PATRICIA A. WINKLER, PT, DSc, NCS After reading this chapter the student or therapist will be able to: 1. Describe the application of current concepts in motor control and motor learning theories for clients with traumatic brain injury. 2. Understand the meaning of impairment, activity limitation, and participation limitation and their interrelationships as they apply to clients with traumatic brain injury. 3. Prescribe methods of examining, evaluating, and developing interventions for clients with brain injuries on the basis of task, impairment, and activity limitation analysis. 4. Describe prognosis and outcomes for clients with traumatic brain injury. 5. Differentiate between development of basic movement patterns and motor skills. 6. Understand the role of synergy formation, synergy selection and modification, and anticipatory and feedback information as used in motor skills. 7. Describe the long-term effects of different types of feedback and practice on learning. Traumatic brain injury (TBI) is defined as a blow or jolt to the head or a penetrating head injury that disrupts the function of the brain. Not all blows or jolts to the head result in a TBI. The severity of such an injury may range from mild—a brief change in mental status or consciousness—to severe—an extended period of unconsciousness or amnesia after the injury. A TBI can result in short- or long-term problems with independent function.1 One and three-quarter million people sustain a TBI every year.1 Of these, 1.3 million are treated in emergency departments and 275,000 injuries are severe enough to require hospitalization.2 Fifty-two thousand people die yearly of TBI, 80,000 injuries result in disabilities, and 5.3 million people are living with permanent disabilities from TBI. It is the leading killer and disabler of children and young adults. Motor vehicle crashes cause 20% of all TBIs, falls cause 28%, violence causes 11% (the majority from firearms), and sports and recreation account for 10%. Child abuse accounts for 64% of infant brain injuries.1 Fifty-thousand children sustain bicycle-related brain injuries, and 400 of them die.3 Two thirds of firearm-related TBIs are suicidal. Falls are the leading cause of TBI in people aged 65 years and older, with 11% proving fatal. The incidence of TBI is 506.4 per 100,000 population, with 43% of those hospitalized having long-term activity limitation.4 The incidence of brain injuries is higher for the male population than for the female population by more than 2:1. Most of those injured are 15 to 24 years old.4 The greatest risk of injury is for those younger than 10 years old or older than 74. American Indians and African Americans have the highest rate of TBI. People in lower socioeconomic status also have a higher rate of injury. There are four main types of injury, as follows: 1. Those from external forces hitting the head or the head hitting hard enough to cause brain movement. Injuries include those with skull fracture and those without skull fracture (closed head injuries). Direct blows to the head can cause coup injuries (at the site of impact) and contrecoup injuries (distant from the site of impact). 2. Severe acceleration and deceleration of the head can cause TBI without the head hitting an object. An example is shaken baby syndrome. 3. Blast injuries have become very common in the past 10 years, mainly affecting military personnel. 4. Penetrating objects cause direct cellular and vascular damage. Injuries to the face and neck can cause brain injury by damaging the blood supply to the brain.5 Contusions—a bruise or bleeding on the brain—and lacerations can occur with or without skull fractures. Either an object hits the head, neck, or face, or the head hits an object. Damage can be to any area of the brain. Occipital blows are more likely to produce contusions than are frontal or lateral blows. Areas in which the cranial vault is irregular, such as on the anterior poles, undersurface of the temporal lobes, and undersurface of the frontal lobes, are commonly injured. Lacerations of blood vessels within the brain itself or of blood vessels that feed the brain from the neck or face reduce the flow of blood carrying oxygen to the brain. Contusions and lacerations can also injure the cranial nerves. The most commonly injured are the optic, vestibulocochlear, oculomotor, abducens, and facial nerves. Lacerations of the dura or in the arachnoid space may cause cerebrospinal fluid to discharge from the nose (cerebrospinal fluid rhinorrhea discharge increases with neck flexion, coughing, or straining).6 An example of a computed tomography (CT) scan of a cerebral contusion can be found in Chapter 37, Figure 37-17, B. Subdural hematomas occur with acceleration-deceleration injuries when bridging veins to the superior sagittal sinus are torn. Blood accumulates in the subdural space. Symptoms include weakness and lethargy. Symptoms such as weakness and lethargy that come on acutely are life-threatening. Symptoms caused by slow bleeding may not be present for several weeks. A CT scan of this problem can be found in Chapter 37, online image Figure 37-17, A. Also, note on the same figure the midline shift of the brain. Diffuse axonal injuries, or shearing injuries, are among the most common types of primary lesions in patients with brain trauma.7,8 Brain tissues that differ in structure or weight experience unequal acceleration, deceleration, or rotation of tissues during rapid head movement or during impact, causing diffuse axonal injury and changes in chemical processing. Refer to Chapter 37, Figure 37-17, D for an illustration of what axons are most affected by this shearing motion. Severing of the axons may be severe enough to result in coma. In milder forms, more spotty lesions are seen, including deficits such as memory loss, concentration difficulties, decreased attention span, headaches, sleep disturbances, and seizures. Damage often involves the corpus callosum, basal ganglia, brain stem, and cerebellum.6,8 For a complete image of how the axons diffuse throughout the entire CNS, refer to Figure 37-17, C. Blast injuries occur when a solid or liquid explosive material explodes, turning into a gas. The expanding gases form a high-pressure wave (overpressure wave) that travels at supersonic speed. Pressure then drops, creating a relative vacuum (blast underpressure wave) that results in a reversal of air flow, which is in turn followed by a second overpressure wave. Blast-related injury can occur through several mechanisms. The primary blast wave generates extreme pressure changes that can cause stress and shear injuries. For example, rupture of the tympanic membranes is very common after blast injury, and lung and gastrointestinal injuries also occur. The exact mechanism of injury to the brain is unknown, with speculation about both axonal shearing and shearing of vasculature.9,10 Box 24-114 lists possible autonomic nervous system symptoms resulting from brain injury. Motor abnormalities after severe head trauma are common. More severe head injuries tend to manifest more persistent physical problems.6 In at least two studies6,15 a fourth of the cases had no neurophysical sequelae. Changes in muscle tone may reflect the physiological effects of changes in the amount of tissue compression or irritation.16 Box 24-2 lists motor changes and provides symptoms of sensory and perceptive involvement. The social consequences of inappropriate behavior can be disastrous and a stumbling block to achieving therapy goals. A correlation between preinjury personality and postinjury changes has not been established.6 It does seem reasonable, however, that factors within an individual’s psychological makeup may affect reaction to the injury. Brain trauma frequently happens to adolescents—an age group fraught with its own problems that may be aggravated by the injury. Outcomes at 1 year postinjury have shown the most common problems to be poor memory and problem solving, problems managing stress and emotional upsets, and an inability to control temper. Finally, managing money and paying bills were still a problem at the 1-year mark.17 Box 24-318 lists both cognitive and behavioral changes resulting from brain injury. Coma and changes in consciousness result from conditions in which there are diffusely extensive and bilateral cerebral hemispheric depression of function, direct depression or destruction of the brain stem–activating system that is responsible for consciousness or a combination of the two. In moderate or severe head injury, unconsciousness can be prolonged. Plum and Posner’s definitions16 of various stages of acutely altered consciousness are briefly presented, intermingled with some insights from the descriptions offered by Gilroy and Meyer.11 Plum and Posner19 do not equate the presence or absence of motor responses with the depth of coma. These authors point out that the neural structures regulating consciousness differ from and are more anatomically distant from those regulating motor function. In mild concussion, the loss of consciousness may not occur or lasts a relatively short time (20 minutes or less) and there is little or no retrograde amnesia. A concussion can cause diffuse axonal injury and result in either temporary or permanent damage. The client may be irritable or distractible and have difficulty with reading and memory. There may be complaints of headache, fatigue, dizziness, and changes in personality and emotional disposition. This group of symptoms constitutes what is called posttraumatic syndrome. The effects of repeated concussions (second impact syndrome) are cumulative.20 Coma is defined as a complete paralysis of cerebral function; a state of unresponsiveness. The eyes are closed, and there is no response to painful stimuli. Within 2 to 4 weeks, nearly all clients in coma begin to awaken. Oculomotor and pupillary signs are valuable in assisting with the diagnosis, localizing brain stem damage, and determining the depth of coma.19 In coma, brain stem responses may include grimacing to pain, which is frequently associated with a flexor or localizing motor response, loss of hearing or balance, abnormal palate and tongue movements, and loss or distortion of taste. Finally, no discussion of changes in consciousness would be complete without mention of those unfortunate enough to remain in a “persistent vegetative state.” This state is characterized by a wakeful, reduced responsiveness with no evident cerebral cortical function. The vegetative state can result from diffuse cerebral hypoxia or from severe, diffuse white matter impact damage. The brain stem is usually relatively intact. Clients may track with their eyes and show minimal spontaneous motor activities that even appear purposeful, but they do not speak, nor do they respond to verbal stimulation.21 Life expectancy can be weeks, months, or years.22,23 Clients with brain injury who remain vegetative for 3 months rarely achieve an independent outcome. However, the term “persistent” should not be added to “vegetative state” until the injury has stabilized or the state has lasted for approximately 1 year.24 Functional magnetic resonance imaging (fMRI) was recently used to test clients who were diagnosed as being in persistent vegetative states. Five of 54 clients diagnosed as in a persistent vegetative state demonstrated “willful, neuroanatomically specific blood-oxygenated–level–dependent responses when told to visualize one of two tasks.”25 The diagnosis of persistent vegetative state indicates lack of cortical function, and fMRI may be useful in this diagnosis in the future. Recovery of consciousness, if it occurs, includes a gradual return of orientation and recent memory.19 The duration of each of these stages is variable and can be prolonged. Improvement can stop at any point. A list of the complications that may accompany brain injury would be limitless. In addition to any concomitant injuries, some of the diagnostic, monitoring, and therapeutic procedures themselves carry hazards. So does prolonged bed rest. Catheters, nasogastric tubes, and tracheotomies can cause iatrogenic injuries. Infections, contractures, skin breakdown, thrombophlebitis, pulmonary problems, heterotopic ossification (HO), and surgical complications are but a few of the risks. Posttraumatic epilepsy is also a possible sequela. Depression occurs frequently after brain injury, and it can alter functional outcome. It appears that a combination of neuroanatomical, neurochemical, and psychosocial factors are responsible for the onset and maintenance of the depression.26 Two types of amnesia are frequently associated with brain injury: retrograde and posttraumatic.28 Cartlidge and Shaw14 define retrograde amnesia as a “partial or total loss of the ability to recall events that have occurred during the period immediately preceding brain injury.” The duration of the retrograde amnesia may progressively decrease. Posttraumatic amnesia (PTA) is defined “as the time lapse between the accident and the point at which the functions concerned with memory are judged to have been restored.”14 The duration of PTA is considered a clinical indicator of the severity of the injury.14 An additional deficit can be the inability to form new memory, referred to as anterograde memory. The capacity for anterograde memory is frequently the last function to return after recovery from loss of consciousness.29 The client’s inability to develop continuing short-term memory can be quite frustrating for the rehabilitation team as well as for the client because memory is an important component of learning.30 There are two types of memory: declarative and procedural. Memory in which the client can recall facts and events of a previous experience is declarative memory. Explicit learning, a conscious verbal learning, is based on declarative memory. However, many clients who cannot reproduce memories through conscious recollection do have the ability to learn new motor skills. Implicit learning, a noncognitive type of learning in which clients can show changes in performance after prior experience, is based on procedural memory. Clients can show the ability to change motor, perceptual, or cognitive behaviors with practice or training but may lack declarative memory. That procedural memory may be present without declarative memory in clients with TBI has been demonstrated.28 On the client’s admission to the hospital, a neurosurgeon usually assumes initial and primary responsibility for the client. The first priority in medical care is resuscitation, after which baseline assessments are made and a history is obtained. Immediate surgery may or may not be indicated. Surgery is indicated when blood and necrotic tissue are present in the cranial vault. Early concerns may include the management of respiratory dysfunction, cardiovascular monitoring, treatment of raised ICP by means of pharmacological, mechanical, or surgical procedures,14 and general medical care. Examples of general medical care are familiar: maintenance of fluid and electrolyte balance, nutrition, eye and skin care, prevention of contractures, postural drainage, and safety considerations.6 The need for this type of care gradually lessens as the client responds, or it may continue if unconsciousness persists. Initially, a determination of Glasgow Coma Scale31 (GCS) score (Box 24-4) is performed to test the function of the brain stem and the cerebrum through eye, motor, and verbal responses. It provides a measure of the level of consciousness. Scores range from 3 to 15, with lower scores associated with lower levels of function. Scores from 13 to 15 indicate a mild brain injury, 9 to 12 a moderate brain injury, and 8 or less a severe injury. Several scales define TBI as mild, moderate, or severe based on specific measurements (Table 24-1). Because the definition of mild brain injury has varied so widely, the CDC convened a panel of experts to further define it. The new definition of mild TBI is an injury to the head (arising from blunt trauma or acceleration or deceleration forces) that results in one or more of the following: any period of confusion, disorientation, or impaired consciousness; any dysfunction of memory around the time of injury; loss of consciousness lasting less than 30 minutes; or the onset of observed signs or symptoms of neurological or neuropsychological dysfunction.2 According to the Brain Injury Association of America, with a moderate TBI the client experiences a loss of consciousness that lasts from a few minutes to a few hours; confusion that lasts from days to weeks; and physical, cognitive, or behavioral impairments that last for months or are permanent. A severe brain injury occurs when a prolonged unconscious state or coma lasts days, weeks, or months. With the possible exception of the diagnosis and hence prognosis of diffuse white matter impact damage,32 one third of clients hospitalized with brain injuries have extracranial injuries,6 which are explored with a physical examination and appropriate special tests. Additional testing depends on the client’s particular dysfunctions. CT,33 MRI, positron emission tomography (PET), radioisotope imaging, ventriculography, echoencephalography, electroencephalography, monitoring of ICP, measurement of cerebral blood flow and metabolism, monitoring of cardiorespiratory and cardiovascular function, and tests of cerebrospinal fluid and other biochemical studies all provide important information. Changes in electrocerebral potentials that occur in response to specific stimuli also are studied. Visual, auditory, and somatosensory evoked potential examinations are used with clients with brain injury but are more effective when combined with other examinations.34 These examinations make it possible to observe the presence, evolution, and resolution of a lesion.6 Reflex motor responses in unconscious clients are tested by applying a noxious stimulus, such as pressure on a nail bed with a pencil or supraorbital pressure, and observing the response. Most responses generally fall into three categories: appropriate, inappropriate, or absent.19 Testing for cognitive and behavioral functions is usually done via neuropsychological tests. In some circumstances the results of IQ tests, achievement tests, and Armed Forces tests may be available for comparison. Differentiating changes in cognitive and behavioral functions caused by brain injury from posttraumatic stress syndrome, conversion or hysterical reactions, malingering, depression, and anxiety is extremely important. TABLE 24-1 SEVERITY OF TRAUMATIC BRAIN INJURY Medications are chosen according to symptoms to be treated. Many of these recommendations are from a meta-analysis of management of severe TBI published in 2007.35–39 When ICP increases, changes in Pco2 are seen. The maintenance of a Pco2 at 30 to 40 mm Hg appears most appropriate. Osmotic agents such as mannitol are used to pull fluid from brain tissue back into the blood system, thus lowering ICP. Propofol, a barbiturate, is recommended for control of ICP if it cannot be controlled by other means.35 Use of mannitol is recommended for clients who have profusion problems.35 ICP has been lowered by intentional hyperventilation, which causes an increase in blood Pco2, resulting in vasoconstriction of the central vessels and reduced cerebral blood flow. However, Muizelaar and colleagues40 as well as information from the Traumatic Coma Data Bank41 showed that dramatically reducing a client’s Pco2 in this manner resulted in a worse outcome than that in clients managed with medication. Therefore hyperventilation is currently used only for nonresponsive cases and for short durations. Glucocorticoids (dexamethasone [Decadron], methylprednisolone [Solu-Medrol]) have been used to treat cerebral edema, but most studies show no long-term changes in outcome, and methylprednisolone is contraindicated because it increases mortality.39 See Chapter 36 for additional information. Blood pressure control is important in clients with brain injury. Cerebral perfusion pressure42 or adequate blood pressure to maintain cerebral blood flow against increased ICP is calculated by subtracting the ICP from the mean arterial pressure. If fluid management cannot keep the blood pressures elevated, then vasopressor drugs such as phenylephrine (Neo-Synephrine) are used to constrict peripheral vessels but not the vessels of the brain. Medications also may be prescribed for motor abnormalities involving increases in tone. Baclofen is now used more frequently with clients with brain injury; however, it can produce lethargy, confusion,43 and reduction in attention span44 in some clients. These effects are greatly reduced with implantation of a pump to deliver the drug. Dantrolene sodium is another medication used to decrease spasticity and rigidity. This drug works directly at the muscle level and therefore is less likely to cause cognitive disturbances but more likely to cause generalized weakness.45 Botulinum toxin type A (Botox) is widely used to inject into specific muscles, such as the finger flexors, biceps, or gastrocnemius, to decrease their tone. Diazepam (Valium) initially was the drug most commonly administered for spasticity or high tone. However, diazepam also promotes drowsiness and decreased responsiveness and can increase muscle weakness and ataxia.43 These side effects actually hinder rather than assist in rehabilitation. Glenn and Wroblewski44 conclude that “rarely, if ever, are the benefits of diazepam’s antispasticity effect great enough to justify its use in the brain-injured population.” Drugs to treat behavioral or cognitive dysfunction have not been particularly successful. Antidepressive drugs as well as carbamazepine (Tegretol) and propranolol (Inderal) have been used to treat aggression and agitation. Carbamazepine appears to reduce agitation or aggression in clients with brain injury.46 Confusion and other neuropsychotic symptoms have been treated using neuroleptic medications. A recent review article suggests that these drugs may negatively affect motor outcomes.47 Sedative drugs prescribed in an attempt to control delirium may add to the client’s confusion and may also contribute to a decreased responsiveness. Later in the rehabilitative process, various antidepressants may be used to treat aggressive and disruptive behaviors. These, too, may have deleterious side effects. Antidepressants other than the tricyclics appear to be the most effective for treating depression. Hypothermia is frequently used in acute severe TBI. Although it does not appear to change the mortality rate, it is associated with improved functional outcome on the Glasgow Outcome Scale (GOS) (Box 24-5).36
Traumatic brain injury
Overview of brain injury
Epidemiology of traumatic brain injury
Population of clients with brain injury
Mechanisms of injury
Pathophysiology of injury
Primary damage
Secondary damage
 Increased intracranial pressure (ICP) (resulting from swelling or intracranial hematoma). Swelling of the brain causes distortion because the brain is held in the skull, a rigid, unyielding structure. The resultant increased ICP can lead to herniation of parts of the brain. The most often seen herniations include cingulate herniation under the falx cerebri, uncus herniation, central (or transtentorial) herniation, and herniation of the brain stem through the foramen magnum.11 Acute hydrocephalus occurs when blood accumulates in the ventricular system, expanding the size of the ventricles and causing increased pressure on brain tissue being compressed between the skull and the fluid-filled ventricles. The increased pressure can then result in changes in Pco2, which is also harmful to nervous tissue. Increased ICP has been correlated with poorer outcomes and higher mortality rates.12
Increased intracranial pressure (ICP) (resulting from swelling or intracranial hematoma). Swelling of the brain causes distortion because the brain is held in the skull, a rigid, unyielding structure. The resultant increased ICP can lead to herniation of parts of the brain. The most often seen herniations include cingulate herniation under the falx cerebri, uncus herniation, central (or transtentorial) herniation, and herniation of the brain stem through the foramen magnum.11 Acute hydrocephalus occurs when blood accumulates in the ventricular system, expanding the size of the ventricles and causing increased pressure on brain tissue being compressed between the skull and the fluid-filled ventricles. The increased pressure can then result in changes in Pco2, which is also harmful to nervous tissue. Increased ICP has been correlated with poorer outcomes and higher mortality rates.12
 Cerebral hypoxia or ischemia (occurring when blood vessels are ruptured or compressed). Hypoxia can occur from a lack of blood to the brain or from lack of oxygen in the blood as a result of airway obstruction or chest injuries.
Cerebral hypoxia or ischemia (occurring when blood vessels are ruptured or compressed). Hypoxia can occur from a lack of blood to the brain or from lack of oxygen in the blood as a result of airway obstruction or chest injuries.
 Intracranial hemorrhage causes hypoxia to tissues fed by the hemorrhaging blood vessels and adds pressure and distortion to brain tissue. Metabolic products from damaged cells and blood bathe the brain. Cell death occurs within minutes after injury from ischemia, edema, necrosis, and the toxic effects of blood on neural tissues.
Intracranial hemorrhage causes hypoxia to tissues fed by the hemorrhaging blood vessels and adds pressure and distortion to brain tissue. Metabolic products from damaged cells and blood bathe the brain. Cell death occurs within minutes after injury from ischemia, edema, necrosis, and the toxic effects of blood on neural tissues.
 Electrolyte imbalance and acid-base imbalance. Secondary cell death occurs either by swelling and then bursting of the cellular membrane (necrosis) or by destruction from within the cell through changes in the deoxyribonucleic acid (DNA) (apoptosis). Cell death can occur days, weeks, or months after injury.13
Electrolyte imbalance and acid-base imbalance. Secondary cell death occurs either by swelling and then bursting of the cellular membrane (necrosis) or by destruction from within the cell through changes in the deoxyribonucleic acid (DNA) (apoptosis). Cell death can occur days, weeks, or months after injury.13
 Infection from open wounds. Infection in brain tissue may cause swelling and cell death.
Infection from open wounds. Infection in brain tissue may cause swelling and cell death.
 Seizures from pressure or scarring. Seizures are most common immediately after injury and 6 months to 2 years after injury. The seizures can cause additional brain damage owing to high oxygen and glucose requirements.
Seizures from pressure or scarring. Seizures are most common immediately after injury and 6 months to 2 years after injury. The seizures can cause additional brain damage owing to high oxygen and glucose requirements.
Physiological, cognitive, and behavioral changes after brain injury
Autonomic nervous system
Motor, functional, sensory, and perceptual changes
Cognitive, personality, and behavioral changes
Changes in consciousness and coma
Concussion.
Coma.
Persistent vegetative state.
Other complications
Amnesia.
Memory.
Initial care and medical interventions

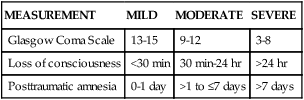
MEASUREMENT
MILD
MODERATE
SEVERE
Glasgow Coma Scale
13-15
9-12
3-8
Loss of consciousness
<30 min
30 min-24 hr
>24 hr
Posttraumatic amnesia
0-1 day
>1 to ≤7 days
>7 days
Pharmacological interventions
Drugs that decrease intracranial pressure.
Drugs that control blood pressure.
Drugs that affect the motor, behavioral, and cognitive functions (see chapter 36).
Prevention of brain cell death.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





















































