A Infection causes systemic illness This infant has septic arthritis of the elbow and is systemically ill.
The prevalence of osteomyelitis is declining and changing character. Long-bone infections caused by Staphylococcus aureus and septic arthritis caused by Haemophilus influenza have declined most. Osteomyelitis has changed forms, with more complex and unusual patterns [B]. The incidence of infection with resistant strains is increasing.

B Local spread Infection from metaphyseal osteomyelitis may spread into adjacent joints in the infant.
Infections are still important and often challenging, but improved management makes poor outcomes less common and less acceptable.
Pathogenesis
An understanding of the pathogenesis of musculoskeletal infections facilitates management.
Portals of Entry
Most infections are hematogenous, with the primary site of entry in the ear; oropharynx; or respiratory, gastrointestinal (GI), or genitourinary (GU) tracts [C] . Skin infections such as occur after chicken pox, penetrating injuries such as nails in the sole of the foot, or infections from surgical procedures are less common [D]. Extension of contiguous infections are least common, although adjacent joint infections are relatively common when associated with adjacent osteomyelitis [B].
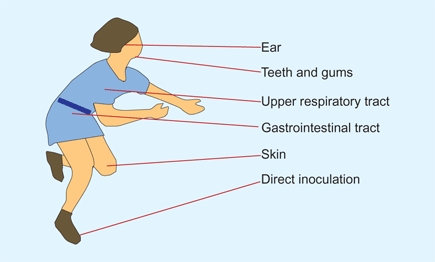
C Portals of bacterial entry
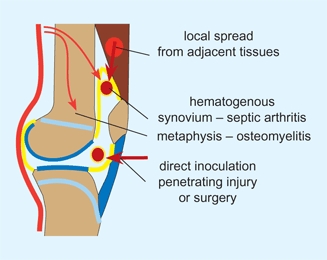
D Spread to bone and joints Infection is commonly hematogenous but may occur by local spread or from direct inoculation.
Initial Deposition
Bacteremia is a common event but rarely results in tissue infections. When infections occur, bone and joints are vulnerable. The reason for this vulnerability is unknown.
Bone
is usually infected in the metaphysis. Bacteria are deposited in capillary loops adjacent to the physeal plate. Nearly always, these bacteria are quickly destroyed by phagocytosis. Trauma is a factor that reduces resistance by causing the formation of a hematoma [A]. Bacterial proliferation is enhanced by the elaboration of a biofilm, which enhances bacterial adhesion to bone and provides protection from phagocytosis or antibiotics.
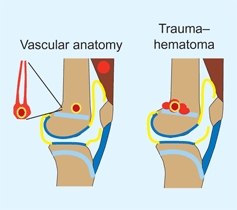
A Vascular anatomy of the metaphysis Bacteria may accumulate in vascular loops in the metaphysis. Traumas with hematoma formation provide good environments for bacterial proliferation.
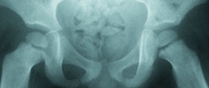
Joints
may be infected by hematogenous spread via the synovium, by a penetrating injury of a joint, by direct spread from a contiguous infection, or by bacterial transport by way of transphyseal vessels. Transphyseal vessels are present in early infancy before the formation of the growth plate [B]. This may account for the frequency of septic arthritis of the hip in the neonate [C]. In children, about a third of long-bone osteomyelitis is associated with septic arthritis of the adjacent joint.
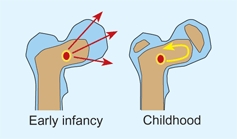
B Transphyseal spread Transepiphyseal vessels allow spread of infection from the metaphysis into the joint (red arrows). The presence of a physis blocks this spread (yellow arrow).
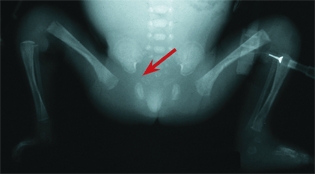
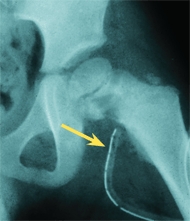
C Neonatal septic arthritis of the hip Note the widening of the joint space. This is a late finding.
