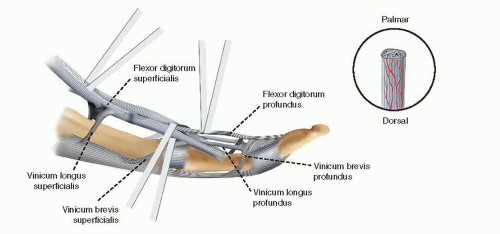
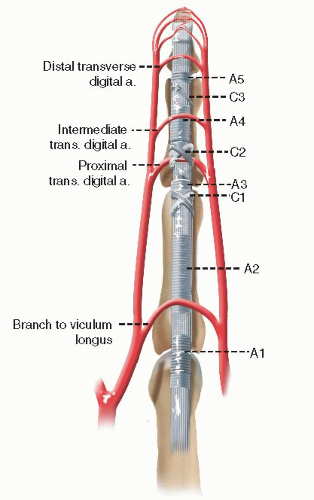
While the fundamental anatomy and basic science of tendon injury and healing are beyond the scope of this chapter, a few anatomic points are worth a review. First, most index through small fingers are flexed by the flexor digitorum profundus (FDP) and the flexor digitorum superficialis (FDS). These tendons have a very distinct anatomic relationship with one another as they pass through the fibro-osseous tendon canal (Figure 38-1). It is important to remember that a substantial proportion of humans do not have an FDS to the small finger. Second, the flexor tendons pass through a fibro-osseous tendon sheath, consisting of annular and cruciate pulleys (Figure 38-2). The tendon sheath and pulley system provide increased mechanical efficiency for joint motion but create challenges in terms of tendon exposure and reconstruction. Furthermore, vascular supply to the flexors is provided by the vincular system; during laceration or rupture, if these vascular connections are disrupted, the tendon may retract, the sheath fill with blood, and attritional changes could occur in the traumatized tendon stumps.
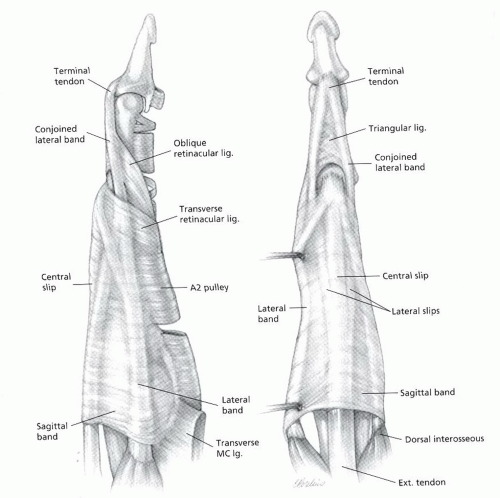
The extensor apparatus is more complex and elegant in its anatomic design (Figure 38-3). Again, the reader is referred to other sources for details regarding anatomy and basic science.1,2 The basic anatomic principles hold true for children and adults.
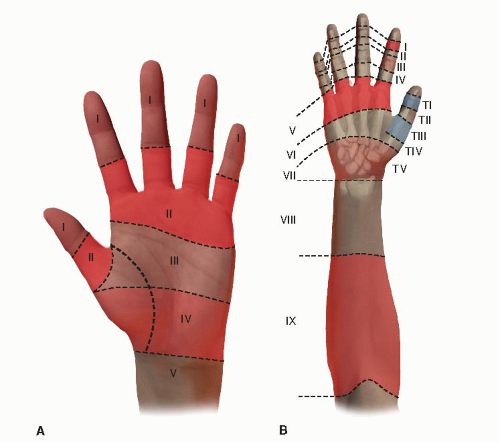
In general, tendon injuries are classified according to timing of presentation (acute or chronic), morphology (complete or partial), and anatomic location. Flexor tendon injuries are divided into zones, each with its own set of particular anatomic and surgical implications (Figure 38-4A; Table 38.1). Similarly, extensor tendon lacerations are divided into zones on the dorsal aspect of the hand (Figure 38-4B; Table 38.2).
Clinical Evaluation
Clinical evaluation begins with a good history. Information regarding the acuity of injury and the mechanism is most important. In older patients, additional questions may be asked about subjective numbness or tingling of the affected digit(s) as well as the quality of bleeding at the time of injury, which suggest concomitant injury to the adjacent neurovascular bundle. (Given the anatomic relationship between the more volar digital nerve and more dorsal digital artery, any volar finger laceration with profuse bright red bleeding should raise concern for a digital nerve laceration.) Chronicity is important, particularly after closed tendon ruptures, as long-standing injuries are associated with greater tendon retraction, myostatic contractures, and the potential need for single- or two-stage flexor tendon grafting and pulley reconstruction.
Physical examination should note the location, orientation, and quality of all lacerations and wounds, however small. Remember that small superficial lacerations may mask larger tendon and soft tissue injuries beneath. The vascularity of the digits should be assessed to determine the integrity of the digital arteries and guide surgical timing. Sensibility can be evaluated using light touch (threshold) or two-point discrimination (innervation density) testing. Discriminatory sensibility is usually present in patients older than 5 to 7 years of age. In rare situations, in a young child, the warm water immersion test can be performed to assess digital nerve function; if after soaking the affected hand in lukewarm water there is no wrinkling of the glabrous skin, a digital nerve injury should be suspected (Figure 38-5).
Table 38.1 Zones of flexor tendon injury | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 38.2 Zones of extensor tendon injury | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
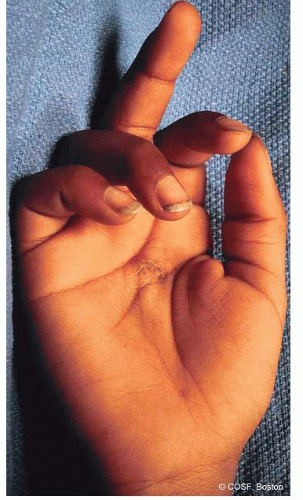
Assessment of flexor tendon integrity is performed by observation, passive motion, and active motion. Disruption of the normal digital cascade—in which each digit is slightly more flexed at rest than the adjacent radial digit—suggests flexor tendon laceration. This may be highlighted using the tenodesis effect, whereby passive wrist extension causes obligate passive digital flexion (Figure 38-6). In the young uncooperative or anxious child, compression of the FDS and FDP muscle bellies in the forearm, away from the zone of injury, is a helpful maneuver; again, absence of passive digital flexion should alert the examiner to a flexor tendon disruption. Finally, active distal interphalangeal (DIP) joint and proximal interphalangeal (PIP) joint flexion of each digit should be specifically assessed. Isolated DIP flexion is performed to test FDP function. For FDS testing, isolated PIP flexion with the other digits held in an extended position is needed to prevent the FDP—with its shared muscle belly—from flexing the tested digit. In cases of partial tendon lacerations, active flexion may be intact, but there will be pain with flexion against resistance.
Extensor tendon injuries are similarly assessed by observation and passive and active motion. Tenodesis
and passive wrist extension are helpful, as is specific testing of metacarpophalangeal (MCP) joint (sagittal bands), PIP (central slip), and DIP (terminal tendon) extension. Furthermore, it is important to recognize that in the case of an isolated central slip injury (the boutonniere deformity), the digit can still be actively extended, due to the pull of the extrinsic extensors through the lateral bands to the terminal tendon. To specifically test central slip integrity, the so-called Elson’s test is used.3 The PIP joint is flexed, and the patient is then asked to extend the PIP joint. In cases of central slip injuries, the DIP joint goes into rigid extension prior to attempted PIP joint extension.
and passive wrist extension are helpful, as is specific testing of metacarpophalangeal (MCP) joint (sagittal bands), PIP (central slip), and DIP (terminal tendon) extension. Furthermore, it is important to recognize that in the case of an isolated central slip injury (the boutonniere deformity), the digit can still be actively extended, due to the pull of the extrinsic extensors through the lateral bands to the terminal tendon. To specifically test central slip integrity, the so-called Elson’s test is used.3 The PIP joint is flexed, and the patient is then asked to extend the PIP joint. In cases of central slip injuries, the DIP joint goes into rigid extension prior to attempted PIP joint extension.
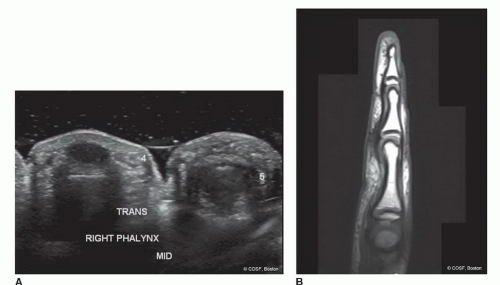
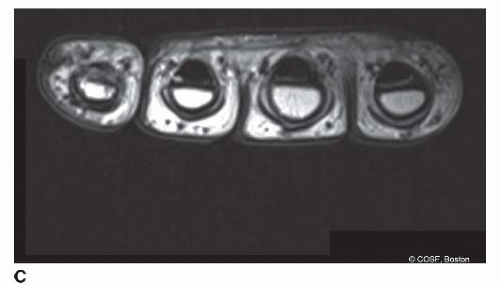
The diagnosis of tendon disruption is made clinically, though radiographic imaging may be helpful. Both ultrasound and magnetic resonance imaging (MRI) scans may be used to assess tendon integrity as well as the degree of retraction (Figure 38-7). This is particularly helpful in chronic injuries or postsurgical patients with limited motion in whom rerupture is suspected.
Surgical Indications
Surgical repair is indicated in all patients with open extensor tendon injuries and acute complete flexor tendon lacerations. Furthermore, flexor tendon repair or reconstruction is indicated in chronic flexor tendon disruptions in patients with significant functional limitations who are willing and able to comply with postoperative rehabilitation and activity restrictions.
SURGICAL PROCEDURES
Hitting is timing.
—Warren Spahn
Treatment of flexor tendon injuries is dependent upon the timing from injury to surgery. In acute flexor tendon lacerations, primary tenorrhaphy is performed using minimum four-strand core suture repair supplemented by an epitendinous suture repair. When surgery is delayed >4 weeks from injury, the myostatic contractures and tendon retraction may not allow for primary repair; in these cases, surgical treatment options include single-stage tendon grafting or staged flexor tendon reconstruction, depending upon the status of the fibroosseous canal.
• Closed Treatment of Mallet Fingers and Open Mallet Finger Extensor Repair
Mallet finger refers to the characteristic extensor lag associated with disruption of the terminal tendon’s insertion onto the dorsal distal phalanx. In children, due to the presence of the physis, clinical mallet fingers may actually represent Salter-Harris type III fractures of the dorsal epiphysis of the distal phalanx. Radiographs of the affected digit are needed to distinguish fractures (bony mallet finger) from true soft tissue extensor tendon injuries. The standard of care for closed soft tissue mallet fingers is continuous extension splinting of the DIP joint for 6 weeks; the PIP joint is left free and PIP motion encouraged to avoid lateral band and PIP joint adhesions and stiffness, respectively. After 6 weeks, part-time extension splinting is recommended for an additional 4 weeks during sleep and sporting activities.
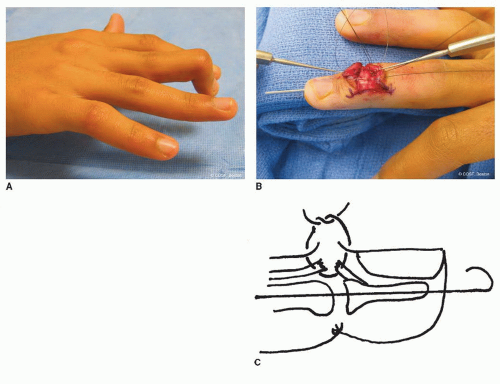
Occasionally, patients will present late with chronic mallet injuries. This situation is commonly seen in pediatric patients, due to either missed diagnosis or failure to comply with acute splinting. Usually, this is not painful or functionally limiting, and observation alone may be recommended. In the rare situation of the painful or functionally limiting chronic mallet finger, soft tissue reconstruction by tenodermodesis technique may be performed (Figure 38-8).4,5
Open mallet fingers are an indication for surgical treatment. After formal irrigation and debridement of the traumatic wound, the extensor tendon ends are mobilized, with care being taken to avoid iatrogenic injury to the germinal matrix during exposure and soft tissue dissection. The tendon ends are then reapproximated with interrupted figure-of-eight, cruciate, or core-grasping sutures; due to the thin, flat, often diaphanous consistency of the terminal tendon, traditional core-grasping sutures with heavy (3-0) braided nonabsorbable suture material may not be technically feasible. Tenodermodesis sutures may similarly be used in acute open mallet injuries if the quality of the tendon stumps is insufficient. After tendon repair, a single retrograde percutaneous pin is placed into the distal phalanx and across the DIP joint, holding the fingertip in full extension. A mallet splint or cast is applied. The pin is removed and splinting and therapy are initiated as described above 4 weeks postoperatively.
▪ Primary Tenorrhaphy of Acute Flexor Tendon Laceration
Under loupe magnification, flexor tenorrhaphy begins with adequate exposure. Although a variety of incisions have been advocated, we favor a volar zigzag Bruner approach, which is extensile, allows access to the radial and ulnar neurovascular structures, and can easily incorporate traumatic wounds.6 This is particularly useful, as both the distal and proximal flexor tendon stumps may retract and reside far from the initial traumatic laceration. For example, when a flexor tendon laceration is caused
by a child grasping a knife with a closed fist, the position of the tendon laceration is digital flexion; during surgery, as the finger is extended, the distal stump will lie more distal than the original wound, and the proximal tendon will retract due to the effect of the proximal muscle bellies. Skin flaps are carefully raised, and the tendon sheath and adjacent digital arteries and nerve are exposed.
by a child grasping a knife with a closed fist, the position of the tendon laceration is digital flexion; during surgery, as the finger is extended, the distal stump will lie more distal than the original wound, and the proximal tendon will retract due to the effect of the proximal muscle bellies. Skin flaps are carefully raised, and the tendon sheath and adjacent digital arteries and nerve are exposed.
Access to the flexor tendon is achieved by judicious opening of the flexor tendon sheath using the A1, C1-A3, and C3-A5 windows (Figure 38-9). Even prior to opening the sheath, tendon stumps may be localized by the characteristic hematoma that forms in the zone of injury and at the tendon ends. The A2 and A4 pulleys are preserved in an effort to avoid subsequent bowstringing. Working within these intervals, the flexor tendon stumps are identified.
One of the first intraoperative challenges is reapproximating the tendon ends within the same tendon sheath window. If there has been minimal retraction—often the vincula will prevent tendon migration, particularly in the acute setting—reapproximation is straightforward. In cases
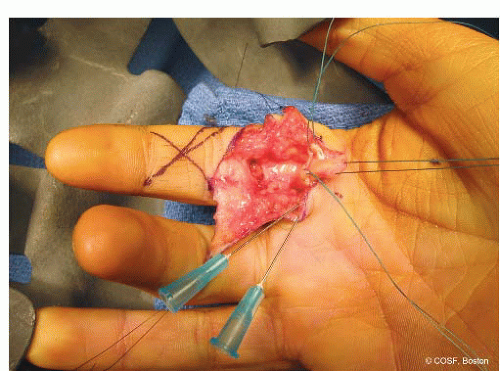
of greater tendon retraction, a number of retrieval methods have been described. First, a milking maneuver is performed. With the wrist and digit flexed, pressure on the volar surface of the wrist, hand, and digit is applied in a proximal to distal fashion. Often this will provide a glimpse of the proximal tendon stump, which may then be brought into the appropriate tendon sheath window. Second, a single blind pass with a small skin hook may be attempted.7 The hook is passed into the tendon sheath with the curvature of the hook flat. After the tendon stump is felt, the skin hook is rotated 90 degrees to engage the tendon end and pull it into the window of repair. This technique should be attempted only once, as repeated passes will only increase the local trauma and thus risk of subsequent fibrosis and tendon adhesions. Finally, a pediatric feeding catheter (typically 5 or 8 Fr in diameter) can be used as a tendon shuttle. The catheter is passed retrograde from the tendon gap, through the tendon sheath, proximally, into a region where the flexor tendon is identifiable (usually beneath the A1 pulley).8 The tip of the catheter is then temporarily sewn to the intact flexor tendon with a fine 5-0 or 4-0 nylon suture. Once secured, the catheter is withdrawn, delivering the flexor tendon into the zone of intended repair. The flexor tendon is held in place by a transverse 25-gauge hypodermic needle passed across the sheath and flexor tendon.
of greater tendon retraction, a number of retrieval methods have been described. First, a milking maneuver is performed. With the wrist and digit flexed, pressure on the volar surface of the wrist, hand, and digit is applied in a proximal to distal fashion. Often this will provide a glimpse of the proximal tendon stump, which may then be brought into the appropriate tendon sheath window. Second, a single blind pass with a small skin hook may be attempted.7 The hook is passed into the tendon sheath with the curvature of the hook flat. After the tendon stump is felt, the skin hook is rotated 90 degrees to engage the tendon end and pull it into the window of repair. This technique should be attempted only once, as repeated passes will only increase the local trauma and thus risk of subsequent fibrosis and tendon adhesions. Finally, a pediatric feeding catheter (typically 5 or 8 Fr in diameter) can be used as a tendon shuttle. The catheter is passed retrograde from the tendon gap, through the tendon sheath, proximally, into a region where the flexor tendon is identifiable (usually beneath the A1 pulley).8 The tip of the catheter is then temporarily sewn to the intact flexor tendon with a fine 5-0 or 4-0 nylon suture. Once secured, the catheter is withdrawn, delivering the flexor tendon into the zone of intended repair. The flexor tendon is held in place by a transverse 25-gauge hypodermic needle passed across the sheath and flexor tendon.
After the tendon stumps have been identified and retrieved, preparations are made for suture passage. It is clear that thicker suture material and a greater number of strands crossing the tenorrhaphy site increase the strength of the repair. While in adults, six- or eight-strand repairs have been performed, our practice is to perform four-strand repairs using either 3-0 or 4-0 nonabsorbable braided core sutures (Ethibond, Ethicon, Inc., Somerville, NJ) supplemented by a running locked, 6-0 monofilament epitendinous stitch (Prolene, Ethicon, Inc., Somerville, NJ). This is in part due to the small size of the tendons in children as well as our choice of postoperative rehabilitation. Currently, we perform a Strickland-type repair, which utilizes a Tajima core suture and horizontal mattress9




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree