PHYSIOLOGY
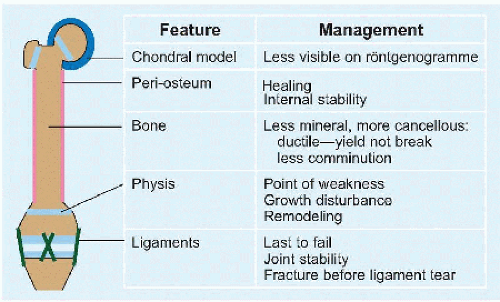
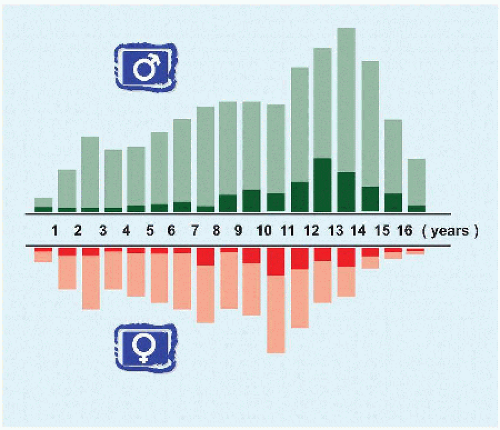
Children’s bones differ from those of adults [C]. The differences and consequences diminish with age, so that during adolescence, treatment approaches that of the adult.
Growth Plate
The growth plate, or physis, is the most distinctive feature of a child’s skeleton. It adds to the risk of growth disturbance. It is weaker than bone, which is weaker than ligament [D]. It is most vulnerable during periods of growth acceleration, such as puberty. It enables remodeling [E].
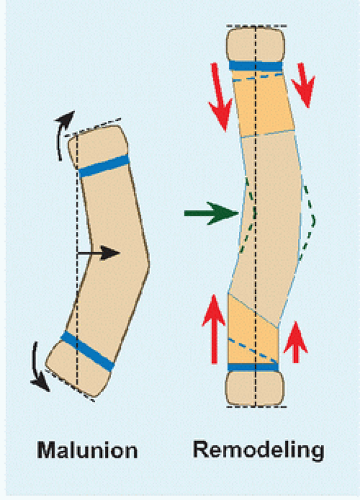
Remodeling This refers to correction of a malaligned bone with growth [E]. This consists of two principal components:
Differential growth at the physis, which accelerates on the concave side
Differential growth at the fracture, which shows periosteal laying down of bone by apposition in the concavity and bone resorption on the convexity of the apex of deformity
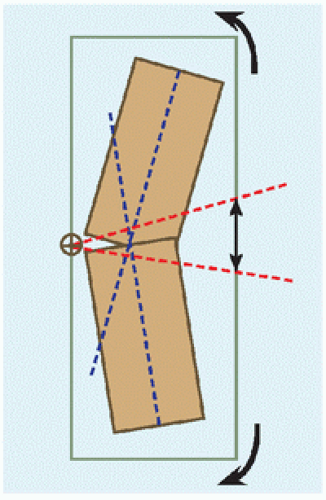
Remodeling rectifies epiphysial and articular orientation, as well as the mechanical axis. Several factors influence remodeling:
While 2 years of growth remaining may be regarded as a requirement for remodeling, the process is more predictable for fractures occurring in the first decade than in the second decade.
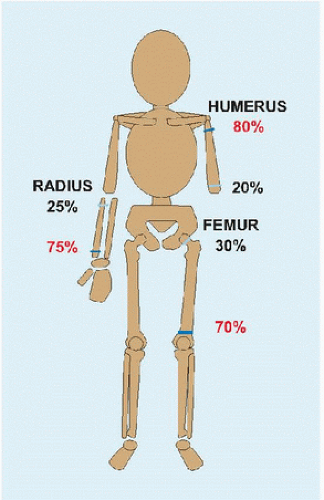
Growth of the bone. Physis that are more active are more potent. The greatest percent growth of bone occurs at proximal humerus more than distal radius more than distal femur [F]. As a result, greater displacement of fractures of proximal humerus and distal radius may be accepted: remodeling substitutes for reduction [G].
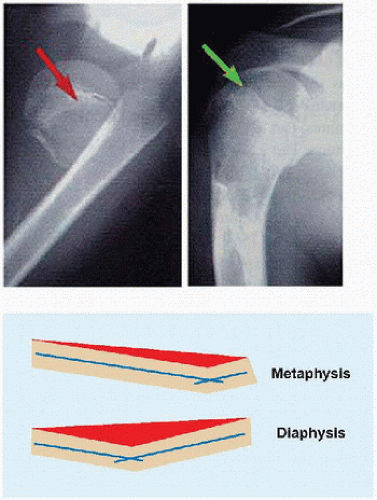
Location of fracture within a bone. More remodeling is required in the diaphysis than in the metaphysis [H]
Plane of joint motion. Forces that stimulate new bone formation are greatest in the plane of motion (Wolff law). In addition, an enarthrodial joint can accommodate greater residual deformity than a more restricted joint, such as a ginglymus, which can accommodate only in the sagittal plane of motion.
Duration of acute remodeling, which is the period of observation before intervention for malunion, is typically 1 year but occasionally up to 2 years, for example, proximal metaphysis of tibia fracture.
Injury Physis are located adjacent to an epiphysis, which is a secondary ossification center that forms the articular surface of a bone “on top” (Greek επι-) of the physis, and an apophysis, which grows “away” (Greek απο-) from the physis to serve as a site of attachment of a muscle. Injuries to and displacement of the former are less tolerated than are the latter. Ligaments attach to epiphysis, thereby concentrating force during joint motion at the physis, which increases risk of injury.
Growth disturbance occurs most frequently from trauma and infection. Infection typically results in a diffuse zone of injury. Trauma may do the same, as in a crush mechanism, or it may produce a discrete bridge of bone: displacement brings metaphysis from one side into contact with epiphysis on the other side, which unite. Injury also may stimulate a growth plate to overgrow. This is most striking in the femur and may be related to hyperæmia.
Force of fracture travels through the hypertrophic zone, because this is the level of highest stress concentration between the zone of provisional calcification adjacent to metaphysis and the proliferative and germinal zones adjacent to epiphysis. Growth will resume after fracture provided the blood supply is preserved, and there is no mechanical disruption of the rest of the physis. The latter may occur at an undulating or otherwise irregular physis, such as the distal femur or distal tibia, where “Poland hump” may act as a spike to tear across the proliferative and germinal zones. The distal physis of tibia also is vulnerable due to force concentration of body weight over a relatively small area. This may explain injury to the tibial apophysis, where force of quadriceps is concentrated.
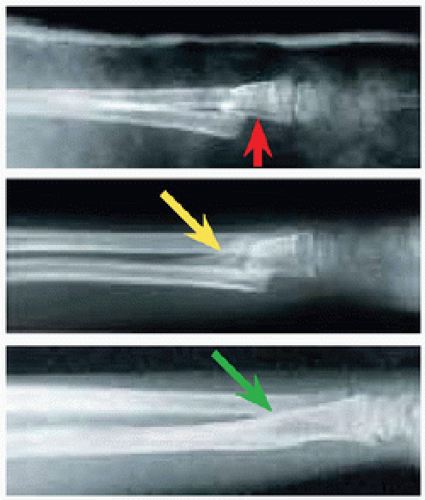
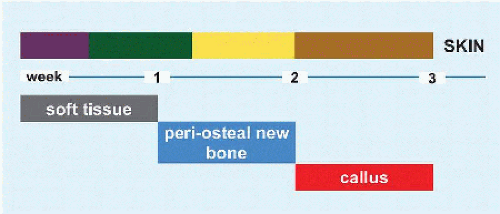
Injury may be marked on bone by a growth arrest line (Harris) [I]. This represents condensation of mineral due to temporary growth arrest locally after fracture or diffusely after a generalized severe illness. Date of injury may be calculated based upon distance from physis and physial rate of growth. Slowing or arrest of growth is indicated by a reduction of distance. Partial growth disturbance is suggested by obliquity of the line relative to the physis, suggesting asymmetric growth by an unhealthy physis.
Bone
Reduction in mineralization with a more collagenous extracellular matrix, and a larger proportion of cellular component, result in a more ductile material that can buckle when stressed [J] or plastically deform [K] and that resists fragmenting into multiple pieces. The lag in mineralization behind longitudinal growth renders immature bone more porous and thereby more susceptible to injury.
Periosteum
This is more metabolically active in the child than in the adult. It does not tear as readily, leaving continuity for new bone formation. This explains the exuberant callus seen in the infant and the rapid union and increased potential for remodeling seen throughout childhood. The periosteum is thick. The structural integrity of a child’s periosteum adds internal stability to fractures. However, it also may interfere with reduction and growth if it becomes entrapped within a fracture.
Ligaments
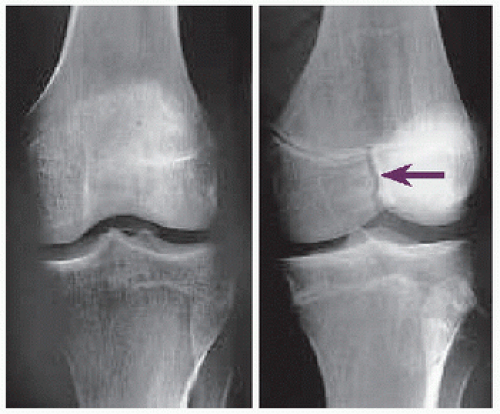
In a child, ligament is stronger than bone, which is stronger than physis [L]. Ligaments, and perichondrium, protect a physis they span from displacement. Ligaments resist failure such that they do not tear but rather transmit force to dissipate in an avulsion fracture [M]. Chondral Model An increasing proportion of the skeleton, growing by endochondral ossification, is invisible on röntgenogramme with decreasing age. Early on, landmarks may be absent. Later, articular fragment size may be underestimated, as typified by the patellar sleeve fracture [M].
CLASSIFICATION
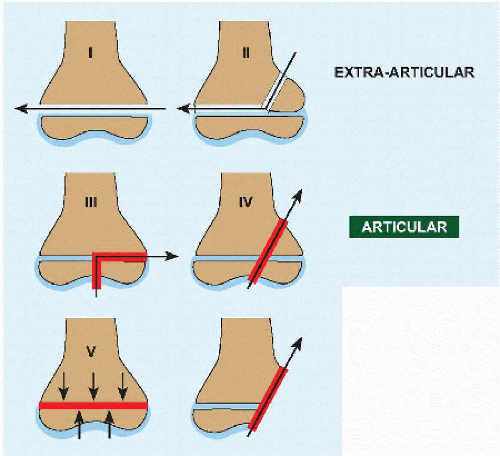
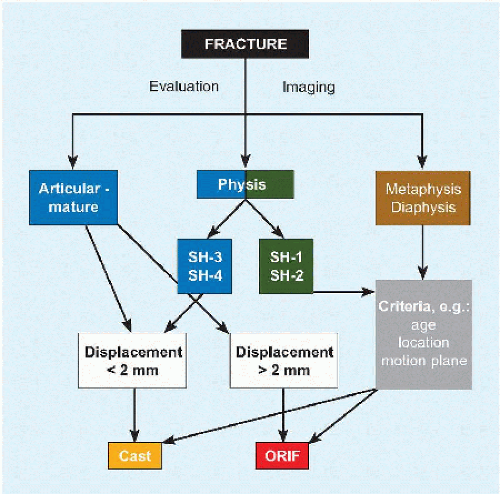
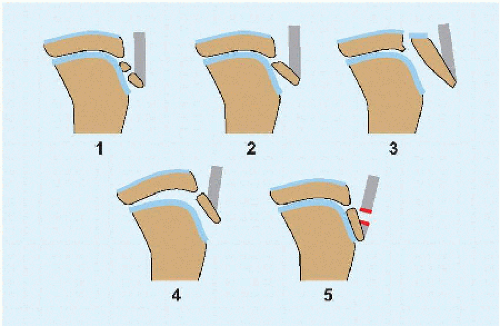
There are several classifications of pædiatric fractures. In the most accepted system [A], fractures are divided into five categories based upon pattern and mechanism, as evaluated by röntgenogramme. Type V is rare and identifiable only in retrospect, when compression of the physis has led to growth disturbance. The first four types may be divided into two groups, extra-articular or articular, thereby dividing fractures into those which risk growth and those which risk growth and osteoarthritis. The two groups also may be distinguished by operative rate. Physial fractures are managed according to criteria for acceptable displacement that vary according to site; most are treated nonoperatively. Articular fractures are treated according to universal principles, which do not accept >2-mm step-off in order to minimize risk of osteoarthritis; as a result, most are treated operatively.
EVALUATION
Up to 15% of fractures in children are missed or misdiagnosed at first evaluation. Individual fractures will be addressed separately.
Physical Examination
Pseudoparalysis refers to refusal to use a limb because of pain. The upper limb is held suspended as if paralyzed. The child refuses to bear weight on the lower limb. Because the child comes with parents, and both may be distressed, there is pressure not to disturb the child any more than already has been done, by injury, by those enlisted to help at the scene, by transportation to a medical facility, and by others who already have examined the child. Be thorough, for example, do not miss an open wound covered by a splint. Be persistent: management of a postoperative neural deficit after reduction and fixation of a supracondylar humerus fracture is predicated on knowledge of the preoperative function.
Divide type I open fractures into outside-in and inside-out [A]. The latter is produced by the osseous fragment pushing through the skin from a clean environment, rather than in the former case, where contamination from the outside may be introduced into the fracture. Inside-out open fractures may be washed in the emergency setting, treated with a single dose of antibiotics, and treated as though closed with close observation. After cast application, cut a window in the cast to make the lesion visible for follow-up. All other open fractures are managed according to general principles. The window for surgical débridement may be opened to 24 hours in children.
Compartment syndrome in children is not as fulminant as in adults. Bleeding raises compartment pressure, producing a tense limb that hurts. Increasing pressure, exacerbated by capillary leaking, first occludes venous outflow and only later occludes arterial flow to produce pallor, pulselessness, and paræsthesias. Have a high index of suspicion, for example, after supracondylar humerus fracture. While this is a clinical diagnosis first and foremost, data may be necessary in children when their presentation may be mild [B]. Delay in diagnosis is not unusual, but this is mitigated by the fact that full recovery may be expected up to 36 hours after injury. Distinguish exertional compartment syndrome (cf. Sports chapter).
Imaging
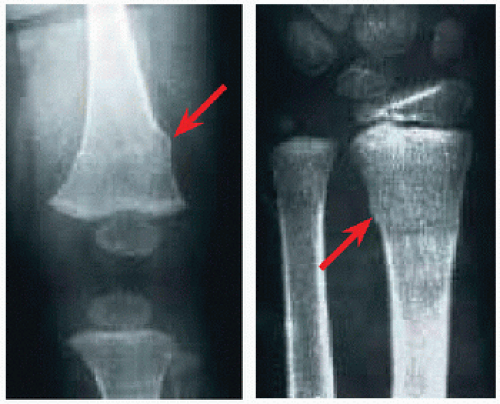
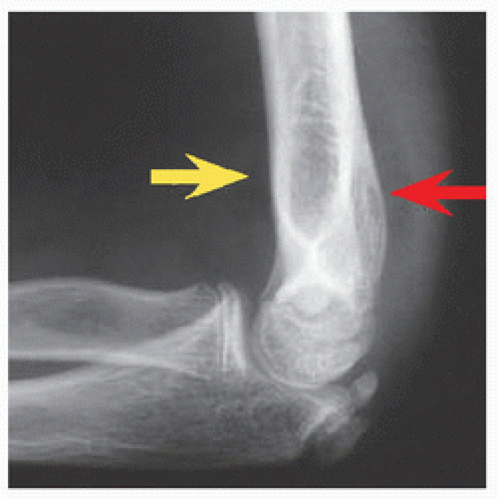
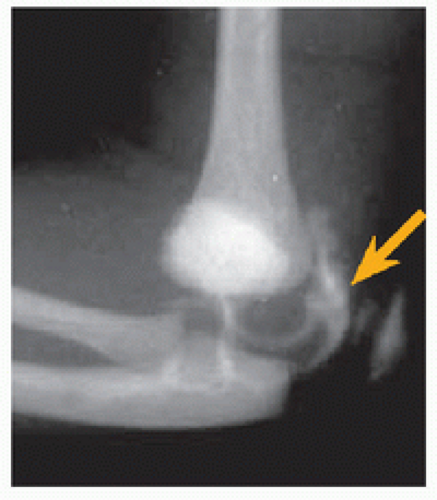
Röntgenogramme This is the mainstay of trauma imaging. In addition to anteroposterior and lateral projections, special views may be helpful, for example, oblique for condylar fractures [C] and mortise of the ankle. Beware of TRASH: The Radiologic Appearance Seemed Harmless. The term encompasses osteochondral lesions that may be incompletely visible on this imaging modality. These typically occur in the first decade. The elbow is a rich source, due to the multiple ossification centers with varying appearance, such as an epiphysial separation in the infant, a displaced intra-articular medial condyle fracture, or radiocapitular subluxation. Occult injuries may manifest secondarily in soft tissue, for example, the sail sign at the elbow [D]. Imaging the contralateral uninjured side may be helpful in the setting of atypia, such as a skeletal dysplasia.
Arthrogram This outlines the articular surface when affected by fracture and unossified [E]. In addition to aiding diagnosis, this modality may influence operative decision making and may be used to confirm acceptability of reduction of articular fractures, for example, of the lateral condyle of humerus (q.v.).
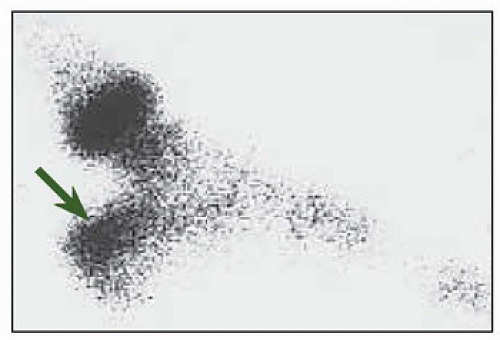
Scintigramme This also is useful for röntgenographically occult injury. In a child who refuses to bear weight on the lower limb or in whom the physical examination is nonlocalizing, scintigramme may reveal an injury and focus the evaluation.
Computed Tomography This is most useful to evaluate an articular fracture, to most accurately measure interruption of the surface. While outcome studies have suggested that >2 mm of articular step-off on röntgenogramme significantly increases the risk of posttraumatic arthritis in certain joints, for example, wrist and ankle, this rule has been extrapolated widely to all joints and to CT, which is a more sensitive modality. There is no consensus on diastasis without step-off. CT also aids preoperative planning, for example, to determine location of fixation in a triplane ankle fracture.
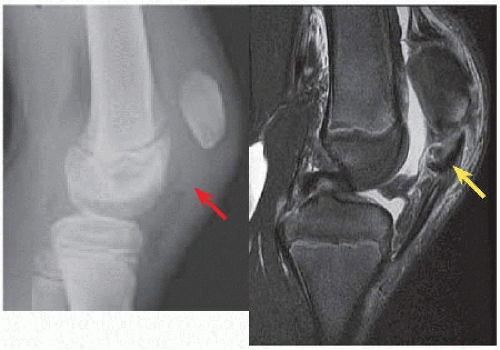
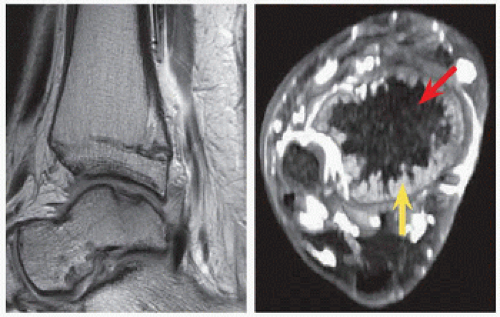
Magnetic Resonance Imaging Use judiciously, as this modality requires sedation of a first-decade child. MRI is most useful to evaluate associated soft tissue injury, such as in the setting of spine fracture in order to evaluate the neural elements, or at the knee in order to rule out meniscal tear in the setting of intercondylar eminence of tibia fracture. MRI often is utilized for complications and preparation for reconstruction, for example, mapping of a physial bridge or determination of presence and extent of osteonecrosis of the head of femur.
Ultrasonogramme This is inexpensive, nonradiating, portable, and facile in the outpatient or emergency setting where it may be performed by the surgeon; is not stressful; and asks little of the child. It is useful for diaphysial fractures, where its specificity may be relied upon in decision to image further. The imprecision of ultrasonogramme around physis and joints limits its utility and influence on management.
MANAGEMENT
Cast
This is safe and inexpensive and has long experience to support it. Not as relevant to children as they are in adults are concerns about joint stiffness and interference with activities such as mobility and work. Despite this, operative treatment for children’s fractures is on the rise [A]. Fiberglass is becoming the standard because it is less messy and lighter.
A splint may be applied at the initial encounter, for example, emergency department, if operation is anticipated or if the limb must remain accessible for observation, for example, swelling.
Position the patient, and assistant, appropriately. A stockinette may be folded to soften cast edges. For width of padding, balance risk of pressure sore against loss of reduction. Focus padding over prominences, for example, malleolus; over other areas of stress concentration, for example, cast edges; and where a saw will cut the cast, for example, “racing strips” along anticipated path of saw, at time of cast removal. Extensor transitions may be angled, to limit sliding of the limb in cast, for example, right angle at posterior elbow; by contrast, flexor transitions must be smooth, for example, in the antecubital fossa, to avoid soft tissue injury.
Roll—do not stretch—cast material, in order not to compress the muscle compartments. Open casts, for example, “bivalve,” if swelling is anticipated. Cut the padding as well if bleeding is anticipated, as blood will harden padding risking a circumferential constriction.
A waterproof cast is attractive to patients: it allows bathing but requires care to dry. It may give a conflicting signal to a child who has been instructed in protected weight bearing yet is allowed to swim with a cast.
Wedge a cast for fragment drift [B].
A plaster cast may be soaked off. Plaster and fiberglass casts typically are sawed off. The saw has a blunt blade that breaks a cast and as such will not cut skin it touches transiently. Gain the child (and the parent’s) confidence by demonstrating on your finger and inviting the child to try. The blade heats as it works, thereby risking skin burns that may leave a permanent scar. Insert plastic strips where there is access to protect the skin. Stop periodically and cool the blade. Renew the blade regularly. Do not dwell: push in, pull out, and keep moving.
Fixation
Use enough fixation. If mobilization is not imperative, supplement with a cast, which may allow simpler and less morbid fixation, for example, inserted percutaneously and removed in the clinic. The soft tissue envelope, including periosteum, is robust, and the energy of injury is more likely low compared with adults. As a result, children’s fractures have inherent stability, which, along with more rapid and reliable healing, allows for less invasive and less rigid fixation, for example, elastic nails instead of plates.
The articular surface is more important than the physis: do not sacrifice reduction and stability for concerns about growth disturbance. Osteoarthritis has no simple solution, whereas much can be done about growth disturbance. Furthermore, implants (even threaded) may be placed across a physis so long as their cross-sectional area is small, the physis is not dissected (extraperiosteal, extrachondral), and they are removed within 2 years (before the physis gives up growth).
Remove plates applied in the first decade. Periosteal appositional growth will make them intraosseous by maturity. Do not remove before 6 months, in order to minimize refracture. External fixators produce ugly scars. Their rigidity and any distraction at the fracture may delay union: do not remove them before there are at least three continuous cortices of bone. As with frames for lengthening, remove the barrel and let the child bear weight, with or without a cast, for 2 to 4 weeks. In the event of a refracture, the barrel may be applied in a reduced position.
Bend smooth wires with a long tail over the skin; otherwise, the skin will overgrow them. Save a child an anæsthetic by pulling wires in the clinic, even those placed medullary in the forearm. Deep infection is rare: irritated entry sites usually recover after wire removal. Figure C represents an algorithm for management.
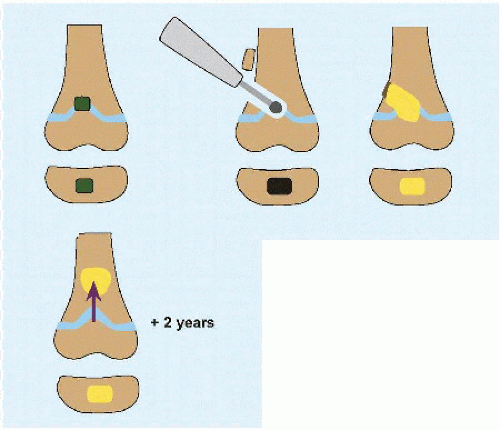
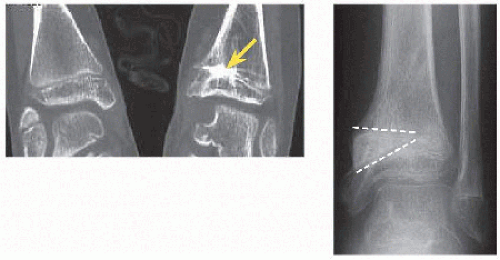
PHYSIAL BRIDGE
Growth disturbance after fracture may be due to chondrocyte injury in germinal or proliferative zones of the physis, or it may be due to a bridge (or bar) of bone forming across and tethering the physis. The former is remediable by secondary reconstruction, such as limb lengthening to compensate for growth arrest. The latter may be treated directly by bridge resection.
Small bridges may lyse spontaneously. Central bridges are more likely to lyse and less likely to cause deformity than peripheral ones. Central bridges may cause a fishtail deformity, which is better tolerated in the distal femur [A], where it results in a lower limb-length discrepancy, than in the distal humerus, where it is associated with elbow stiffness. Peripheral bridges produce angular deformity [B].
Time for growth is necessary for a disturbance to manifest. Educate patients about alignment of limb or joint, and follow up patients at risk through the anniversary of fracture. Röntgenographic findings include angulation after healing, asymmetric Harris growth arrest line, and limblength discrepancy. MRI maps the physis to localize and aid determination of the extent of a bridge [C]. This modality may reduce zeal for resection, and thereby improve outcomes of resection, by giving a more accurate (and realistic) representation of the physis.
Resect bridges that occupy <25% to 50% of the physis and in a child with ≥2 years of growth remaining [D]. Outcomes are related to the size of the bridge and the health of the adjacent physis. Growth acceleration after peripheral bridge resection may correct angular deformity ≤10 degrees [E]. For greater angular deformity associated with a bridge, combine with a corrective osteotomy, which facilitates access to the bridge for resection.
If the physial bridge exceeds 50%, complete physiodesis is indicated. For angular deformity, osteotomy may be performed through the physis, where a structural graft may be placed to accomplish both goals of physiodesis and correction. Residual limb-length discrepancy is managed according to general principles (cf. Lower Limb chapter).
NONACCIDENTAL TRAUMA
The original report emphasized skull fracture and multiple fractures in various stages of healing (Caffey). The New York Society for the Prevention of Cruelty to Children was founded in 1874 as the world’s first child protective agency. The Federal Child Abuse Prevention and Treatment Act was established in 1974. One-third of abuse is neglect and 1/3 is physical injury, with the final 1/3 including sexual, emotional, and other causes.
The magnitude of the problem is arresting. Prevalence is 1%. Most abuse occurs in the first 3 years of life: 1/2 are <1 year and 1/4 are 1 to 3 years. Abuse accounts for 3/4 of fractures <2 years. After initial presentation, risk of repeat abuse (morbidity) is 1/3, while risk of death (mortality) is up to 10%.
Evaluation
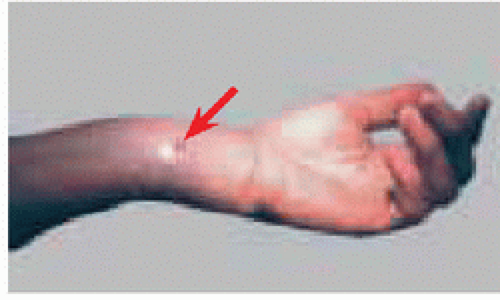
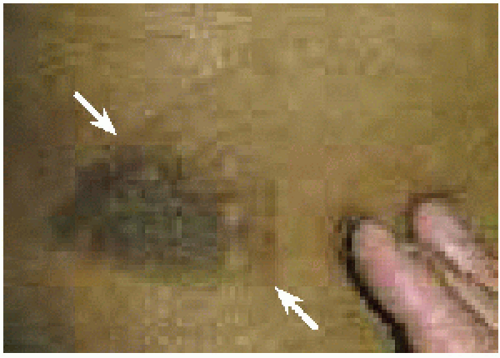
Have a high index of suspicion, and be swayed only by objective findings, for example, not by socioeconomic level. Note that an abuser will seek attention at different facilities for repeat events. Infant prematurity, parental youth, and unmarried status are risks factors. The skin tells the story: cutaneous lesion is the most common finding [A], including burns and bruises. Bruises turn purple (0 to 3 days), then green-yellow (3 to 7 days), and then yellow-brown (after 1 week) [B]. Scalds spare inguinal and popliteal regions due to reflex flexion of hips and knees. One-third of children will have head injury.
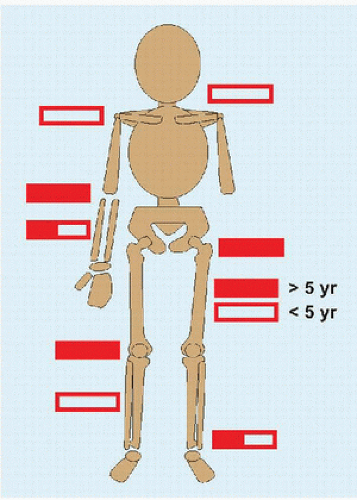
Fractures may be categorized according to specificity for nonaccidental trauma [C]. The corner fracture is nonaccidental a priori. The differential diagnosis list includes osteogenesis imperfecta (in particular type IV, which does not have the distinctive blue sclerae), osteomyelitis, infantile cortical hyperostosis, leukæmia, hypervitaminosis A, and rickets.
Imaging
Röntgenogrammes are the standard, ordered per protocol: both views of chest and skull; anteroposterior views of arms, forearms, hands, pelvis, thighs, and legs; and lateral view of spine [D]. Scintigramme surveys the skeleton and may expose fractures in difficult to image locations in a young child with incomplete ossification. False-negative rate for röntgenogramme approaches 10%, whereas for scintigramme, it is 1%.
Management
Most important is safety of the child: consult other providers, including pædiatricians, who may admit a child to complete an evaluation, and social workers, who understand how to interface with governmental agencies.
FOOT
Foot fractures account for 5% of children’s fractures, yet rarely is there an indication for operation. Half involve the metatarsal bones.
Toe
Hallux fracture may involve avulsion of the nail plate and injury to the nail matrix, which may be flipped into a physial separation as indicated by persistent displacement despite reduction. Treat this open injury with irrigation, open reduction, and smooth wire fixation. Lesser toe injuries may be displaced such that they require reduction and buddy-tape immobilization.
Metatarsal
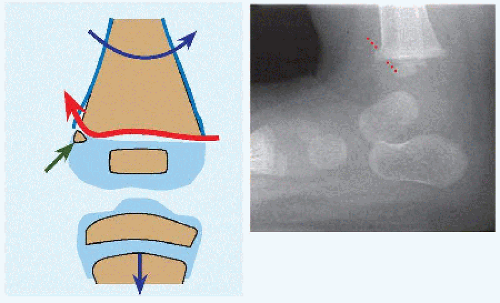
Fall from a height, such as a bunk bed, may result in a pædiatric equivalent of Lisfranc injury. This is characterized by a flexion and axial force that drives the medial cuneiform into the first metatarsal to second metatarsal interspace, creating a lateral proximal Salter-Harris IV fracture of the first metatarsal [A]. Reduce if necessary, fix with wires, and immobilize in a cast.
Stress fractures in adolescents are diaphysial and heal uneventfully with protection and immobilization [B].
The base of the fifth metatarsal presents several patterns:
Apophysitis or avulsion. The radiolucent apophysial cartilage is oriented longitudinally. This occurs under pull of peroneus brevis in a prepubescent child, who presents with tenderness and swelling. Protect weight bearing and immobilize in a cast.
Accessory ossicle. Do not confuse this with fracture (cf. Foot chapter). This is rounded, with an orientation if determinable that is oblique.
Metaphysial-diaphysial fracture [C]. Jones described this in himself after a night out dancing with his wife. Mechanism is inversion with abrupt traction by a peroneus brevis that attempts to rectify the foot. The fracture, which is transverse, occurs at a vascular watershed zone, hence the risk of delayed or nonunion. Most heal in a cast. Consider percutaneous screw fixation in a mature adolescent or for delayed union: use at least a 4.5-mm screw that fills the medulla to obtain internal cortical purchase.
Compartment Syndrome
A medial incision that takes down abductor hallucis, the “door to the cage” (Henry), gives access to the deep muscles of the foot. Add two longitudinal dorsal incisions.
Tarsus
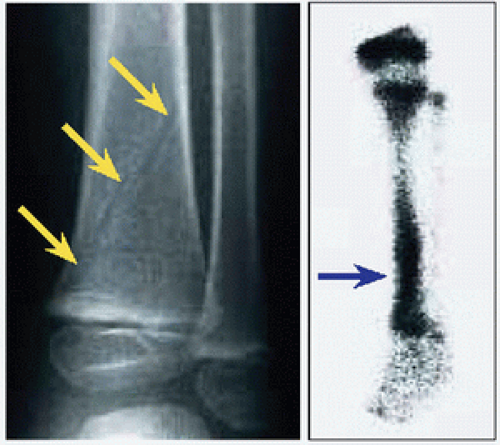
Fractures in this region represent <5% of foot fractures in children. These are treated according to general principles. Complications, for example, of head of talus after neck fracture, and comminution, for example, of calcaneus fracture, are less frequent in children. Beware of an occult injury producing limp in the young child [D]. Scintigramme may reveal a stress fracture when physical examination demonstrates foot tenderness, yet röntgenogramme is normal.
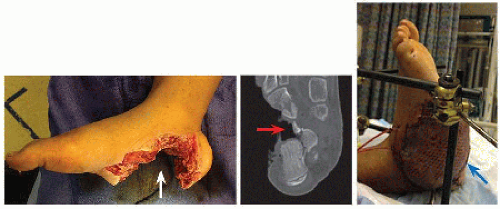
Soft Tissue
The burden of soft tissue injury for fracture in the child’s foot is relatively high due to mechanism of use of the foot, for example, running and jumping, on the ground, and due to mechanisms of injury, for example, lawn mower. Such injuries require complex reconstruction [E].
ANKLE
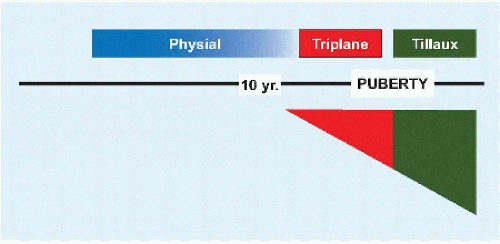
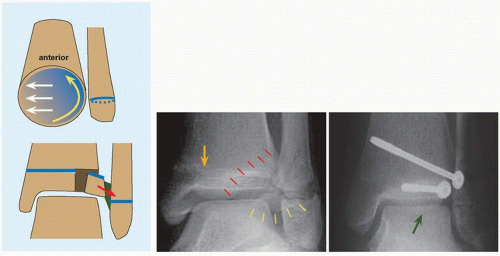
The distal physis of tibia closes by 15 years in girls and 17 years in boys. On mortise view röntgenogramme, there should be ≤8 mm clear space between tibia and fibula, and ≥1 mm overlap of tibia and fibula. Acceptable limits for talar position are <2 mm shift and <5 degrees tilt. The child is vulnerable to physial fractures at the ankle because all the ligaments that bind the joint attach to the epiphysis. Ankle fractures in children may be divided into physial and transitional [A].
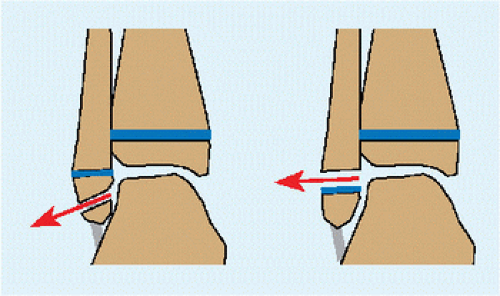
Physial Fracture
These occur before puberty, when physis are wide open. Avulsion fractures of fibula rarely require reduction and fixation [B]. Persistent fragments that do not unite may require delayed osteosynthesis if large, or excision. Do not confuse accesoria, for example, os subtibiale (up to 20% of children), with avulsions: the former are rounded with no matching surface on the main fibula fragment.
Salter-Harris I fractures of the distal fibula are a presumptive diagnosis based upon history of trauma, physical examination showing tenderness and swelling, and normal röntgenogrammes. They are overdiagnosed: most represent a bone contusion or ankle sprain. Immobilize without or with weight bearing until resolution of pain.
Several patterns are possible [C]. Salter-Harris II fractures may be displaced, for example, posterior with a metaphysial fragment by an ankle extension force. Intact ankle ligaments secure the distal fragment. Rest the heel on a firm platform, and apply the reduction force to bring the leg to the distal fragment: this will permit greater force than can be applied by holding the heel, in order to effect a single and as complete as possible reduction. The broad physial surface makes the reduction stable. Up to 10 degrees of residual angulation of tibia is acceptable if there is 2 years growth remaining. Associated fibula fractures may be left alone or stabilized with a percutaneously placed medullary wire, which acts as an internal splint. Residual gapping at the fracture represents soft tissue involution, in particular periosteum, which has been implicated in growth arrest. Educate the patient and family that, despite the apparent benignity of this type of fracture (including management by closed methods), growth arrest occurs in 1/4 of cases, exposing the fragility of this physis.
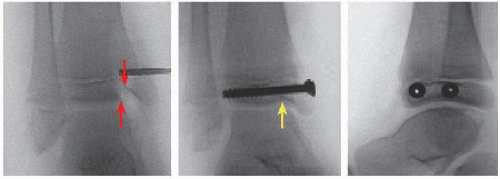
Salter-Harris III and IV are articular. If articular step-off is >2 mm, open reduction and internal fixation are indicated [D]. If the articular surface is not clearly delineated on röntgenogrammes (including oblique views), CT will allow accurate measurement. The surgical approach depends upon the fracture pattern. Plan incision(s) to include a direct view of the articular margin, for example, anteromedial approach to the tibial malleolar fragment. Irrigate the joint to wash out any osteochondral fragments too small to fix. Clean the fracture to remove débris that would obstruct anatomic reduction, including a periosteal flap. Palpate the articular surface with a blunt instrument to confirm that the marginal read is accurate. Fixation includes two screws in epiphysis to stably restore the joint. Excise the metaphysial fragment and overlying periosteum. The fragment is not essential for stability or union, and its removal is an anticipatory bridge excision, which will develop in up to 1/3 of cases [E].
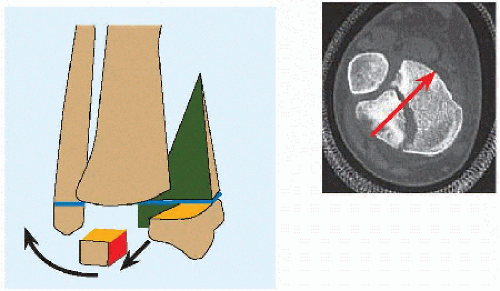
Transitional Fracture
This occurs during the transition between immaturity and mature child, as the distal physis of tibia undergoes the process of closure. As a result, growth disturbance is not a concern. This represents 10% to 15% of pædiatric ankle fractures.
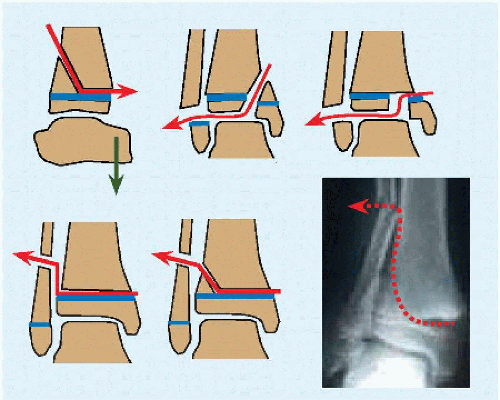
Triplane This fracture is so named after the three planes through which force travels: sagittal disrupts the articular surface, transverse shears the physis, and coronal produces a posterior metaphysial spike [F]. It may be medial or lateral, two-part, three-part, or four-part, presenting numerous patterns and variants that evade a useful classification. The fundamental mechanism is lateral rotation of the ankle, which may be divided into three stages: the first produces an ankle sprain or Tillaux fracture (vs.), the second produces a triplane fracture, and the third stage produces a fibula fracture in half of cases. Because of their complexity, CT is essential to plan fixation, including location of incisions and implant direction. Restore length to take advantage of desmotaxis by fixing the fibula if fractured [G]. Build the distal tibia by starting at the epiphysis. Add fixation, for example, anteroposterior screws, to capture the posterior metaphysial spike, as necessary to reduce the epiphysis to the remainder of tibia. Add a screw to fix the syndesmosis if disrupted. Beware that soft tissue swelling may influence timing of operation.
Tillaux The pathogenesis reflects direction of closure of the distal physis of tibia: this begins central, proceeds medial, turns posterior, and ends at the anterolateral corner, which will be separate and due to stress concentration prone to avulsion under pull of anterior tibiofibular ligament during lateral rotation of the ankle [H]. Unlike the triplane fracture, which is characterized by significant deformity as the distal epiphysis of tibia breaks and separates from the rest of the bone taking with it the foot, a Tillaux fracture presents with no significant deformity and minimal swelling. Tillaux patients are 1- to 2-year older than triplane patients. Because ankle alignment is normal, this fracture may not be evident on röntgenogramme, in particular on anteroposterior projection, in which fibula obscures lateral corner of distal tibial physis. Because of this, and the fact that it is articular, CT is indicated. For displacement >2 mm, perform open reduction via an anterolateral approach that enables inspection of the articular surface. Reduction of the fragment requires simultaneous compression with pointed tenaculum and posteromedial translation with tamp. Fix with one screw parallel to the articular surface and one oblique for rotational control. Do not worry about the physis, which by definition is mostly closed.
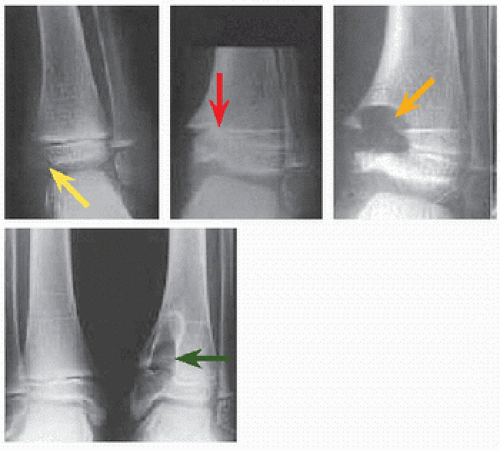
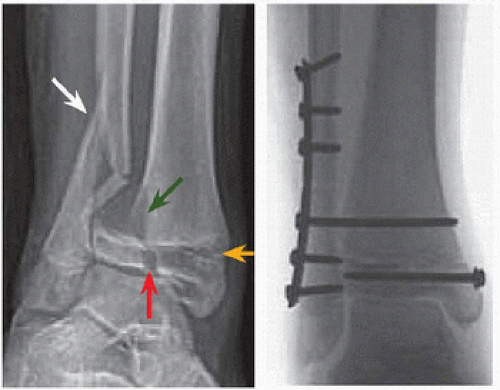
TIBIA
The subcutaneous surface of the tibia makes it slow to heal and prominent when malunited. Unlike femur, overgrowth is insignificant: mean 5 mm up to 10 mm. The tibia bears 80% of body weight through the leg. Compartment syndrome is a real risk after this fracture.
Toddler fracture
The name describes the age of presentation. Energy is low, for example, hyperextension of the knee when landing from a jump. The child may limp or refuse to walk. Physical examination shows tenderness but little else: no swelling and no deformity. Röntgenogrammes show a faint oblique line or may be negative. Scintigramme shows increased uptake [A]. Alternatively, a presumptive diagnosis may be made based upon the typical presentation. Treat with a walking cast: apply the cast above the knee, flexed to 60 degrees, for an older child in less controllable circumstances, to automatically limit activity.
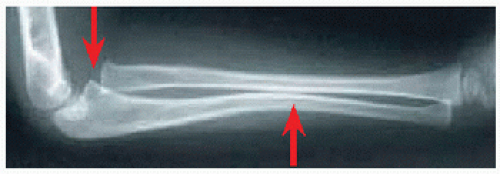
Diaphysial Fracture
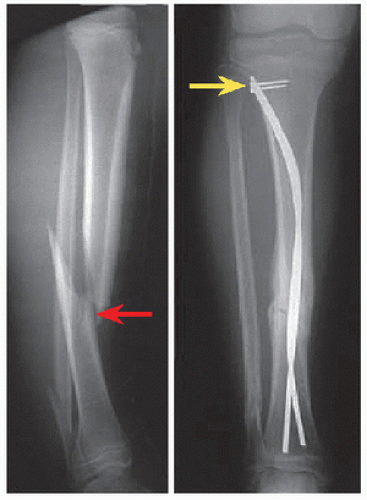
In the first decade, most tibial diaphysial fractures may be managed by reduction and above-knee cast. Flex the knee to at least 45 degrees to ease clearance of the floor with crutches. Include a valgus mold for an intact fibula, which pushes a broken tibia into varus. Follow with weekly röntgenogrammes until stable [B]. Modify ankle position to take advantage of tension produced through the posterior compartment muscles that may be harnessed to support a reduction in the sagittal plane, for example, extend the ankle and relax these muscles in an apex anterior fracture. Up to 10 degrees of residual valgus angulation and 5 degrees of varus are acceptable. Step-off is a concern at the subcutaneous border of the middiaphysis, though this will remodel in the first decade. Transverse plane deformity does not remodel significantly: be cognizant of transmalleolar axis relative to flexed knee during reduction and application of cast.
In the adolescent, surgical management reduces risk of malunion, lessens the burden of follow-up, and obviates the need for casting. Open diaphysial fractures also are treated operatively for wound care and healing and because, often, soft tissue interposition prevents acceptable reduction. Flexible medullary nails [C] are benign, load sharing, and stable enough to effect and maintain reduction and to stand alone for most fractures. Exceptions include significant comminution and bone loss, where external fixation is indicated.
Stress Fracture
Ten percent of all stress fractures affect immature children, while 30% occur in the mature adolescent. The tibia is most affected, comprising 45% of all stress fractures. Sports are the most common cause. Girls are affected more than boys, in part due to a hypoœstrogenic state induced by activity. Röntgenogrammes may be negative: confirm diagnosis with scintigramme. Manage by immobilization, protected weight bearing, or activity modification. Monitor healing by symptoms and until scintigramme normalizes.
Proximal Metaphysial Fracture
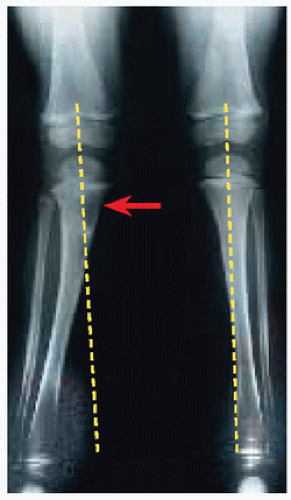
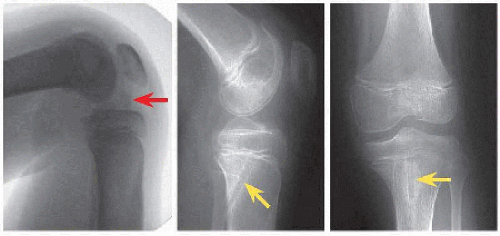
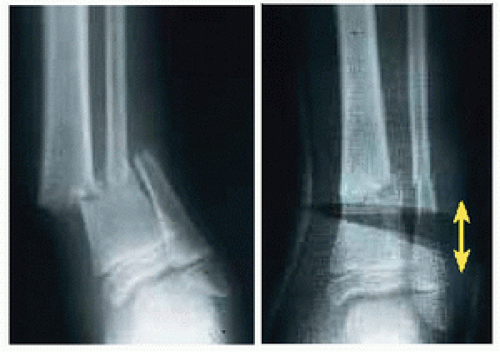
Greenstick fractures of the proximal metaphysis of tibia in the 3- to 7-year-old child (Cozen) may be followed by the development of valgus deformity [D]. Mechanism is valgus force. Medial overgrowth exacerbates normal development from varus to valgus in this age group. Röntgenogrammes show deviation of tibia away from mechanical axis and asymmetry of growth arrest line.
The natural history is spontaneous correction over a 2-year window. Educate family so that they may be patient during this period of observation. For persistent deformity, modulate growth by temporarily arresting the medial proximal physis with an implant that may be removed at correction.
Intercondylar Eminence Fracture
The intercondylar eminence also is referred to as the spine of the tibia. This fracture occurs around the turn from first to second decades. Mechanism is knee hyperextension and axial loading, as in sudden braking while riding a bicycle. The anterior cruciate ligament may stretch but does not fail, a fate that befalls the intercondylar eminence where the cruciates attach. While it is named after the nonarticular part of the knee, the fracture may extend to the articular surfaces of both condyles and may be associated with meniscal tear.
Evaluation The patient presents with knee pain that prevents weight bearing and effusion due to hæmarthrosis in fracture. Pain will not allow Lachman or pivot shift testing.
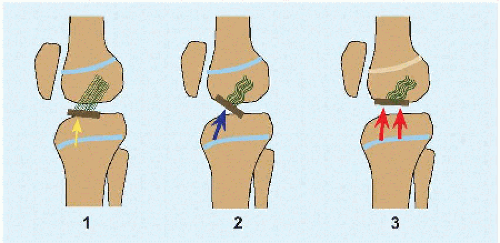
IMAGING The fracture may be classified on lateral view röntgenogramme [E]. CT allows accurate measurement of fragment displacement. Displacement >2 mm is unacceptable even though this is a nonarticular fracture, not because of concern for union or posttraumatic arthritis, but because this will introduce laxity in the anterior cruciate ligament that may destabilize the knee. MRI will show associated articular and ligamentous injury. Half of cases will show medial more than lateral meniscal or intermeniscal ligament entrapment, in type 3 more than type 2. Meniscal tear is rare (<5%).
Management In the emergency setting, aspirate the knee, inject a local anæsthetic, and apply a cast in full knee extension. In this position, the femoral condyles may compress any articular extension of the fracture to reduce the fragment. If there is meniscal entrapment, the reduction will be incomplete. If the fragment is solely nonarticular, it may be displaced by the extension manœeuver because the anterior cruciate ligament is taught. Confirm acceptable reduction with röntgenogrammes or CT.
Type I fractures are treated in an above-knee cast at 30 degrees flexion (relaxed anterior cruciate ligament).
Operative reduction and internal fixation is indicated for displaced fractures [F]. Articular structures may be explored and repaired by arthroscopy, by which the fracture also may be reduced and fixed. If MRI shows an isolated fracture, it may be treated via a linear incision parallel to the ligamentum patellæ starting at the apex of patella and continuing to the anterior articular margin. Because the anterior cruciate ligament is presumably stretched before the fracture occurs, débride the bed of the fracture in order to countersink the fragment and thereby tension the ligament. Fixation may be by suture passed through drill holes in the apophysis, for example, if fragment is small or comminuted, or a screw, which may be placed epiphysial or transphysial and which may be metallic or bioabsorbable. Postoperative immobilization and weight bearing are tailored to union of fracture, meniscal repair if performed, and associated collateral ligament injury if present. Plan removal of transphysial, to avoid growth disturbance, or metallic screws, which will overgrow.
Outcomes are obscure. Children may demonstrate persistent anterior cruciate ligamentous laxity on testing despite operative treatment yet have normal function, as determined by outcome instruments, for example, Lysholm knee score >90/100, and by return to preinjury level of activity. Educate patients and families that not uncommon after this injury are stiffness and prolonged knee pain, which will resolve with dedicated rehabilitation.
Proximal Physial Fracture
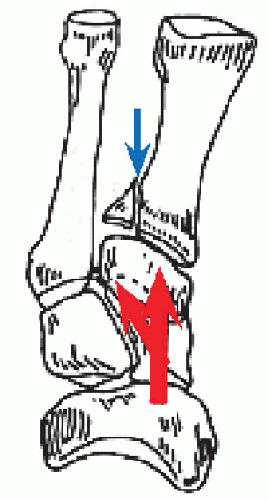
The greatest importance of these fractures is potential for popliteal artery injury by posterior displacement of the proximal metaphysis, as the proximal fragment is retained by the ligaments of the knee. Knee hyperextension drives the distal fragment into the vessel, which may be occluded or torn as it is tethered at the soleus fascia and interosseous membrane. The fractures are treated according to general principles of Salter-Harris types.







 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access