A Trauma is part of a child’s life This boy sustained a fracture of his forearm and ankle during play.
Children’s injuries not only differ from those of adults, they also vary depending on the age of the child. Infants, children, and adolescents experience different injuries. Appreciating these differences is essential to optimal management.
Statistics
Boys are injured more often than girls. Injuries increase in frequency with advancing age during childhood, and the percentage of fractures that occur through the physis increases with age as well [B].
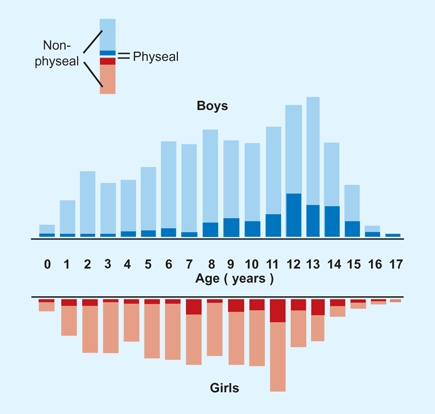
B Age distribution of physeal and nonphyseal injuries Note the differences between boys (blue) and girls (red). From Mizuta et al. (1987).
About half of boys and one-fourth of girls can expect to experience a fracture during childhood. Fractures are becoming more common as sports activities increase. The wrist is the most frequent site of injury [C]. Age affects the pattern of injury.
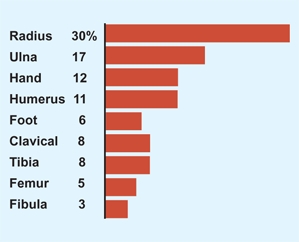
C Fracture frequency in infants and children Frequency of fractures in a sample of 923 children’s fractures. From Mizuta (1987).
Children Prone to Injury
Low bone mineral content
Children with generalized disorders such as osteogenesis imperfecta [A], renal diseases, cystic fibrosis, diabetes mellitus, and growth hormone deficiencies are at risk.

A Multiple fractures in osteogenesis imperfecta This newborn’s fragile bones resulted in paranatal fractures.
Neuromuscular disorders
Children with cerebral palsy, spina bifida, and arthrogryposis [B] are fracture prone because of the combination of poor mineralization and joint stiffness.

B Fractures due to joint stiffness in arthrogryposis These birth fractures resulted from trauma at delivery due to joint contractures.
Fracture personality
Children in general are at greater risk due to their higher activity levels, and some children in particular who have risk-prone behaviors are at even greater risk.
Physiology
The musculoskeletal system of children is different from that of adults, which explains why children’s fractures are different [C]. These differences gradually diminish with age, so that fractures in the adolescent are similar to those in the adult.
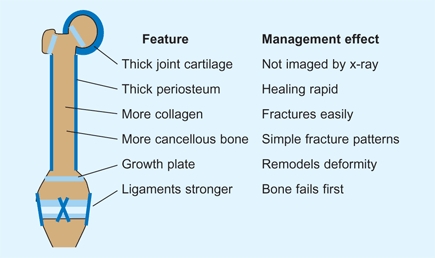
C Bone structural features affecting management The child’s musculoskeletal system is different from the adult’s in several important ways. These differences significantly affect management.
Growth Plate
The most obvious musculoskeletal difference is that the child has a growth plate [C]. The relative strength of the growth plate compared to adjacent bone changes with age. For example, the physis in infants is stronger than the adjacent bone, so diaphyseal fractures are most common.
Helps fracture management
The growth plate usually helps in managing fractures. Growth facilitates remodeling that corrects residual angulation. The potential for remodeling depends on the growth rate of the adjacent physis and on the remaining growth of the child.
Injured growth plate causes deformity
Just as the physis can resolve deformity, asymmetrical physical growth causes deformity.
Bone
Higher collagen-to-bone ratio
This lowers the modulus of elasticity and reduces the tensile strength of the bone [D].
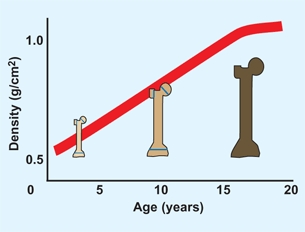
D Bone mineral density This graph shows bone mineral density in the femoral neck in normal subjects. From Thomas (1991).
Higher cellular and porous bone
This reduces tensile strength and reduces the tendency of fractures to propagate and explains why comminuted fractures are uncommon in children.
Bone fails in both tension and compression
This explains the mechanism of the common buckle fracture in children [E].
E Buckle fractures These fractures are common in children because the bone fails in both tension and compression and because of the high collagen content.
Bone transitions
between metaphysis and diaphysis cause a mechanical discontinuity, leading to certain fracture types.
Periosteum
Metabolically active
The periosteum is more metabolically active in the child than in the adult. This explains the exuberant callus seen in the infant [A and B] and the rapid union and increased potential for remodeling seen throughout childhood. Bone forms with the periosteal sleeve to create bone continuity. This active periosteum also contributes appositional bone, which facilitates remodeling.

A Exuberant callus formation in the newborn fracture This physeal separation resulted from birth trauma.

B Callus from femur fracture in an infant Note the extensive callus formation.
Thickness and strength
Children have increased thickness and strength of the periosteum. Fractures within the intact periosteal sleeve may have little displacement and be difficult to diagnose [C]. The intact periosteal hinge affects the fracture pattern [D] and may be helpful in reduction of fractures.

C Plastic bowing of the ulna This child has a dislocation of the radial head with plastic bowing of the ulna.

D Greenstick fracture of the forearm Greenstick fractures are common in the forearm, as bone bends before it fractures and the periosteal sleeve maintains apposition.
Age-Related Fracture Patterns
These changes in bone result in changing fracture patterns throughout growth [E]. The infant with the diaphyseal fracture, the child with a fracture through the metaphysis, and the adolescent with an epiphyseal injury are examples of this effect.
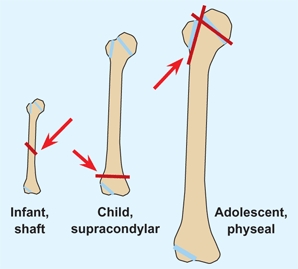
E Age-related injury types of the humerus This injury pattern is present in other long bones, with diaphyseal fractures in infants, metaphyseal fractures in children, and epiphyseal fractures in adolescents.
Ligaments
Ligaments are relatively stronger than bone. Usually bone fails before ligaments, which explains various injury patterns. Avulsion injuries are common in children [F and G]. The distal femoral physis fails before the collateral ligaments [H].

F Avulsion injury of the triceps Avulsion of the tendo-Achilles insertion is due to the greater tensile strength of the triceps tendon than calcaneal bone in the adolescent.

G Avulsion of the tibial spine The bone fails before the anterior cruciate ligament (ACL), resulting in a fracture of the tibial spine.

H Fracture of distal femoral epiphysis The physis fails before the adjacent bone or collateral ligaments. This is a common injury type in adolescents.
Cartilage
The increased ratio of cartilage to bone in children improves resilience but makes evaluation by radiography more difficult. The size of the articular fragment is often underestimated.
Physeal Injuries
Physeal injuries account for about one-fourth of all childhood fractures. They are most common in boys, in the upper limb, and in childhood [A]. Physeal injuries may also occur from infection, tumors, or ischemia. Physeal fractures are of great importance, as these injuries can affect subsequent growth and remodeling potential.
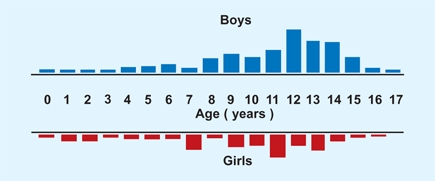
A Age distribution of physeal injuries in boys (blue) and girls (red) From Mizuta (1987).
Anatomy
The physeal anatomy is varied but the pattern is similar.
Physes
can be classified into three main categories:
Long bones
The femur is one of the long bones.
Ring epiphyses
occur in round bones (cuboid) and around secondary ossification centers.
Apophyses
occur at the site of muscle or tendon insertions (e.g., greater trochanteric apophysis).
Growth disturbances of long bone physes are most likely to be damaged and create the greatest deformity.
Long-bone physes
often show an undulating pattern with mamallary processes. This provides greater sheer strength but may lead to an increased risk of physeal damage from high-impact injuries. An example is the greater likelihood of growth arrest from simple physeal fractures of the distal femoral physis.
Injury
The physis usually fractures through the zone of provisional calcification, sparing the germinal cells so growth is unaffected. Less common injuries that damage the germinal zone or create a tethering bridge across the physis may slow or arrest growth.
Physeal susceptibility to arrest varies. The most sensitive long-bone physis is the anterior portion of the proximal tibial epiphysis. Recurvatum deformity may occur from trivial injury [B].

B Recurvatum deformity due to anterior tibial physeal arrest This physis is very vulnerable to arrest.
Stress injuries to the physis are most commonly observed in athletes and children with myelodysplasia [C]. The gymnast may develop a stress fracture of the distal radial physis. Such physeal injuries often cause growth arrest.

C Physeal injury in myelodysplasia Note the physeal widening.
Physeal arrest is most common in injuries that allow the bone to bridge the growth plate. The location and percentage of the cross-sectional area occupied by the bony bridge determines the extent of the secondary deformity.
Classification
Several classification systems for physeal injuries exist. The most simple and widely used is that originated by Salter and Harris (SH). Fractures are divided into five categories based on pattern [D, previous page]. SH-5 injuries are very rare. More comprehensive classifications include those devised by Peterson [E, previous page] and by Ogden. For complex injuries, use a more comprehensive classification.
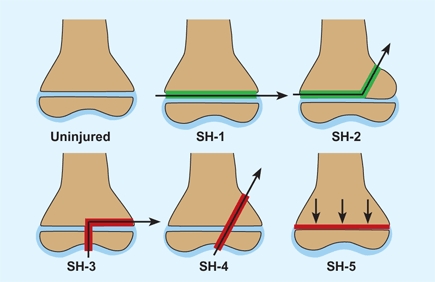
D Salter–Harris (SH) classification of growth plate injuries These are classified as types 1 through 5 based on the fracture pattern. Types 1 and 2 (green lines) do not traverse the epiphysis and usually do not cause growth problems. Types 3 to 5 (red lines) may cause growth arrest and progressive deformity.
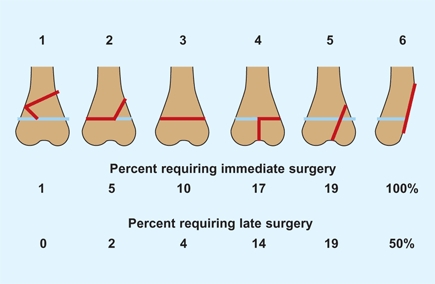
E Peterson classification The frequency of injuries of each type requiring immediate and late surgery are shown. From Peterson (1994).
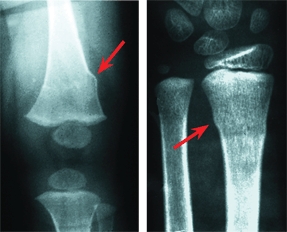
Classification of injury type is usually done by radiography. Imaging by CT scans may clarify complex fracture patterns such as those in triplane fractures of the ankle. MRI studies [A] often show considerably more physeal damage than was suspected from radiographs, and may change the SH category. Because experience is based on radiographic imaging, prognosis and management based on the more sensitive MRI may lead to overtreatment.
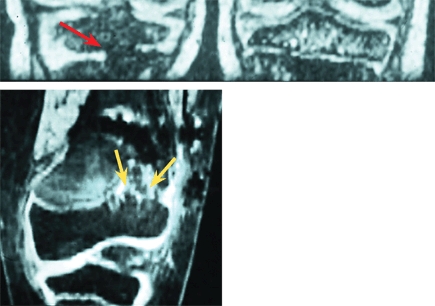
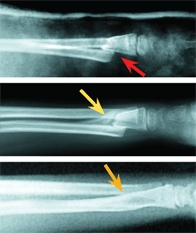
A MRI evaluation of physeal bars The bar may appear as a bridging bone (red arrow) or as an irregularity of the physis (yellow arrows).
Natural History
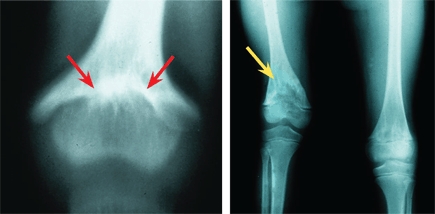
Most acute physeal injuries heal rapidly; any deformity remodels completely, and growth proceeds normally. About 1% of physeal injuries cause physeal bridging and altered growth [B]. Small bridges (<10%) may lyse spontaneously. Central bridges are more likely to lyse and less likely to cause deformity than peripheral ones. Central bridges may cause a fishtail deformity, which only slows rather than arrests growth [D].

B Natural history of physeal injuries of the distal radius This fracture occurred at age 10 years (red arrow). The reduction looks anatomic (orange arrow). The girl was not seen until age 20, when she complained of a wrist deformity. Note the effect of a volar bridge on the distal radius (yellow arrows).
D Central bridge resection in an infant This central bridge (red arrows) resulted from a birth fracture. The bridge was resected (yellow arrow), and growth resumed.
Physeal Bridge Management
Physeal bridge formation usually follows SH-3, SH-4, or SH-5 injuries. The mechanism is either a crush injury to the germinal layer or a displaced fracture that allows bone to form across the physis. The prognostic significance of the type is not always consistent. For example, physeal arrest also occurs in about half of SH-1 and SH-2 injuries of the distal femur in the older child or adolescent [C]. Physeal injury may also follow fracture of the diaphysis. The mechanism is unclear.

C Physeal bridge of distal femur This bar from a SH-2 fracture caused severe valgus deformity.
Avoid
physeal injury when placing fixation devices in children. Reaming of the upper femur for fixation of femoral shaft fractures is a common cause of physeal damage. Use alternative ways of fixation before the end of growth.
Prevention
of physeal bridge formation is best achieved by an anatomic reduction of SH-3 and SH-4 fractures. Open reduction and internal fixation that does not traverse the physis is best. If fixation is necessary across the growth plate, use small, smooth K wires.
Monitor growth
for detection of a physeal bridge. If a bridge is found, make a radiograph of the involved bone and the contralateral side on the same film every 4–6 months. Note changes in relative overall length or angulation of the adjacent joint surface.
Imaging physeal bars
may be done by CT scans or MRI studies. Order frontal and sagittal computer reconstruction of 1-mm CT scans. MRIs tend to show more soft tissue information but may be more difficult to interpret. Assess the location of the percentage of the cross-sectional area of the physis that the bridge occupies.
Birth and Neonatal Injuries
Birth Injuries
Birth injuries often occur in some unusual obstetrical situations such as large birth weight, shoulder dystocia, mechanically assisted delivery, or prolonged gestational age. It also occurs in infants with some underlying problem such as osteogenesis imperfecta or arthrogryposis.
The most common injuries include brachial plexus injuries and fractures of the clavicle. Other injuries include femoral shaft fractures [A] and neurologic injuries at the intracranial and spinal cord level.

A Birth fractures Joint injuries (yellow arrow) and diaphyseal fractures (red arrow) are examples of the spectrum of these injuries.
Manage these fractures by simple splinting. Manage clavicular fractures by simply strapping the arm to the thorax for comfort. Manage femoral shaft fractures in a Pavlik harness. Remodeling will correct any remaining deformity.
Fractures in Early Infancy
Neonatal fractures are most common in very low birth weight premature infants who have developmental nutritional rickets. Fractures most commonly involve the ribs, radius, humerus, and femur. Manage by metabolic therapy and splinting. Avoid casts.
Child Abuse
Because child abuse or nonaccidental trauma is a potentially lethal condition, consider this possibility in every infant or young child with a fracture. When the diagnosis of child abuse is missed, recurrent injuries occur in about half, and it is lethal in 10% of infants and children.
Evaluation
Be suspicious of any long-bone fractures in an otherwise normal infant in the first year. Many femoral shaft fractures in early infancy are due to abuse. Be concerned if the caregiver reports only a change in behavior without a history of injury or a trivial injury. Remember that abuse can occur at any socioeconomic level.
Examination
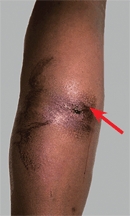
Look at the whole child. Other than the current problem, does the infant appear normal? Note any evidence of swelling, pseudoparalysis, or soft tissue trauma [B]. Bruising is more common than fractures.
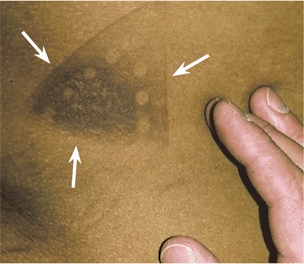
B Child abuse This hot iron burn scar is permanent and unmistakable (white arrows).
Imaging
If you are suspicious, order an AP radiograph of the chest, all four limbs, and a lateral of the skull. Order a bone scan to show recent fractures if further evaluation is indicated.
Fracture patterns in abuse
Fractures that have a high degree of specificity for abuse are metaphyseal fractures and fractures of the humeral shaft, ribs [C], scapula, outer end of the clavicle, and vertebra. Bilateral fractures, complex skull fractures, and those of different ages are suspect. Fractures of varying ages occur in only about 13% of cases. Try to date the fractures by radiographic appearance [C, and A, next page].
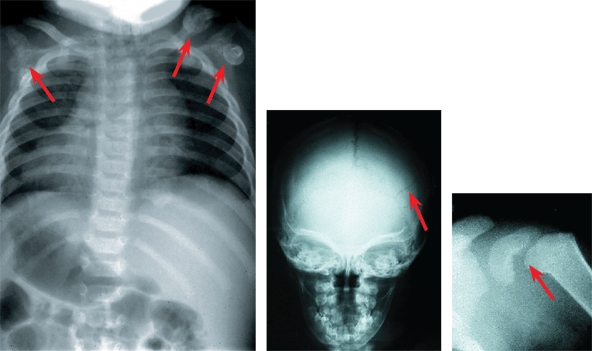
C Multiple fractures in abuse Multiple fractures (red arrows) at varying stages of development are common in abuse.
If abuse is a possibility
Personally call a social worker or case worker if abuse is suspected. Communicate the concern and index of suspicion. Consult pediatric colleagues for their opinions. Carefully document any findings and efforts. Parents of infants with accidental injuries usually accept consultations with a simple explanation of the reason. Objection should raise suspicion.
Remodeling
The capacity of bone to remodel significantly influences the management of fractures in children. One of the great challenges in pediatric orthopedics is to predict accurately which fractures require reduction and which will remodel sufficiently on their own.
Mechanism
Remodeling results from a combination of appositional bone deposition on the concavity of the deformity, resorption on the convexity, and asymmetrical physeal growth [A and B]. Remodeling requires a functional physis and intact periosteum.
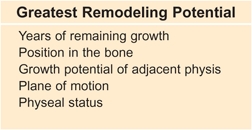
C Factors affecting remodeling potential These are the significant factors to consider in management.
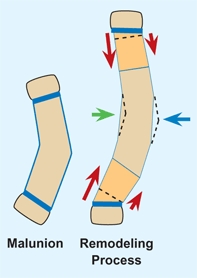
A Mechanism for remodeling Remodeling occurs from appositional periosteal formation (green arrow), resorption (blue arrow), and asymmetrical physeal growth (red arrows).
Redrawn from Gasco (1997).
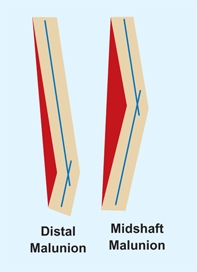
B Greater remodeling for mid shaft deformity For the same angular deformity, more correction (area in red) is required for midshaft than distal deformity.
Factors Affecting Remodeling Potential
Some generalizations are possible to predict whether a specific malunion will remodel without reduction [C].
Years of remaining growth
This is possibly the most important factor.
Position in the bone
The best examples are forearm fractures. Midshaft fracture remodeling is substantially less than fractures near the wrist [D].
D Remodeling of forearm The fracture fragments were in bayonet apposition (red arrow). Three months later, remodeling was in progress (yellow arrow). At 2 years (orange arrow), remodeling was nearly complete.
Growth potential of adjacent physis
As an example, fractures of the upper humerus show spectacular remodeling [F] as compared with distal humeral fractures.
Plane of motion
Remodeling is generally greatest for sagittal plane, then frontal, and least for transverse plane malunions.
Physeal status
Any damage to the adjacent physis reduces growth and the potential for remodeling.
Examples of Remodeling
Remodeling is one of the most forgiving features of childhood fracture management. Examples are useful to show the potential for correction to the clinician and for reassuring families. (See pages 294–295 to show families the potential for remodeling.)
Wrist
Note that the wrist has extensive remodeling potential [D].
Femoral shaft
Femoral shaft fractures in the child remodel completely [E].

E Remodeling of femoral shaft fracture This segmental fracture in an 8-year-old girl was managed in traction and in a cast (red arrow). Note the filling in of the periosteal sheath at 6 months (yellow arrow) and restoration of normal femoral shape at age 13 years (orange arrow).
Proximal humerus
Because the shoulder joint is multiaxial with rapid growth, remodeling is often spectacular [F].
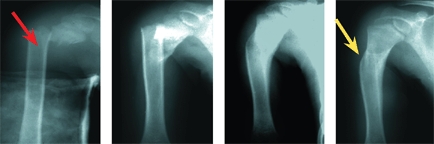
F Remodeling of the humerus This 8-year-old boy shows a complete loss of apposition (red arrow). Note the remodeling over the next 2 years (yellow arrow).
Pathologic Fractures
Pathologic fractures are relatively common in children. Fractures frequently occur through osteopenic bone in children with neuromuscular disorders and through bone weakened by tumors.
Evaluation
Be concerned if the trauma required for fracture is less than normal. Normal infants and young children’s bones can fracture with simple falls. Usually a history and screening examination will separate normal children from those with underlying osteopenic problems.
Management
Generalized disorders include those that decrease or increase bone density. Manage fractures through osteopenic bone in children with conditions such as cerebral palsy [A], spina bifida, and osteogenesis imperfecta with a minimum period of immobilization because mobilization increases deossification and increases the risk of additional fractures. Dysplasias increase bone density and may also be prone to fracture [B].
A Fracture in child with cerebral palsy The bone easily fractures, and abundant callus occurs during healing.

B Fracture in osteopetrosis These bones fracture easily and are difficult to fix internally.
Cast treatment
for conditions such as developmental hip dysplasia increase the risk of fracture. The period of greatest vulnerability is shortly after cast removal, as joints are stiff and bone is weakened by immobilization [C].

C Fracture following DDH treatment in a spica cast
Benign bone lesions
are often the sites of fracture.
Small localized tumors
If the lesion is small and the trauma significant, immobilize in a cast until union has occurred. Usually, it is best to allow the fracture to heal and then deal with the lesion. For larger lesions, especially those involving the upper femur, stabilization and bone grafting may be necessary.
Fibrous dysplasia
Consider early augmentation with a flexible intramedullary rod [D] to increase bone strength and reduce the risk of fracture. This treatment usually shortens the period of convalescence.

D Multiple fractures in fibrous dysplasia This child has developed a shepherd crook deformity from repeated fractures.
Unicameral bone cysts
Most cysts should be allowed to heal and then be managed as described in Chapter 7. Those of the upper femur require special consideration. Most require internal fixation to prevent malunion. Graft and fix during the same operative session. Avoid threaded or large fixation across any growth plate in the child under age 8–10 years. Smooth K wires may be applied across the proximal femoral physis. Bend the pins over to avoid migration.
Nonossifying fibromas
are common sites of fractures [E]. If they involve more than 50% of the transverse bone area, they may require grafting.

E Fracture through a nonossifying fibroma
Malignant tumors
Be most concerned about missing a fracture through a malignant tumor such as an osteogenic sarcoma [F]. Ask if the child or adolescent had night pain before the fracture. Night pain is often an indicator of a malignant tumor. Carefully review the radiograph with attention to the character of the bone. Early identification of the pathologic aspect of the fracture is the primary concern.

F Fracture through malignant osteogenic sarcoma This is the most worrisome fracture to miss.
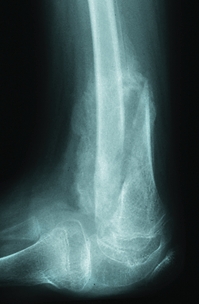
Open Fractures
Open fractures in children most commonly involve the tibia, but they may also complicate supracondylar fractures and fractures of the forearm, femur, and other bones.
Classification
The classification of open injuries is basically the same as for adults [A]. Overall, the prognosis for a given grade is better in children, especially infants and young children. Adolescents behave more like adults.
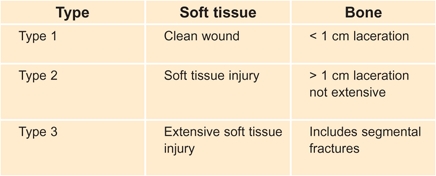
A Gustilo classification of open fractures in children
Management
Sequence
Manage acute injuries in the same sequence as done for adults. This involves antibiotic prophylaxis, tetanus update, debridement [B and C], and immobilization. Limb salvage is usually feasible. Open fractures in younger children can be managed less aggressively than those of the adolescent.


B Open supracondylar fracture This type 1 open fracture (arrows) produced only a puncture wound above the elbow. The wound was irrigated and edges debrided.

C Fracture debridement While swimming, this boy sustained an open tibial fracture from a boat propeller. This debridement was carefully performed to remove all devitalized and foreign material. An external fixator was placed, and the bone healed without infection.
Different management for the child
Managing the child differs from managing the adult in several ways: (1) soft tissue healing is much more rapid and complete, (2) devitalized bone that is not contaminated can be left in place and will incorporate, (3) the periosteum will generate new bone when bone is lost [D], (4) delayed union or nonunion is uncommon, and (5) external fixators may be left in place for prolonged periods to be certain bony union is solid.



D Open segmental fracture of the tibia This fracture (red arrows) was managed by debridement and removal of the loose contaminated segment. Note that the bone regenerated within the periosteum (yellow arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








