The Thrower’s Elbow
CASE PRESENTATION
A 12-year-old youth baseball pitcher comes for evaluation of lateral elbow pain. He reports having soreness when pitching for the past 6 months but continued to participate in both school and town baseball teams. At his last outing, he reports having sudden onset of increased lateral elbow pain associated with swelling and elbow stiffness. He denies distal numbness, weakness, or tingling. He now presents for first clinical evaluation. Radiographs were interpreted as normal. Magnetic resonance imaging (MRI) studies are shown in Figure 41-1.
CLINICAL QUESTIONS
What are the causes of medial and lateral elbow pain in the young throwing athlete?
What is “osteochondritis dissecans (OCD)”? What causes it? How is it different from Panner disease?
Is pitching causative? What guidelines can be offered regarding how much pitching/throwing is safe and appropriate?
How do these patients present?
How is OCD classified?
What are the indications for surgical treatment?
What are the anticipated results of surgery for OCD?
THE FUNDAMENTALS
Sooner or later the arm goes bad. It has to. …Sooner or later you have to start pitching in pain.
—Whitey Ford
As participation in youth sports has increased, so too, it seems, has the prevalence of overuse injuries of the elbow. Among the various causes of lateral elbow pain in the young athlete is OCD of the capitellum. Most commonly seen in young throwers and gymnasts, OCD of the elbow is a common cause of pain, disability, and long-term impairment in the young, growing athlete.1,2 Medial elbow pain is also common and may be due to medial epicondylar apophysitis (see Chapter 39), ulnar collateral ligament (UCL) insufficiency, flexor-pronator tendinosis, and ulnar neuritis.
Etiology and Epidemiology
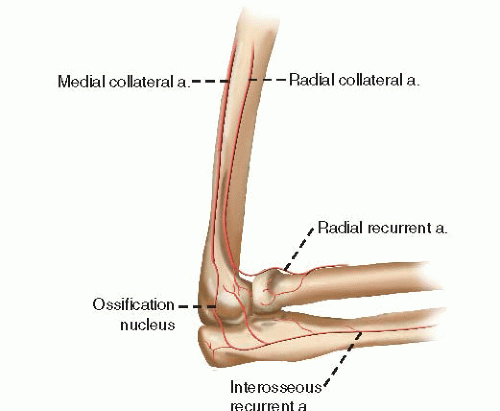
In general, OCD of the elbow results from excessive and repetitive compressive and shear forces across the radiocapitellar (RC) articulation in young, skeletally immature athletes. In the preadolescent and adolescent elbow, the vascular supply to the capitellar chondroepiphysis is tenuous, arising mainly from posterior perforating vessels and supplemented by limited terminal branches of the interosseous recurrent, middle collateral, radial collateral, and radial recurrent arteries (Figure 41-2).3, 4, 5, 6, 7 and 8 Given the forces imparted across the lateral elbow—during late cocking and early acceleration phases of throwing in the pitcher, for example, or during handsprings and vaulting in the young gymnast—limitations in vascularity result in the inability to heal after repetitive microtrauma.9 The subchondral bone fails, and the overlying cartilaginous articular surface is compromised. When left unchecked, this may lead to fragmentation and structural failure of the capitellar cartilage, resulting in loose body formation.10,11 Despite its name, inflammation does not play a role in the pathophysiology of elbow OCD.12
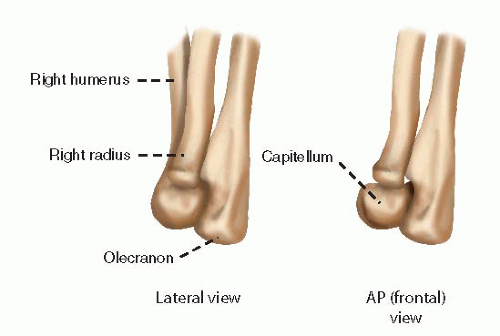
Panner disease refers to an “osteochondrosis” of the capitellum. Similar to the other osteochondroses of the femoral head (Legg-Calve-Perthes disease), navicular (Kohler disease), and scaphoid (Preiser disease), Panner disease typically affects the entire capitellar ossification center in boys under the age of 10 years.4,13, 14, 15, 16 and 17 The clinical presentation suggests that Panner’s may be due to repetitive microtrauma to the immature capitellar secondary center of ossification, which is vulnerable due to a host of hormonal, nutritional, and mechanical factors.4,5,8
While the risk factors may be similar, Panner’s is distinguished from OCD by a number of clinical differences.8 First, Panner’s tends to affect patients in the first decade of life, whereas the peak age for OCD is typically between 10 and 14 years of age. Second,
radiographically Panner’s involves the entire capitellar ossification center, while OCD lesions of the capitellum are more anatomically distinct, involving a specific part of the articular surface.18 Finally, Panner’s is thought to be a self-limited, self-resolving disease process, in contrast to OCD lesions, which when allowed to progress to fragment instability, have poor healing potential. Despite these distinct clinical features, many still believe that Panner’s and OCD represent different aspects of the same clinical entity.19
radiographically Panner’s involves the entire capitellar ossification center, while OCD lesions of the capitellum are more anatomically distinct, involving a specific part of the articular surface.18 Finally, Panner’s is thought to be a self-limited, self-resolving disease process, in contrast to OCD lesions, which when allowed to progress to fragment instability, have poor healing potential. Despite these distinct clinical features, many still believe that Panner’s and OCD represent different aspects of the same clinical entity.19
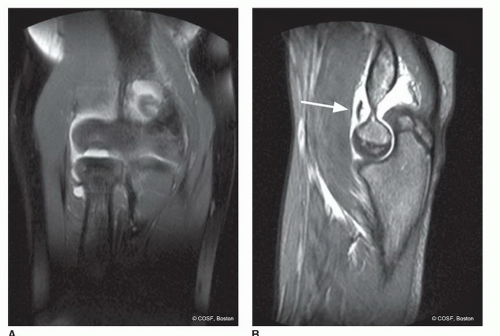 FIGURE 41-1 A: Coronal FSE PD MRI image demonstrates a capitellar osteochondral defect. B: Sagittal FSE IR MRI image reveals an intra-articular loose body in the anterior compartment of the elbow. |
Little epidemiological data are available regarding the true incidence or prevalence of OCD. Prior studies by Lyman et al.20 have clearly demonstrated that approximately a quarter of all youth baseball pitchers will report elbow pain during a baseball season. Presumably, a considerable proportion of these complaints will be due to OCD.21 Until more thorough screening and longitudinal observational studies are performed, the exact frequency with which OCD occurs will remain unknown.
Clinical Evaluation
Over 90% of patients with OCD will present with lateral elbow pain. While often casually attributed to lateral epicondylitis or “Little Leaguer’s elbow,” careful history and examination will elucidate that the location of the pain is in the capitellum, not the lateral epicondyle or extensorsupinator mass (Figure 41-3). Direct palpation over the capitellum, which can only be performed with the elbow hyperflexed, will elicit tenderness. While usually present only during or immediately after provocative activities (e.g., pitching, gymnastics), often patients will develop continuous pain even at rest in advanced situations.
Up to half of patients will demonstrate subtle loss of elbow motion, typically an elbow flexion contracture. This is often the first clinical sign of internal derangement of the elbow. An elbow effusion may or may not be detectable. Similarly, RC crepitus or instability may be elicited in those patients with unstable lesions. Neurovascular examination is usually normal.
In the young thrower or overhead athlete, careful examination of the shoulder will invariably detect an internal rotation deficit (see Chapter 39). Identification of this is critical in the rehabilitation of elbow OCD. As the patient tries to impart more angular velocity during throwing, the presence of an internal rotation deficit will often result in a lower arm-trunk angle (“dropping down”) and greater valgus and lateral compression forces across the elbow, thereby increasing the risk for OCD. Finally and perhaps most importantly, up to 20% of patients will present with mechanical symptoms of locking, catching, or giving way of the elbow. These symptoms should alert the examiner of the possibility of an intraarticular loose body and advanced stage of OCD.
In patients with medial elbow pain, tenderness with direct palpation of the medial epicondyle should alert the examiner to the possibility of medial epicondyle apophysitis. Tenderness more distally over the proximal flexor-pronator mass and pain with resisted wrist flexion are consistent with flexor-pronator tendinosis. In patients with suspected UCL insufficiency, a number of provocative maneuvers will elicit pain and/or instability, including: (1) valgus stress at 30 degrees of elbow flexion, (2) positive modified milking test, and (3) positive moving valgus stress test.22, 23 and 24 Finally, all patients with medial elbow pain should be assessed for ulnar nerve instability and ulnar neuritis. Ulnar nerve subluxation may be palpated with elbow flexion and extension. A Tinel’s sign, positive elbow flexion test, diminished sensation in the ulnar two digits, or any evidence of adductor pollicis or intrinsic weakness should raise the question of ulnar neuropathy.
Plain radiographs should be obtained during the initial evaluation, including anteroposterior (AP) and lateral views. Contralateral elbow radiographs may be helpful for comparison, particularly in the more skeletally immature. Takahara et al.25 have also highlighted the utility of the 45-degree flexion AP view, which may better bring an OCD lesion into profile given its characteristic posterior location within the capitellum (Figure 41-4). In cases of suspected UCL insufficiency, a gravity stress radiograph can be obtained. This view is performed with the patient supine, shoulder abducted 90 degrees, and forearm maximally supinated (thumb pointed to the ground). An AP view of the elbow is then taken with the beam directed parallel to the floor. Medial joint space opening of ≥3 mm is indicative of valgus instability.
Increasingly, MRI is becoming the standard imaging modality of choice, given its ability to localize and stage the OCD lesion, as well as identify associated pathology, including intra-articular loose bodies.26 T2-weighted coronal and sagittal reconstructions are particularly helpful in identifying adjacent signal abnormalities or fluid undercutting of the lesion, radiographic features suggestive of fragment instability. Also, MRI may be helpful in identifying flexor-pronator tendinosis, medial epicondyle apophysitis, and UCL tears.
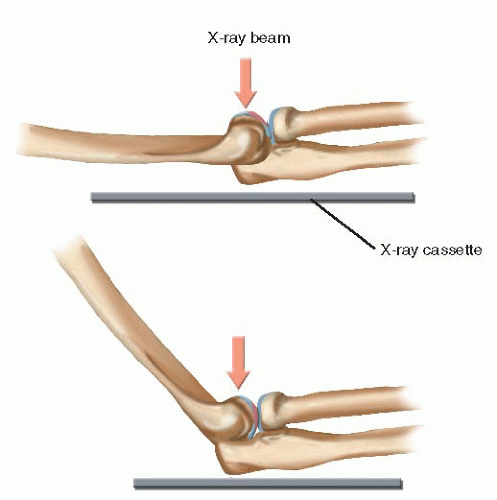 FIGURE 41-4 Schematic diagram depicting use of the 45-degree flexion AP view of the elbow to allow radiographic visualization of OCD lesions. |
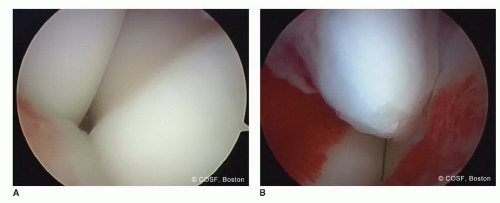
Currently, a host of classification systems exist for elbow OCD. Most are based on either radiographic or arthroscopic findings and divide lesions according to overlying cartilage integrity and fragment stability. Baumgarten et al.27 proposed an arthroscopic classification based upon that used to assess talar dome lesions. Grade 1 lesions had smooth but ballotable articular cartilage. Grade 2 lesions had cartilage fibrillations or fissures. In grade 3 lesions, there was exposed bone by stable osteochondral fragments. Grade 4 lesions were loose but undisplaced. Grade 5 lesions were displaced with intraarticular loose bodies.
Difelice et al.28 proposed a similar classification system, also based upon cartilage integrity and fragment stability (Table 41.1). Type 1a lesions have intact articular cartilage and fragment stability. Type 1b lesions have intact articular cartilage but unstable subchondral bone with impending collapse. Type 2 lesions demonstrate cartilage fracture with collapse or displacement of subchondral bone (e.g., unstable but in situ). Type 3 lesions denote intra-articular loose bodies. This classification system is similar to that of the International Cartilage Research Society classification of osteochondritis dissecans. Grade 1 lesions denote softened but intact cartilage surfaces. Grade 2 lesions have cartilage fissuring but are stable upon probing. Grade 3 lesions demonstrate complete discontinuity of cartilage but remain localized (“dead in situ”). Grade 4 lesions describe displaced lesions. All these classification systems are helpful not only to describe radiographic or arthroscopic appearance but also in guiding treatment. As with many upper limb conditions, however, clinical symptoms often do not correlate with radiographic findings.1
Surgical Indications
Surgical treatment is indicated in cases of symptomatic elbow OCD with fragment instability or intra-articular loose bodies. Furthermore, surgical treatment is also relatively indicated in cases of stable OCD lesions with persistent functionally limiting pain despite “adequate” rest and rehabilitation.
Table 41.1 Classification of elbow OCD lesions | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
SURGICAL PROCEDURES
The downside isn’t really injury, fear of injury, or the process of fighting injury. The downside, the very worst thing in the world, is surgery.
—Greg Rusedski
• Nonoperative Treatment of Elbow OCD
Nonoperative treatment is recommended for the intact, stable elbow OCD lesion, particularly in the young, skeletally immature athlete. Complete rest of the affected elbow is initiated for 6 weeks, followed by physical therapy to work on posterior capsular stretching of glenohumeral internal rotation deficit, strengthening of the rotator cuff and periscapular muscles, strengthening of the flexor-pronator mass, and special attention to throwing mechanics. Core strengthening is a major part of their rehabilitation, as most of those young athletes need to transition from using their arm to using their core (knees to chest) musculature to increase throwing velocity. While advocated by some, we do not typically utilize hinged or varus elbow braces, given that the upper limb is a non-weight-bearing joint. This is reserved for the hyperactive child who just will not or cannot slow down. Typically, throwing is resumed once the patient demonstrates no pain, even with direct palpation over the capitellum, and full elbow motion symmetric to the opposite side. An interval throwing program is initiated, with emphasis on the “soreness rules,” which limit progression or advancement through pain. Patients and families are counseled that it may be many months until vigorous throwing (or gymnastics, etc.) can be resumed.29 This is not always an easy “sell,” but the risk of long-term arthritis needs to be kept in mind.30
▪ Medial Epicondyle Avulsion Fracture
While further details regarding medial epicondylar fractures in children are provided in Chapter 29, a brief discussion is warranted here. In addition to the valgus compression forces on the lateral elbow resulting in elbow OCD, tensile forces on the medial elbow may result in avulsion fractures
of the medial epicondyle in young throwers, gymnasts, wrestlers, cheerleaders, and other overhead athletes. With small avulsion fractures, the athlete will often indicate a particular moment (e.g., “sixth inning, clean-up batter at the plate for the other team, tying run on third, and I threw my best fastball and felt immediate pain”) that resulted in the injury. These fractures will heal with nonoperative management. Complete displacement of the entire medial epicondyle comes with macrotrauma (doing a floor routine in gymnastics with a fall). The displaced fractures may result in symptomatic valgus instability and altered flexorpronator function in these high-demand athletes. For this reason, surgical reduction and fixation are recommended for displaced medial epicondyle fractures in young overhead or upper limb-weight-bearing athletes.
of the medial epicondyle in young throwers, gymnasts, wrestlers, cheerleaders, and other overhead athletes. With small avulsion fractures, the athlete will often indicate a particular moment (e.g., “sixth inning, clean-up batter at the plate for the other team, tying run on third, and I threw my best fastball and felt immediate pain”) that resulted in the injury. These fractures will heal with nonoperative management. Complete displacement of the entire medial epicondyle comes with macrotrauma (doing a floor routine in gymnastics with a fall). The displaced fractures may result in symptomatic valgus instability and altered flexorpronator function in these high-demand athletes. For this reason, surgical reduction and fixation are recommended for displaced medial epicondyle fractures in young overhead or upper limb-weight-bearing athletes.
While surgery may be performed in the prone position with the shoulder internally rotated to impart a varusproducing force on the elbow, our preference is to perform these procedures in the supine position with the limb supported by an operating hand table if the patient has enough external rotation at the shoulder to allow easy access to the posteromedial elbow. Positioning this way makes fluoroscopy a bit easier than prone or “sloppy lateral” positioning. We check for the shoulder passive range of motion under anesthesia before a final positioning decision is made. A nonsterile tourniquet is utilized. A longitudinal incision based upon the medial epicondyle and medial column of the distal humerus is made. Skin flaps are carefully raised, understanding that the course of the medial antebrachial cutaneous nerve (MABCN) is quite variable. The MABCN often runs with the more easily identifiable basilic vein and should be protected to avoid symptomatic numbness or neuroma formation. Deep dissection will allow for identification of the ulnar nerve. While it is unnecessary to dissect the ulnar nerve circumferentially, it is critical to localize and gently retract the nerve during bony fixation, particularly as a high percentage of young patients will exhibit asymptomatic ulnar nerve subluxation.31