Natural History of Infection
It is probable that the vast majority of bacterial colonies are destroyed by systemic and local mechanisms. The likelihood of progression is based on the balance between organism virulence and host resistance [D].
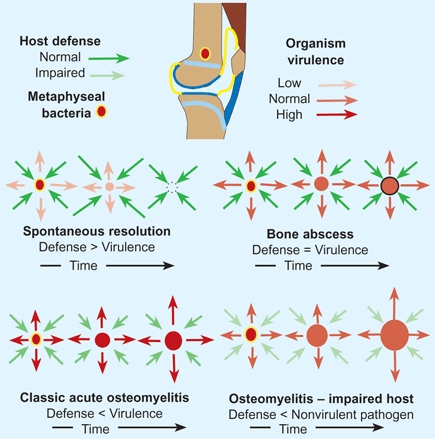
D Natural history of osteomyelitis This is often determined by host resistance and organism virulence.
Spontaneous resolution
is common. Host resistance exceeds the virulence of the organism.
Subacute osteomyelitis
is less common. Host resistance and virulence are about equal. A bone abscess forms reactive sclerotic bone walls off the abscess. No equivalent of this subacute form exists for septic arthritis.
Classic acute osteomyelitis, or septic arthritis,
results from a virulent organism and a normal host. The patient becomes systemically ill, and if untreated may develop septicemia and die, or extensive local bone necrosis may occur, and chronic osteomyelitis follows.
Impaired host
may allow development of a bone or joint infection from organisms of relatively low virulence, as seen in such conditions as sickle cell disease [E].
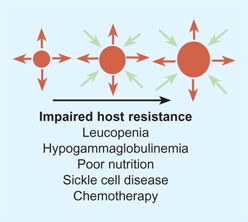

E Impaired host resistance. Organisms of low virulence may cause infections when host resistance is impaired.
Organisms
The organisms that infect the musculoskeletal system are numerous, varied, continually changing, and have predilection for the site, tissue, and age of the host [A].
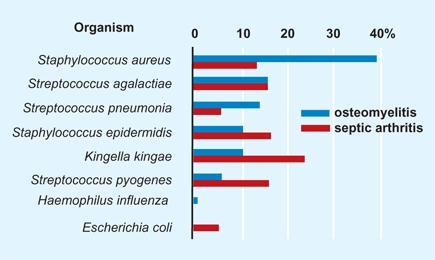
A Infecting organism in bone and joint infections in children under 36 months of age The percentage of 30 cases of osteomyelitis (blue bars) and 30 cases of septic arthritis (red bars) caused by different organisms. From data of Lundy and Kehl (1998).
Staphylococci
Gram-positive organisms are the most common causes of infections. The incidence is declining, however. Staphylococcus aureus includes a variety of pathogenic strains. New strains may be methicillin or vancomycin resistant. Staphylococcus epidermidis may cause infection in impaired hosts.
Streptococci
Streptococcal infections cause soft tissue and bony infections. Common pathogens are b-hemolytic streptococci. Streptococcus pneumonia may cause septic arthritis. Streptococcus agalactiae is a common cause of neonatal osteomyelitis. Streptococcus pyogenes is a less common pathogen.
Neisseria meningitidis
Meningococcal septicemia causes acute and chronic orthopedic problems. The disseminated intravascular coagulation and focal infections acutely cause necrotizing fasciitis and damage physeal circulation, causing physeal arrest and limb deformities [B].

B Septic physeal fusion This child with meningococcemia developed a fusion of the distal tibial growth plate (arrows).
Pseudomonas aeroginosa
This gram-negative rod is chondrophilic, and a common cause of joint infections of the foot from penetrating injuries.
Escherichia coli
This gram-negative rod is a rare cause of musculoskeletal infections.
Salmonella
This gram-negative rod is most likely to be encountered in sickle cell osteomyelitis.
Mycobacteria tuberculosis
This acid-fast organism has a resurgence of worrisome drug-resistant strains. It causes bone and joint infections in children. Tuberculous spondylitis with kyphosis is a common and serious deformity [C].


C Tuberculous spondylitis with kyphosis This was a common condition in the past (red arrow) in North America, and it is still prevalent in developing countries (yellow arrow).
Kingella kingae
This gram-negative coccobacillus is common in the respiratory system, slow growing, aerobic, and fastidious. It is difficult to culture. Only recently has it been found to cause musculoskeletal infections. It remains susceptible to most antibiotics.
Haemophilus influenza
This was previously a common cause of septic arthritis in infants. Now it is rare due to immunization programs.
Evaluation
The child’s medical history is important in the assessment of any previous injury or medical problem in the course of the current illness. The duration of symptoms in septic arthritis is of prognostic significance. Infections that are present for more than three days may cause residual joint damage, especially in the newborn. It is important to inquire about previous antibiotic treatment.
Physical Examination
Perform a screening examination first. Does the child appear ill [A]? The presence of systemic signs distinguishes septic arthritis from toxic synovitis. Is spontaneous movement present? The most reliable sign of septic arthritis of the hip in the newborn is a reduction of spontaneous movement of the limb. The reduction of movement from infection is described as pseudoparalysis. Swelling, erythema, and increased temperature are signs of inflammation, often due to infection. Note the position of the limb. Most infected limbs are positioned with the joints in slight flexion to reduce the intraarticular pressure. The hip is usually positioned in slight flexion, lateral rotation, and abduction [B].

A Ill Child This child is systemically ill from septic arthritis. Note the lethargy and dehydration.

B Cellulitis involving the hip This child has cellulitis about the left hip (arrow). The limb is held in a position of flexion and abduction that reduces soft tissue pressure and minimizes discomfort.
Note the extent of soft tissue swelling and joint effusions. Try to localize the area of tenderness about the knee, ankle, wrist, or elbow to determine whether the primary problem is in the joint or the adjacent metaphysis. This is helpful in differentiating septic arthritis from osteomyelitis.
Move the joint through a gentle range of motion to assess guarding or limitation of the arc of motion. Medial rotation is limited by inflammation about the hip.
Imaging
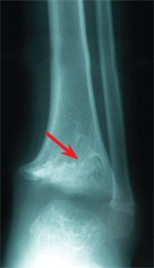
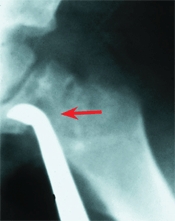
Conventional radiographs
may show soft tissue swelling [C] and obliteration of the soft tissue planes, but little else during the early course of an infection. A reduction of bone density of about 30% is necessary before radiographic changes are present. This usually requires 10–14 days [D].

C Soft tissue swelling Soft tissue swelling is present in this infant with septic arthritis of the elbow.


D Delay in radiographic appearance of osteomyelitis. This original film at the onset of the disease was normal (left). At 2 weeks (right), the lytic lesion is seen in the metaphysis (red arrow).
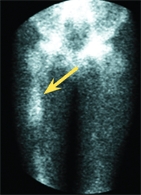
Bone scans
are useful in evaluating infection in the early stages of the illness. Technetium scans in septic arthritis are usually “warm.” Scans in osteomyelitis are usually warm or hot but may be cold early in the disease. In the early phase of the disease, uptake may be reduced and a cold segment of bone may indicate the presence of a severe infection. In early osteomyelitis, the phasic scan may be useful. The early phase includes vascular perfusion that parallels the physical findings of swelling and inflammation. In the second or osseous phase, uptake is greater over the site of involvement. Bone scans are not necessary if radiographic changes are already present. Often the bone scan is helpful in localizing the site of involvement [E]. Order a high-resolution scan for increased resolution. The bone scan is unaffected by bone or joint aspiration.


E Osteomyelitis of proximal femur Bone scans aid in localizing the site of infection. The metaphysis of the proximal femur on the right hip (arrow) shows more uptake than the opposite femur. The bone scan may be useful in determining the site for surgical drainage.
SPECT scans
Single-photon emission computed tomography (SPECT) scans are tomographic bone scans to identify focal inflammatory lesions of bone.
Ultrasound
evaluation for hip joint effusions [A] may be helpful if the ultrasonologist is experienced. A negative study should not delay a diagnostic aspiration if the clinical signs suggest the possibility of an infected joint. Ultrasound is also useful in localizing abscess formations around long bones, and its use is underutilized.

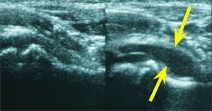
A Imaging in septic arthritis This child developed hip pain and guarding. The initial radiograph (top) was negative. The family refused aspiration. When seen the next day, the radiograph showed widening of the joint space (red arrow), and the ultrasound showed a joint effusion (yellow arrow).
MRI
studies of infection may be useful in localizing an abscess [B]. MRI studies of discitis may be alarming and can lead to overtreatment. Use newer imaging techniques only as adjuncts to conventional well-understood techniques.
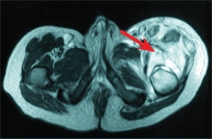
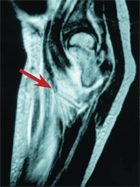
B MRI showing a thigh abscess This study shows the massive upper thigh abscess (arrows) secondary to femoral osteomyelitis.
CT
studies are sometimes useful in evaluating deep infections, such as those about the pelvis. CT and MRI studies may be helpful in localizing abscess and planning the surgical approach for drainage.
Laboratory Studies
The erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), and cultures are the most valuable laboratory tests. Serial measures are useful in following the course of infection. Often the white blood count (WBC) is normal.
ESR
is still valuable. Following the onset of infection, the ESR slowly rises to peak at 3–5 days and remains elevated for about 3 weeks if treatment is successful [C].
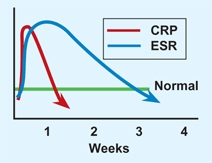
C CRP and ESR changes with time Following a musculoskeletal infection, the CRP declines more rapidly than the ESR. Based on Unkila-Kallio (1993).
CRP
peaks in 2 days and follows most closely the clinical course of the infection. If treatment is successful, the values return to normal in about a week.
Cultures
are essential and usually include blood, joint fluid, wound, and biopsy samples. Blood cultures are positive in 30–50% of patients. Be aware that negative cultures are common in both osteomyelitis and septic arthritis.
PCR
Molecular methods are being applied to the microbiology of bone and joint infections. Amplification techniques using polymerase chain reaction (PCR) have been shown to be very sensitive and specific when DNA probes are used for such specific infections as tuberculosis and Lyme disease. In settings of polymicrobial infections and infections where the likely organism is unknown, the ability of molecular techniques to identify the organism is as yet not superior to standard cultures. Further evolution of these techniques will likely increase their use in clinical medicine in the future.
Differentiation from Neoplasm
The differentiation of infection from neoplasm is sometimes difficult. Infections are more common, especially in younger subjects, and often show signs of inflammation. Subacute osteomyelitis may be confused with osteoid osteoma, osteosarcoma, chondroblastoma, Ewing sarcoma, fibrosarcoma, or eosinophilic granuloma. If necessary, establish the diagnosis with biopsy, curettage, and cultures. If the lesion is well demarcated, making a malignant tumor less likely, consider prescribing a course of oral antibiotics. If the lesion is due to an infection, the treatment is both diagnostic and therapeutic.
Eosinophilic granuloma
may show inflammatory features.
Ewing sarcoma
differentiation may pose a major problem. MRI and bone scans may be helpful [D]. Sometimes biopsy and cultures are necessary.


D Differentiating diaphyseal osteomyelitis from Ewing sarcoma In this child with osteomyelitis, note that the conventional radiograph was negative (left). This differentiation was aided by the MRI study, which showed little soft tissue involvement (arrow). The bone scan (yellow arrow) showed that only the femur was involved.
Management Principles
Management of infections in children is guided by a number of principles that often differ from those that apply to adults.
Greater Healing Potential
The potential for healing infection is remarkable in children. For example, discitis usually resolves with time with or without treatment. Bone damaged by osteomyelitis heals. Infection of bone may be contained and localized to only a residual abscess or it may resolve completely without treatment. Chronic osteomyelitis can nearly always be cured in children. Operative wound infections are uncommon in children.
Antibiotics
The selection of an antibiotic agent is complex. Consider the disease, organism, and special features of the child. These features include the age, concurrent illness, and the family situation. The route of administration and duration of treatment are other factors to consider. Initial therapy should be intravenous or, if access is difficult, intramuscular. Certain antibiotics are most commonly used for musculoskeletal infections [A and D].
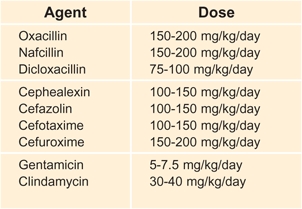
A Daily dosage of antibiotic treatment These are some broad generalizations for infants over 1 month of age and for children.
D Commonly used antibiotics for musculoskeletal infections
Oral antibiotic
therapy is justified if the infection is minor, the agent is well absorbed, and the family is reliable. In most serious infections, treatment may begin with parenteral antibiotics and switch to oral agents when the disease is under control. Before switching to the oral route of administration, be certain that adequate blood levels are documented following oral administration and that the family is reliable.
Methicillin-resistant organisms
Consider the incidence of methicillin-resistant Staphylococcus aureus (MRSA) in the community. If the child appears ill, the empiric choice is vancomycin, with modifications made after the culture and sensitivities are determined.
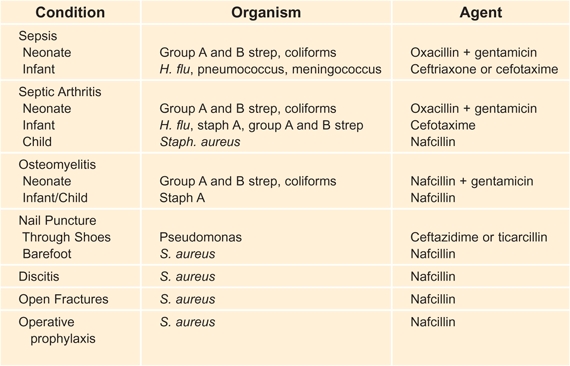
Duration of antibiotic treatment
is controversial. Several factors should be considered in determining the duration. Consider the severity and potential for disability that the infection poses, the rapidity of response to treatment [B], serial determinations of the ESR and CRP, the results of published studies, and the age of the child. Treat older children slightly longer. There are, however, some generalizations that can be made [C]. These can be modified according to the situation. Joint suppuration in septic arthritis reduces the effectiveness of the antibiotic treatment. For duration and dose of antibiotic selection, use the AAP Red Book [E].
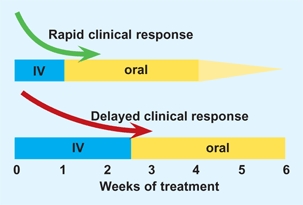
B Duration of IV antibiotic treatment Base duration of parenteral antibiotics on clinical response.
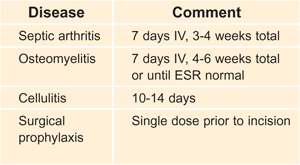
C Duration of antibiotic treatment These broad generalizations serve as an average duration of treatment.
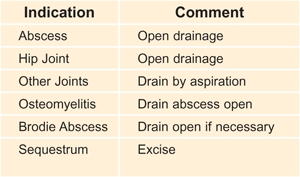
F Methods of drainage These are the common methods of drainage.
Operative Drainage
Drainage may be accomplished by needle aspiration, arthroscopic decompression, or open procedures [F, previous page].
Indications
Drainage is necessary whenever antibiotic penetration into the infected site is impaired. This penetration is most often due to the presence of an abscess or an accumulation of pus within a joint [A]. Impaired penetration may also be due to a loss of vascularity, as occurs in chronic osteomyelitis with sequestration or in soft tissue with poor vascularization due to thrombosis of vessels and acute inflammation. The presence of an abscess may be demonstrated by clinical examination, imaging such as ultrasound or MRI, needle aspiration, or suggested by a failure of clinical response to antibiotic treatment. This failure of response to antibiotics [B] is the failure of reduction in fever, pain, local inflammatory signs, and CRP during the first 48–72 hours after instituting antibiotic treatment. Keep in mind that this failed response may also be due to an ineffective antibiotic agent or to an immunocompromised child.
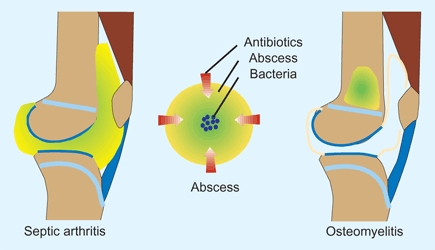
A Abscess protects bacteria from antibiotics The abscess prevents antibiotic penetration, protecting bacteria.
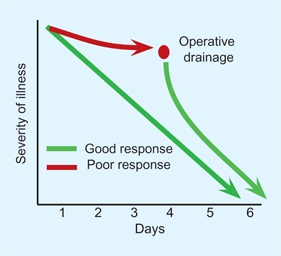
B Indication for operative drainage The failure of response to antibiotic treatment is often an indication for drainage.
Technique
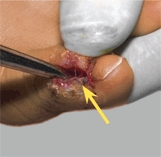
may be simply needle aspiration [C], as is feasible for most joints, arthroscopic, or open drainage. Open drainage of abscess due to acute infections requires simply draining the abscess through a small window in the cortex. If the abscess is near a growth plate, take care to avoid injuring the physis [D and F]. Monitor the position of the curette with fluoroscopy.

C Needle aspiration This drainage is usually adequate for most joints with septic arthritis.
D Drainage in difficult locations Monitor position of curette with fluoroscopy and avoid the physis (red arrow). Usually, a drain is placed (yellow arrow).
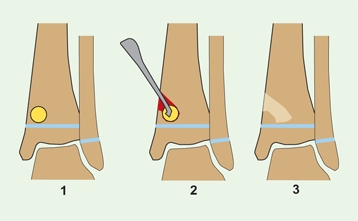
E Surgical drainage of acute or subacute osteomyelitis The infection is drained locally, with care taken to avoid injury to the growth plate. With time, bone fills in the defect.
The techniques for drainage of septic arthritis and osteomyelitis are presented on the next two pages.
Osteomyelitis
Osteomyelitis is an infection of the bone [A]. The infection may be acute, subacute, or chronic, and may involve any bone [B]. Osteomyelitis in the preantibiotic era often caused death or severe disability. Currently, osteomyelitis remains a relatively common problem but with a much better prognosis.
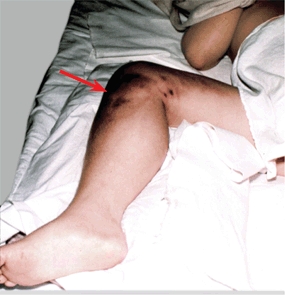
A Osteomyelitis This boy has osteomyelitis of the upper tibia with an associated soft tissue abscess (arrow).
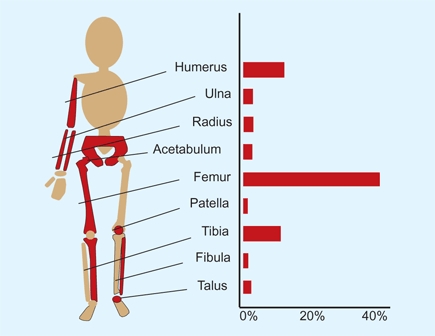
B Distribution of osteomyelitis From a series of 66 patients reported by Perlman (2000).
Natural History
The natural history of osteomyelitis depends upon the virulence of the organism, the resistance of the host, and the age of onset [C]. Virulent organisms may cause the death of a child due to overwhelming sepsis or, if localized, osteomyelitis progresses to chronic osteomyelitis. Chronic osteomyelitis develops through stages, which include bone and soft tissue abscesses causing sequestrum formation [D], intermittent drainage, and a lifelong disability. Chronic drainage may lead to development of squamous cell carcinoma of the sinus tracts during adult life.
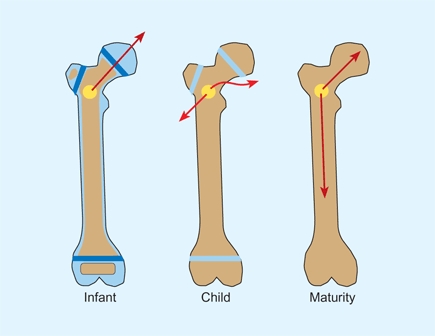
C Spread of osteomyelitis by age Bone structure affects the spread of osteomyelitis (red arrows). In the infant, the absence of an epiphyseal plate may allow spread into a joint. In the child, the path of least resistance is through the adjacent cortex to an extramedullary abscess. In the mature adolescent, the thick cortex and absence of growth plates allow extension throughout the medullary cavity.
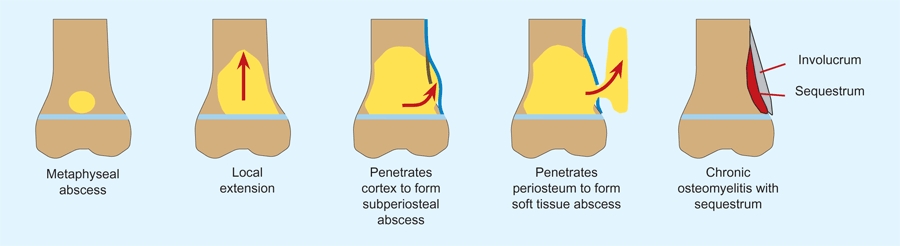
D Natural history of osteomyelitis The infection starts in the metaphysis. Contained by the growth plate, the infection spreads through the metaphysis, and then penetrates the cortex, creating a subperiosteal abscess. This may penetrate the periosteum to produce a soft tissue abscess. During healing, new bone (involucrum) forms around the devitalized cortical bone. This dead bone is called a “sequestrum.”
Acute Osteomyelitis
Acute osteomyelitis produces local pain, swelling, warmth, erythema, tenderness, and systemic manifestations of fever and malaise. Laboratory findings usually include a leukocytosis and elevated CRP and ESR. The CRP and ESR elevations are the most consistent laboratory findings.
Image
with conventional radiographs to provide a baseline, and assess for soft tissue swelling. A bone scan may be useful in localizing the site of involvement. Ultrasound and MRI studies may be helpful in localizing any abscess. To isolate the organism, culture the blood and consider aspirating the site of infection. Aspiration is most successful if a subperiosteal abscess is present.
Management
When planning management, estimate the stage of the disease [D, previous page]. Antibiotic treatment is usually successful without the need for drainage if the osteomyelitis is discovered early before suppuration has occurred. Start antibiotic treatment while awaiting the results of the cultures. Agent selection is done empirically, taking into consideration the age of the patient and the presence of any special features. Antibiotics are first given parenterally to ensure effective blood levels. The clinical course is monitored. If the antibiotic is effective against the organism and no suppuration is present, clinical improvement will occur with reduction in local signs of inflammation and systemic manifestations. If such improvement fails to occur over a period of 24–48 hours, the most likely cause is the formation of an abscess. An abscess requires operative drainage [A].
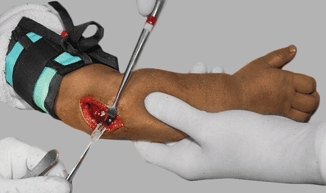
A Drainage of osteomyelitis Drain by windowing the cortex and exploring adjacent bone with a curette (yellow arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree