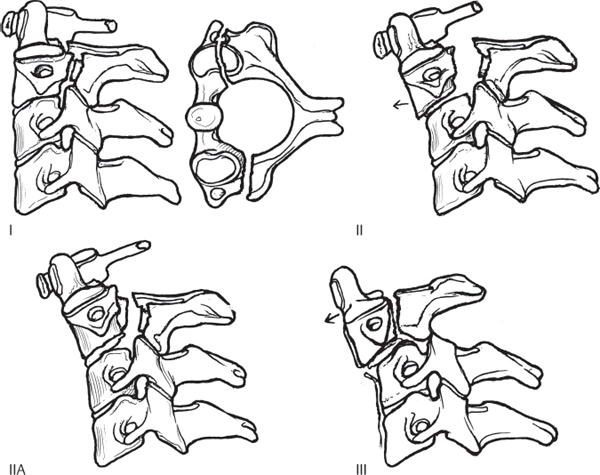
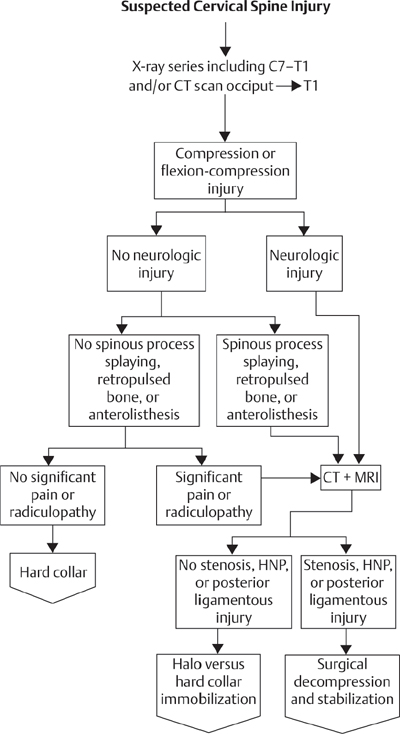
5 Traumatic spondylolisthesis of the axis, or hangman’s fracture, refers to a fracture through the neural arch of the axis (pars interarticularis) with or without disruption of the C2–C3 articulation. The pars interarticularis is the narrow isthmus of bone connecting the superior and inferior articular facets. Despite the colloquial name, the typical mechanism is quite different from that observed with judicial hangings. Judicial hangings produce a forceful distraction and hyperextension of the spine, while most hangman’s fractures occur with a blunt impact to the head causing forced hyperflexion or hyperextension. The classification system of Effendi and Levine is most commonly used and is based on angulation and/or subluxation of the fracture fragments (Fig. 5.1). A Type I fracture has a fracture line traversing the C2 pars with minimal displacement (less than 3 mm) and with no angulation. The Type II fracture pattern is similar but demonstrates significant angulation and displacement of greater than 3 mm. Type IIA fractures show significant angulation without much displacement. This injury pattern results from flexion and distraction of the C2–C3 segment with disruption of the posterior longitudinal ligament, leaving the anterior longitudinal ligament intact. Traction should be avoided with the Type IIA injuries, as it may lead to increased angulation. Type III injuries are the most severe and involve displacement and angulation of the fracture line in combination with a unilateral or bilateral facet dislocation of the C2–C3 facet joint. Type III injuries result in a high rate of spinal cord injury and are most commonly treated with open reduction. The atypical hangman’s fracture, or Type IA, involves a fracture line that traverses the C2 body obliquely, leaving bony fragments anterior to the spinal cord. This injury is more likely to be associated with a spinal cord injury than are other Type I and Type II injuries. Fig. 5.1 The four types of fracture of the neural arch of the axis, known as hangman’s fractures. Type I: minimally displaced with no angulation. Type II: angulated and displaced. Type IIA: minimal displacement with angulation. Type III: severely angulated and displaced with uni/bilateral facet dislocation. Any patient sustaining a significant injury to the head/neck region should be immobilized until radiological studies can be completed. The most common causes of hangman’s fractures are significant falls or motor vehicle collisions. Patients with hangman’s fractures present with neck pain and tenderness over the upper cervical region, especially at the C2 spinous process. A thorough neurological examination is required to rule out a spinal cord injury. Closed head injuries are frequently seen in patients with hangman’s fractures and may significantly affect outcome. Radiographic studies, including anteroposterior (AP), lateral, and open-mouth views, are routinely done when a cervical injury is suspected. When a cervical fracture is noted (or the region of the cervical spine is poorly visualized), a cervical computed tomography (CT) scan should be obtained. Magnetic resonance imaging (MRI) is useful for patients with spinal cord injuries or when a ligamentous disruption is suspected. Type I and Type IA fractures are stable and are treated with a semi-rigid cervical collar for 8 to 12 weeks. Type II fractures are less stable; some advocate initial reduction with skeletal traction (placing the neck in slight hyperextention and applying 10–15 lbs of cranial traction). Fractures with less than 4 or 5 mm of displacement and 15 degrees of angulation may be considered for early mobilization in a halo vest, which is worn for ~ 8–12 weeks. Patients with less stable injuries may first be treated with initial traction for several weeks until fracture callus begins to form, followed by placement of halo vest orthosis. With Type IIA fractures, traction should be avoided. These injuries are best treated with early application of a cervical orthosis (halo vest) in slight extension and compression for 8–12 weeks. Type III injuries are generally not amenable to closed reduction and require open reduction of the facets, followed by arthrodesis using internal fixation. Neurologically intact patients should be studied with MRI prior to the reduction to ensure that a traumatic disk herniation is not present that would preclude a safe reduction of the fracture. As an alternative, unstable fractures (Types II and III) have been successfully treated by direct screw osteosynthesis of the fracture site, placing lag screws across the fractured pars interarticularis. Outcomes depend on the fracture type. Types I and IA fractures do well, with union rates approaching 98%. The most frequent long-term complication involves post-traumatic degeneration of the C2–C3 facet joint, which is seen in 10%. Type II fractures with uncorrectable displacement of 5 mm or greater have a high incidence of nonunion, but commonly undergo fusion of the C2–C3 disk space, providing stability to the segment in 70% of patients. Type III fractures have high rates of union following surgical arthrodesis. Patients sustaining a spinal cord injury in the setting of a hangman’s fracture have outcomes similar to other neurologically injured patients, with the long-term outcome dependent on the severity of the spinal cord injury. Nonunion, post-traumatic arthritis, and neurological deficits may occur. Complications of fracture treatment, such as halo pin loosening, infection, and skull perforation, must be watched for. Associated injuries, particularly closed head injuries, often complicate the treatment of hangman’s fractures. Bucholz RW, ed. Orthopaedic Decision Making. 2nd ed. St Louis, MO: Mosby; 1996:420–423 This chapter provides useful descriptions of radiographic evaluation of trauma patients with suspected cervical spine injuries. An overview of the treatment of hangman’s fractures based on the Levine and Edwards classification is also discussed. Pepin JW, Hawkins RJ. Traumatic spondylolisthesis of the axis: Hangman’s fracture. Clin Orthop Relat Res 1981; (157):133–138 PubMed The authors give an overview of the etiology of hangman’s fractures. They also describe a classification system based on fractures being either displaced or non-displaced, to be used in determining treatment options. However, this did not completely address the issue of instability. DeLee JC, Drez D Jr, Miller MM, eds. DeLee and Drez’s Orthopaedic Sports Medicine. 2nd ed. Philadelphia, PA: Saunders; 2003:834 The author gives an introduction to hangman’s fractures, including mechanism of injury, patient presentation, evaluation and treatment. Levine AM, Edwards CC. The management of traumatic spondylolisthesis of the axis. J Bone Joint Surg Am 1985;67(2):217–226 PubMed This article introduces the Levine and Edwards classification system of hangman’s fractures, most widely used today for treatment. The classification was based on their study of 52 patients and takes stability into account. Longo UG, Denaro L, Campi S, Maffulli N, Denaro V. Upper cervical spine injuries: Indications and limits of the conservative management in halo vest. A systematic review of efficacy and safety. Injury 2010;41(11):1127–1135 PubMed Forty-seven studies including 1078 patients treated in halo vests for C1–C2 fractures were reviewed. A discussion of the safety and efficacy of halo vest is presented. Ma W, Xu R, Liu J, et al. Posterior short-segment fixation and fusion in unstable hangman’s fractures. Spine (Phila Pa 1976) 2011;36(7):529–533 PubMed The authors present a series of 35 patients treated with posterior C2–C3 fusion using C2 pedicle screws and either C3 pedicle screws or lateral mass screws. Fusion was noted in 29 patients, and few surgery-related complications were noted. Schneider RC, Livingston KE, Cave AJE, Hamilton G. “Hangman’s fracture” of the cervical spine. J Neurosurg 1965;22:141–154 PubMed This article gives a historical introduction of the etiology, presentation, and treatment of hangman’s fractures. The author first coined the term “hangman’s fractures” for C2 fractures resulting from vehicular accidents, after noting the similarity with those sustained in judicial hangings. Sherk HH, Howard T. Clinical and pathologic correlations in traumatic spondylolisthesis of the axis. Clin Orthop Relat Res 1983; (174):122–126 PubMed This article correlates the clinical treatment and prognosis of hangman’s fractures with the anatomic lesion. The authors report that fractures that occur through the superior articular facet have a high potential for union because of the well-vascularized cancellous bone of the area, versus those that occur through the thin cortical bone of the pars interarticularis. Vaccaro AR, Madigan L, Bauerle WB, Blescia A, Cotler JM. Early halo immobilization of displaced traumatic spondylolisthesis of the axis. Spine (Phila Pa 1976) 2002;27(20):2229–2233 PubMed In this retrospective study of early halo immobilization in Type II and IIa fractures in 31 patients, the authors found that patients with initial angulation of greater than 12 degrees on lateral radiographic films required an extended period of traction. CT, computed tomography; HNP, herniated nucleus pulposus; MRI, magnetic resonance imaging
Traumatic Spondylolisthesis of the Axis (Hangman’s Fracture)
![]() Classification
Classification
![]() Workup
Workup
![]() Treatment
Treatment
![]() Outcome
Outcome
![]() Complications
Complications
Recommended Reading
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