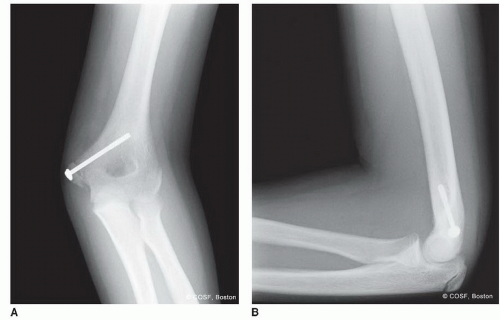 FIGURE 41-5 Postoperative anteroposterior (A) and lateral (B) radiographs following open reduction and internal fixation of a displaced medial epicondyle fracture. |
Once the ulnar nerve is retracted and protected, direction is turned to the fracture. The medial epicondyle fragment is identified along with the attached origin of the flexor-pronator muscles. A 2-0 suture (Ethibond, Ethicon, Inc., Somerville, NJ) may be placed through the superior periosteum overlying the displaced fracture fragment to be used for traction during the case. The bony donor site is similarly identified and fracture hematoma and fibrous tissue are debrided. Under direct visualization, the fracture is reduced. This typically requires flexing the elbow and imparting varus stress while the forearm is pronated to relax the deforming forces. A threaded guide pin from the 3.5- or 4.5-mm cannulated screw set (Synthes, West Chester, PA) is placed into the medial epicondyle, across the fracture site, and up the medial column of the distal humerus; care is taken to place this guide pin in the center of the fracture fragment to avoid fragmentation of the typically small displaced epicondyle (Figure 41-5). A slick way to do this is drill the center of the medial epicondyle in the displaced position; with the drill bit just protruding
from the fragment, anatomically reduce the fracture fragment; and then drill up the humerus obliquely avoiding the olecranon fossa. A second guide pin can be placed for temporary rotational control. Either a partially threaded cancellous screw or a fully threaded cortical screw can be used successfully. If a cancellous screw is used, and the fragment is big enough, then the central guide pin is overdrilled, and a partially threaded cannulated screw with a washer is placed, providing compression across the fracture site. Screw length is typically between 35 and 50 mm, and purchase of the far cortex is not necessary for adequate compression and fixation. If the fragment is smaller and there is concern about fragmentation with fixation, then a cortical screw and washer can be used. Cortical purchase is advised, but the screw needs to be removed sooner to prevent complications. Intraoperative fluoroscopy will confirm reduction, implant placement, and elbow stability. Suture repair of the flexor-pronator origin and periosteum increases stability and rotational control. The wound is closed in layers, and a long arm-bivalved cast is applied. Patients are transitioned into a hinged elbow brace by the second postoperative week to begin gentle range-of-motion exercises.
from the fragment, anatomically reduce the fracture fragment; and then drill up the humerus obliquely avoiding the olecranon fossa. A second guide pin can be placed for temporary rotational control. Either a partially threaded cancellous screw or a fully threaded cortical screw can be used successfully. If a cancellous screw is used, and the fragment is big enough, then the central guide pin is overdrilled, and a partially threaded cannulated screw with a washer is placed, providing compression across the fracture site. Screw length is typically between 35 and 50 mm, and purchase of the far cortex is not necessary for adequate compression and fixation. If the fragment is smaller and there is concern about fragmentation with fixation, then a cortical screw and washer can be used. Cortical purchase is advised, but the screw needs to be removed sooner to prevent complications. Intraoperative fluoroscopy will confirm reduction, implant placement, and elbow stability. Suture repair of the flexor-pronator origin and periosteum increases stability and rotational control. The wound is closed in layers, and a long arm-bivalved cast is applied. Patients are transitioned into a hinged elbow brace by the second postoperative week to begin gentle range-of-motion exercises.
A couple of technical pearls bear mention. First, anatomic fracture reduction can be challenging when performing the surgery in the supine position. The valgusextension position needed for visualization often impedes anatomic reduction. In addition to elbow flexion, forearm pronation, and varus stress, a dental pick or fracture reduction clamp may be helpful. (In our operating room, we have used a sterilized dinner fork with the central tines removed to facilitate fracture reduction and placement of the central guide pin). Alternatively, the drill hole in the epicondylar fragment and the medial column may be predrilled prior to reduction. Once the cannulated screw is placed into the fracture fragment, the screw tip may be inserted into the drilled medial column, using the screw itself to facilitate reduction. Second, it is important to remember that the medial epicondyle is a posterior structure. For this reason, the screw trajectory should be slightly posterior to anterior, and the lateral fluoroscopic image should demonstrate the posterior position of the screw head once fixation is complete. Failure to do so will result in nonanatomic fixation and suboptimal results.
♦ Arthroscopy and Drilling
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree