
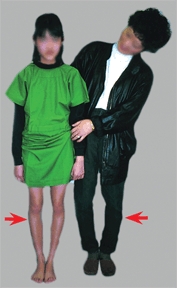
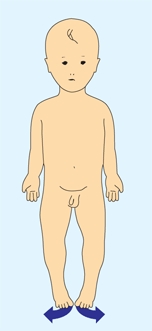
A Common developmental variations This girl (left) has femoral antetorsion and this boy (above) has physiologic genu valgum.
Lower Limb Development
Lower limb development shows a wide range of normal variability, both as variations of growth of children [A] and in the time of appearance of ossification [B and C]. The lower limb bud appears during the 4th embryonic week (see Chapter 1).
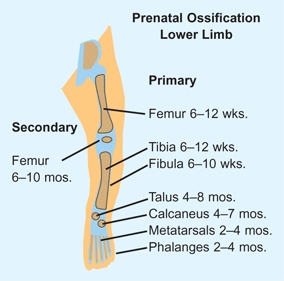
B Prenatal ossification Shown is the time schedule for the appearance of the primary and secondary ossification centers in the lower limb. Based on Caffey (1967).
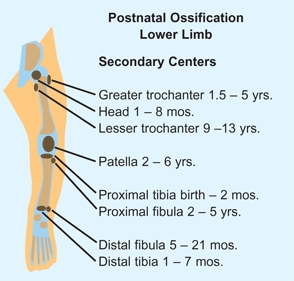
C Postnatal epiphyseal ossification The age range is shown for the appearance of epiphyseal ossification centers in the lower limb. In this range, ossification for girls occurs earlier than for boys. Based on Caffey (1967).
Ossification
Ossification appears first in primary centers [B] before birth. The secondary ossification centers appear in infancy and childhood [C].
Growth
Lower limb growth occurs earlier for girls than boys. In contrast with spine growth, the lower limbs show only a small secondary growth spurt [D]. Most growth of the foot occurs before the age of 10 years.
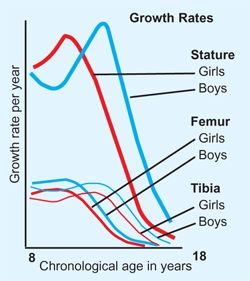
D Growth rates Shown are yearly growth rates for girls and boys for stature and femoral and tibial lengths. Based on Anderson (1963).
Limp
A limp is an abnormal gait that is commonly due to pain, weakness, or deformity. A limp is a significant finding and the cause should be established [A]. Be aware that a painless limp in a toddler maybe due to developmental hip dysplasia.
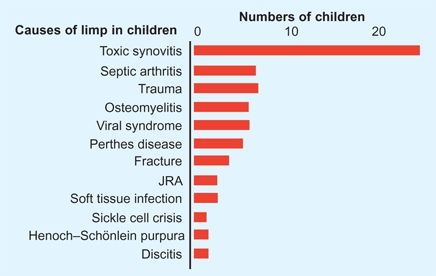
A Causes of limp in 60 young children Data from Choban and Killian (1990).
Evaluation
A presumptive diagnosis can usually be made by the history and physical examination. Age is an important factor to consider during evaluation.
History
First, inquire about the onset [B]. When was the limp first noted? Was the onset associated with an injury or illness? Was it gradual or abrupt? If the limp has been present since infancy, inquire about developmental history because children with neuromuscular disorders have delayed motor development.
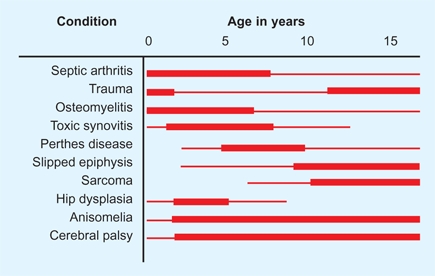
B Causes of limp by age The causes of limp are related to the age of the child. The fine red lines show the range and the heavy lines the most common age range of involvement.
Observation
The type of limp can usually be determined by observation. Remove outer clothing to allow the full view of the legs. Watch the child walk in the hallway of the clinic [C]. Observe in three phases: (1) Overview. Look for obvious abnormalities. Which side seems abnormal? Is the stance phase on each side equal in duration? Is lateral shoulder sway present? Is circumduction seen? (2) Study each leg individually. Look for more subtle changes. Is the normal heel-to-toe gait pattern present? Does the knee approach full extension during the stance phase? How is the hand carried? Elevation of the arm is seen in hemiplegia. (3) Make a presumptive diagnosis, and then make a final observation to be certain that this diagnosis is consistent with the characteristics of the limp.

C Hallway observation Evaluate the limp by studying the child’s gait while the child walks in the clinic hallway.
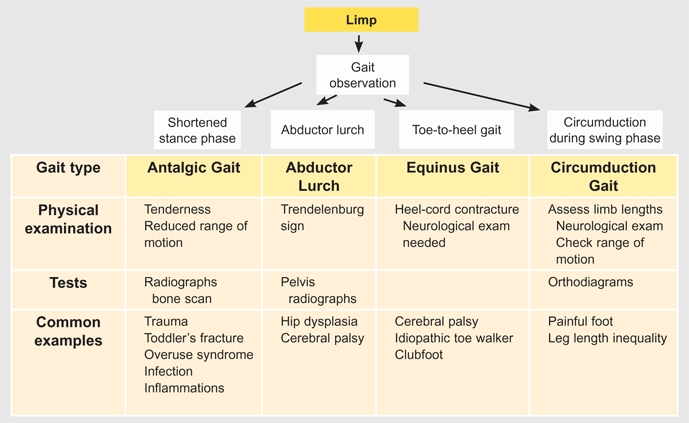
D Algorithm for evaluation of limping The major causes of limping are shown. A general categorization is first possible by observation. The exact causes are established by physical examination and laboratory studies.
Types of Limps
The common types of limping may be classified into four groups [D, previous page].
Antalgic gait
This is a painful limp. The most prominent feature is a shortened stance phase on the affected side. To minimize discomfort, the time of weight bearing on the affected side is shortened. The child is said to “favor” one side or the other. The term “favor” is ambiguous because it may be used to describe either the affected or unaffected side. Find the anatomic location of the problem by determining the site of tenderness, joint guarding, or limitation of motion. The hip is the most common site for the problem [A]. Follow-up with radiographs. Often a CBC and ESR or CRP are helpful. If the radiographs are negative, order a bone scan to localize the problem [B and C].
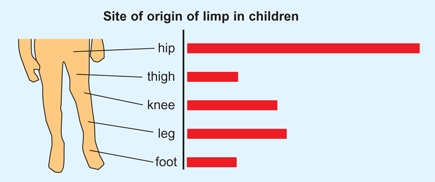
A Origin of limp in 60 young children Data from Choban and Killian (1990).

B Role of bone scan in limp evaluation This child had an antalgic limp with a negative physical examination, radiographs, and ESR. The bone scan showed increased uptake over the calcaneus (red arrow). This suggested a stress injury to the calcaneus. This was confirmed by a radiograph 2 weeks later, showing evidence of a stress fracture (yellow arrow). The child had been stressed by being taken on long walks in a shopping mall.

C Obscure limp from osteomyelitis This 2-year-old complained of night pain and showed a subtle limp during the day. Radiographs were negative, and the bone scan showed slight increased uptake in the upper femur (orange arrow). CT scan demonstrated an intracortical defect (red arrow). The differentiation from osteoid osteomy was made by a resolution with antibiotic treatment.
Abductor lurch
results from weakness of the abductor muscles, usually due to hip dysplasia or a neuromuscular disorder. An abductor lurch is characterized by lateral shoulder sway toward the affected side or sides. In normal gait, the abductor muscles contract during the stance phase to maintain a level pelvis and a linear progression of the center of gravity of the body. If the abductors are weak, the pelvis tilts and falls on the unsupported side during stance. To maintain the center of gravity over the foot, the shoulder shifts toward the weak side. This shift is referred to as an abductor lurch or a Trendelenburg gait. Weakness of the abductors is demonstrated by the Trendelenburg test or sign. The test is positive if the pelvis drops on the unsupported side during single-leg standing. The cause of the abductor lurch is usually established by a standing radiograph of the pelvis and a neurological examination.
Equinus gait
An equinus gait is due to a heel-cord contracture, which is usually due to cerebral palsy, residual clubfoot deformity, or idiopathic heel-cord tightness. Regardless of the etiology, the contracture causes a “toe-to-heel” sequence during the stance phase on the affected side. In the young child, equinus is often associated with a “back knee” or recurvatum deformity of the knee that occurs during the stance phase. Document the deformity by evaluating the range of dorsiflexion of the ankle with the knee extended. The ankle should dorsiflex more than 10°. If an equinus deformity is present, a thorough neurological examination is required. Be aware that this may be confused with a short leg gait due to developmental hip dysplasia.
Circumduction gait
allows a functionally longer limb to progress forward during the swing phase. Circumduction is often due to a painful condition about the foot or ankle because circumduction requires less ankle movement, making walking more comfortable.
Management
The limp may be caused by something as simple as a stone in the shoe, or by something as serious as leukemia or osteogenic sarcoma. Thus, generalizations regarding management cannot be made. Sometimes the cause of the limp cannot be determined. Should the diagnosis be unclear, reevaluate the child weekly until the problem resolves or a diagnosis is established.
Leg Aches
Leg aches, or growing pains, are idiopathic, benign discomfort of extremities, which occur in 15–30% of children. The pains are most common in girls, usually occur at night, and primarily affect the lower limbs. The condition produces no functional disability or objective signs and resolves spontaneously without residua. The cause is unknown. Undocumented speculation on cause includes genetic, functional, or structural (hypermobility) etiology. Leg aches follow headaches and stomachaches as the most common sites of pain during childhood.
Clinical Features
The differential diagnosis of leg aches includes most of the painful conditions involving the musculoskeletal system in children. The diagnosis is made by exclusion [A].
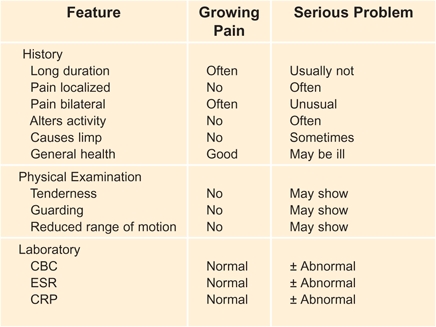
A Differentiating growing pains from more serious problems The features of growing pains are usually so characteristic that special studies are seldom required.
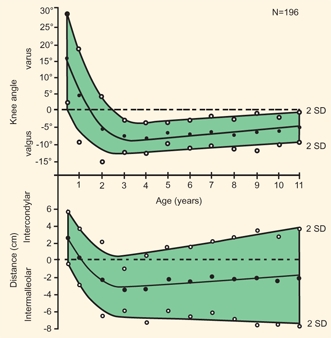
B Normal values for knee angle The normal values for the knee angle are shown in knee angle and intermalleolar or intercondylar distances. From Heath and Staheli (1993).

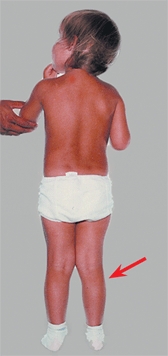
C Physiologic bowlegs This 18-month-old infant has moderate bowing.
D Physiologic knock-knees This 3-year-old girl has mild physiologic knock-knees.
History
The pain from leg aches is typically vague, poorly localized, bilateral, nocturnal, and seldom alters activity. This condition does not affect gait or general health. A history of long duration is most consistent with the diagnosis of leg aches. This long duration is helpful in separating out more serious problems, which over a period of time will usually produce objective findings.
Screening examination
Does the child appear systemically ill? Is deformity or stiffness present? Does the child limp?
Tenderness
Systematically palpate the limbs and trunk for tenderness.
Joint motion
Is joint motion guarded or restricted? Check for symmetry of medial rotation of hips.
Differential Diagnosis
Night pain may also be due to a tumor, such as osteoid osteoma, osteogenic, or Ewing sarcomas. Tumor pain is more localized, often associated with a soft tissue mass, progressive, and usually occurs later in childhood than growing pains.
Management
If the history is atypical for leg aches, or signs are found on examination, imaging and laboratory studies are required. If the findings are negative, a presumptive diagnosis of growing pains or leg aches is made. Provide symptomatic treatment with heat and an analgesic. Reassure the family about the benign, self-limited course of the condition, but advise them that if the clinical features change, the child should be reevaluated.
Genu Varus and Genu Valgus
Genu varum and genu valgum are frontal plane deformities of the knee angle that fall outside the normal range, ±2 SD of the mean. Knee angle variations that fall within the normal range are referred to as bowlegs or knock-knees or physiologic variations [A]. The range of normal for knee angle changes with age [B, previous page]. Lateral bowing of the tibia is common during the first year, bowlegs are common during the second year [C, previous page], and knock-knees are most prominent between ages 3 and 4 years [D, previous page]. Varus or valgus deformities are classified as either “focal,” as seen in tibia vara, or “generalized,” as occurs in rickets.

A Physiological bowlegs and knock-knees These siblings show the sequence, with the toddler having bowlegs and the older sister having mild knock-knees.
Evaluation
History
Inquire about the onset. Was there an injury or illness? Is the deformity progressing? Are old photographs or radiographs available for review? Is the child’s general health good? Does the family provide a normal diet? Are other family members affected?
Physical examination
Start with a screening evaluation. Does the child have normal height and body proportions? Short stature is common in rickets and various syndromes. Are other deformities present? Is the deformity symmetrical [B]? Is the deformity localized or generalized? Are the limb lengths equal? Shortening and knee angle deformity may be due to epiphyseal injuries or some developmental problems such as fibular hemimelia. Measure the rotational profile. Frontal and transverse plane deformities often coexist; make a clear separation. Measure the deformity. With the patella directly forward, measure the knee angle with a goniometer. Measure the intermalleolar or intercondylar distance. Does the deformity increase when the child stands? If the collateral ligaments are lax, such as in achondroplasia, the varus deformity is worse in the upright position.


B Pathological genu valgum Deformity is asymmetrical and due to osteochondromatosis (yellow arrows).
Laboratory
If the child has a generalized deformity, order a metabolic screen, including calcium, phosphorus, alkaline phosphatase, and creatinine, plus a hematocrit.
Imaging
If findings suggest the possibility of a pathological basis for the deformity, order a single AP radiograph of the lower limbs [C]. If knee ligaments are loose, make the radiograph with the infant or child standing. Position the child with the patella directly forward [C]. Use a film large enough to include the full length of femora and tibiae. A 36-inch film is often required. Study the radiograph for evidence of rickets, tibia vara, or other problems. Measure the metaphyseal-diaphyseal angle of the upper tibia (see D, pg. 142). Values above 11° are consistent with but not diagnostic of tibia vara. Measure the hip-knee-ankle angle. Complete the evaluation with other imaging studies if necessary. For knee deformities, a lateral radiograph is useful. CT or MRI studies may be useful in identifying and measuring a physeal bridge. Document the deformity by photography. A sequence of photographs provides a graphic record of the change with time.

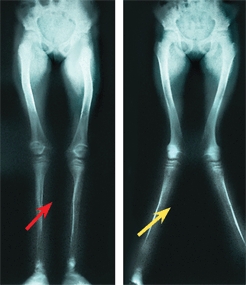
C Positioning for radiographs This girl is being carefully positioned to assure an accurate study. Positioning the patient to fit the legs on the radiograph (red arrow) results in misinformation. In the same patient, note the difference with a properly positioned study (yellow arrow).
Diagnosis
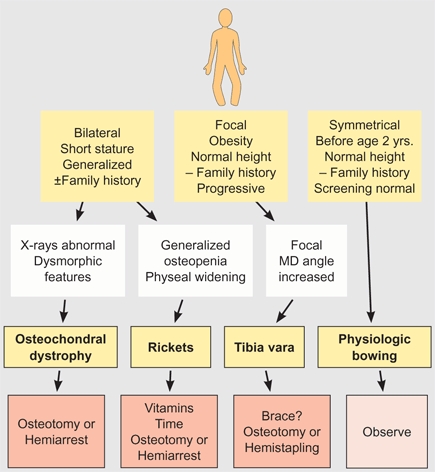
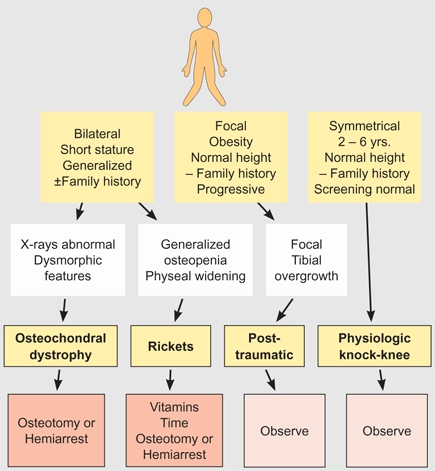
Follow a plan [D and E]. First make the differentiation between physiologic and pathologic forms [A and B]. If a pathologic form is present, consider the different categories of causes [C]. Causes are varied, and usually the diagnosis is not difficult.
A Familial genu varum Asians tend to have more physiological bowing than other groups.
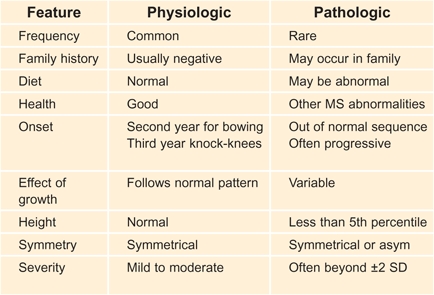
B Differentiating physiologic and pathologic genu varum
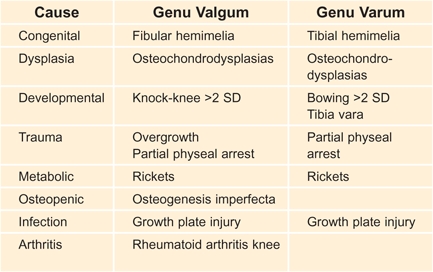
C Classification of pathologic knee angle Causes of genu varum and genu valgum are listed.
D Evaluation of genu varum or bowlegs This flowchart shows the differentiation of the common causes of change in knee angle.
E Evaluation of genu valgum or knock-knees This flowchart shows the differentiation of the common causes of change in knee angle.
Evaluation
Mechanical axis
Obtain a long, standing radiograph of the lower limbs. Be certain the child is positioned with the patella directly anterior when the exposure is made. Draw the axis of the femur and tibia connecting the center of the femoral head to the center of the distal femoral epiphysis [A, next page]. Construct a second line between the midpoint of the upper and lower tibial epiphyses. Mark the articular surfaces. Measure the degree of valgus or varus.
Zone system
On a full-length radiograph, draw a line between the femoral head and ankle. Note the position of the knee relative to this axis [B, next page].
Management Principles
The vast majority of children have bowlegs or knock-knees that will resolve spontaneously. If the intracondylar and intramalleolar distances are >8 cm, consider a consultation.
Document these physiological variations with a photograph and see the child again in 3–6 months for follow-up. No radiographs are necessary. If the problem is pathological, establish the cause. Then consider treatment options.
Nonoperative treatment
with shoe wedges is not effective and should be avoided. Long-leg bracing may be used for early tibia vara, but its effectiveness is uncertain. Avoid long-term bracing for conditions such as vitamin D–resistant rickets because the effectiveness of bracing is unclear and considerable disability results from brace treatment.
Operative correction
options include osteotomy, or hemiarrest procedures either by hemiepiphysiodesis or unilateral physeal stapling. The objectives of operative treatment are to (1) correct knee angle, (2) place the articular surfaces of the knee and ankle in a horizontal position, (3) maintain limb length equality, and (4) correct any coexisting deformities. To achieve these objectives, preoperative planning is required.
Make corrective osteotomies
as close to the site of deformity as practical.
Translation of the osteotomy
may be necessary to position the joint within the mechanical axis.
Multilevel osteotomies
are often necessary in generalized deformities from metabolic conditions and osteochondrodystrophies. Balance the number of osteotomies with risks.
Recurrent deformity
is likely in certain conditions, so delay each correction as long as possible to reduce the number of procedures required during childhood.
Idiopathic Genu Valgum and Varum
Valgus deformity with an intermalleolar distance exceeding 8–10 cm is most common in obese girls. This deformity seldom causes functional disability; the problem is primarily cosmetic. If severe, with an intermalleolar distance of >15 cm, consider operative correction by hemiepiphysiodesis or stapling. Make a standing radiograph and construct the mechanical axis. Determine the site(s) of deformity. In most cases, the distal femur is most deformed near the appropriate site for correction.
Varus deformity is most common in Asians [A, previous page]. The varus deformity may be familial. Whether it increases the risk of degenerative arthritis of the knee is uncertain. This deformity seldom requires operative correction. Manage severe deformity by stapling or hemiepiphysiodesis.
Posttraumatic Genu Valgum
Posttraumatic genu valgum results from overgrowth following fracture of the proximal tibial metaphysis in early childhood [C]. Valgus may also be due to malunion or soft tissue interposition in the fracture.
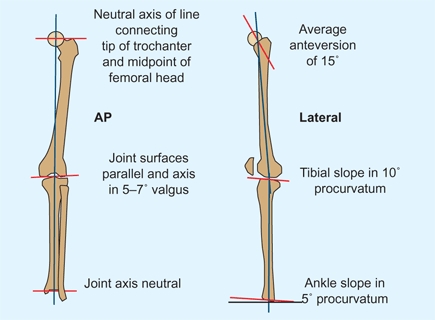
A Normal mechanical axis of lower limbs These are average values. Based on Paley and Tetsworth (1992).
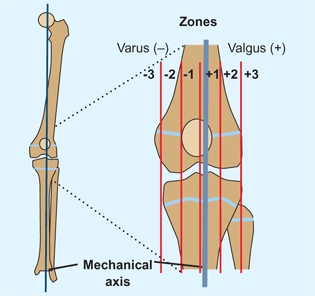
B Zone system for assessing mechanical axis The zone into which the mechanical axis falls is graded as a (-) for varus and a (+) for valgus, and into thirds with values ranging from 1 to 3. Based on Stevens et al (1999).

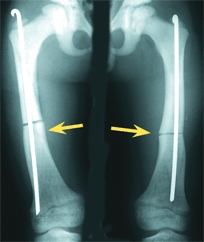
C Posttraumatic genu valgum This deformity is due to overgrowth of the tibia following proximal tibial metaphyseal fracture.
Natural history
The deformity develops during the first 12 to 18 months due to tibial overgrowth following the fracture. This is followed by a very gradual reduction of the valgus over a period of years. In the majority, this correction is adequate and no operative procedure is necessary.
Management
Manage proximal tibial fractures by correcting any malalignment, and immobilize with a long-leg cast applied with gentle varus molding. Document reduction and position with a long film that includes the entire tibia. Advise the family of the potential of this fracture to cause a secondary deformity, which cannot be prevented. Avoid early osteotomy because recurrence is frequent and the deformity usually resolves spontaneously with time. Reassure the family that the knee will not be damaged by the deformity. Should the deformity persist, correct by osteotomy or by hemiepiphysiodesis or stapling near the end of growth.
Rickets
Suspect rickets in a child with increasing genu valgum, short stature, and a history of an atypical diet or similar deformities in other family members. Rickets produces a generalized genu valgum with bowing of the diaphysis and rarefaction of the epiphysis. Low calcium and phosphorus and a high alkaline phosphatase are confirming laboratory findings. Document severity with a 36-inch radiograph of the entire femur and tibia. Measure the hip-knee-ankle angle and mechanical axis zone.
Manage by first referring the child to an endocrinologist to optimize the medical management of the rickets. Despite optimal medical management, the deformities often persist in vitamin D–resistant forms of rickets.
Bracing
The role of bracing is controversial, as long-term bracing imposes a major added burden on the child and the value of bracing has not been shown.
Surgery
If possible, delay correction until late childhood for stapling or adolescence for osteotomy. Correction at the end of growth reduces the risk of recurrence. If deformity is severe, correction may be necessary in childhood [A]. Plan osteotomy as discussed earlier with long films and cutouts. Drape the entire limb free to visualize adequacy of correction. Correct at one or more levels on each bony segment following the preoperative plan. Immobilize for about 10 weeks, as healing may be slightly slower than normal.

A Operative correction of rachitic deformity Multilevel correction is often necessary (red arrows). In some, intramedullary fixation can be used (yellow arrows).
If operative correction is performed before the end of growth, recurrence is common. Recurrence is most rapid in the younger child.
Tibia Vara
Tibia vara, or Blount disease, is a growth disorder involving the medial portion of the proximal tibial growth plate that produces a localized varus deformity [B]. The incidence is greater if the child is black, obese, has an affected family, and resides in certain geographical locations such as the southeastern part of United States. The cause is unknown but it has been theorized that in susceptible individuals mechanical stress damages the proximal medial growth plate, thus converting physiologic bowlegs into tibia vara.



B Tibia vara These images are of a 6-year-old boy with moderate deformity. Note the deformity and medial subluxation of the femur on the tibia as it appears in standing and walking.
Evaluation
Two clinical patterns of tibia vara are seen. Radiographs in early infantile tibia vara may be difficult to differentiate from physiologic bowing.
The metaphyseal–diaphyseal angle
is often used. This angle [D] shows considerable overlap between physiologic and tibia vara cases. If the angle exceeds 15°, tibia vara is likely. Differentiation is made by following radiographs made every 3–6 months. Physiologic varus usually improves after the child’s second birthday. Tibia vara progresses and shows diagnostic metaphyseal changes.
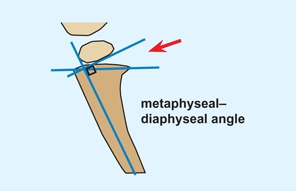
D The metaphyseal–diaphyseal angle This angle (red arrow) is commonly measured.
Bone scan
is seldom necessary but will show increased uptake on the medial side of the proximal tibial physis [C].
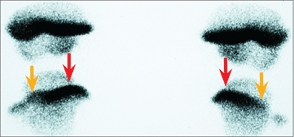
C Bone scan Bone scans early show increased uptake on the medial aspect of the proximal tibial epiphysis (red arrows) as compared with the lateral side (orange arrows). This may be helpful in differentiating early tibia from physiologic bowing.
MRI studies
show considerable deformation, which might be helpful for complex deformity management.
Langenskiöld stages
These are stages of the disease [E] with transition from one to the next over time.
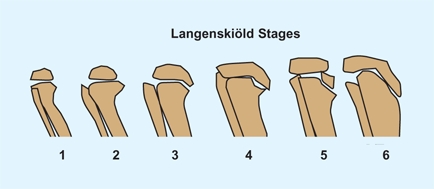
E Langenskiöld classification This classification is commonly used but sometimes difficult to apply.
Management
Treatment is based on the stage of tibia vara [E, previous page] and the age of the child.
Bracing
Mild deformities may resolve without treatment, so the beneficial effect of the brace is uncertain. Often braces are used to treat stage 1 and 2 disease. If treatment is elected, order a long-leg brace with a fixed-knee that incorporates valgus loading. The brace should be worn during active play and at nighttime.
Operative Correction
Operative correction may be achieved by an osteotomy or by initiating asymmetrical growth to correct the deformity. This asymmetrical growth may be achieved by a permanent hemiepiphysiodesis or by a reversible stapling procedure.
Osteotomy in the child
If tibia vara progresses or is first seen in stages 3 and 4, osteotomy is indicated. Perform the osteotomy before age 4 years if possible [A]. Deformities of stages 5 and 6 are more complex and may require a double-level osteotomy to correct both the genu varum and the articular incongruity. Also assess the shape of the distal femur as varus or valgus deformity may contribute to the deformity. Medial tibial torsion is also a common associated deformity. Correct the varus and torsion by a simple closing wedge with rotation or by an oblique osteotomy. Correct the thigh-foot angle to about +10 degrees and overcorrect the varus to about 10 degrees of valgus. Use a sterile tourniquet so the entire limb can be seen to ensure appropriate correction. Release the anterior compartment fascia to reduce the risk of a compartment syndrome. Fix the osteotomy with crossed pins and supplement the fixation with a long-leg cast.



A Infantile tibia vara This disease is usually bilateral and may cause deformity that requires correction by osteotomy (red arrow).
Hemistapling
may be an alternative to osteotomy for stage 2 or 3 deformities.
Physeal bridge resection
Rarely, a physeal bridge is suspected in unilateral involvement in mid to late childhood. CT or MRI studies confirm the presence of the bridge. Resect the bridge, fill the defect with fat, and correct the tibial deformity by osteotomy.
Surgery in the adolescent
Operative correction in the older child or adolescent is usually complicated by obesity. Stabilize the osteotomy with an external fixator. External fixation provides adequate immobilization without need for a cast and allows the option to adjust alignment during the postoperative period [B].



B Adolescent tibia vara This form is often unilateral (red arrows) and usually requires operative correction. External fixation is often an excellent choice in operative correction (yellow arrow).
Stapling
Stapling is a convenient method for correction. The disadvantages are the larger scar, the risk of staple extrusion, and a second operation for staple removal. The advantage is simplicity. The staples (usually two) are placed, the patient carefully followed, and when the deformity is corrected the staples are removed. If the staples are placed extraperiosteal, growth can be expected to resume. The zone system is commonly used to determine the need for correction. A zone 3 deformity may be an indication for stapling. A rebound often occurs after staple removal, undoing some correction, so overcorrect slightly in anticipation of this common problem, especially in children younger than 12 years of age.
Hemiepiphysiodesis
With accurate timing, hemiepiphysiodesis has several advantages. The scar is short and the procedure simple and definitive. Bowen has developed a table to aid in timing [C]. Careful follow-up is essential because if the deformity appears to be destined for overcorrection, arresting the entire epiphysis becomes necessary.
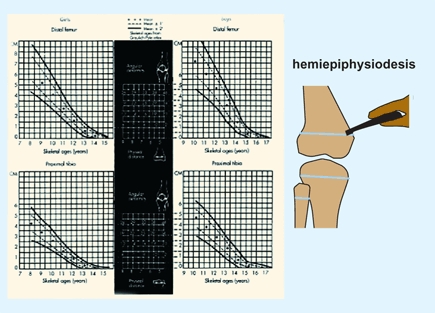
C Chart for timing hemiepiphysiodesis This chart was created to time correction of angulatory deformities. From Bowen (1985).
Timing
The timing of the stapling is not critical. When correction is achieved, the staples are removed. Timing of epiphysiodesis is critical, and tables have been developed to help estimate the appropriate timing.
Prognosis
The prognosis depends upon the severity, stage, and treatment. Recurrence of varus and increasing shortening are common during childhood. Persisting articular deformity often leads to degenerative arthritis in adult life.
Torsion
Torsional problems of in-toeing and out-toeing often concern parents and frequently prompt a variety of treatments for the child. Management of torsional problems is facilitated by clear terminology, an accurate diagnosis, a knowledge of the natural history of torsional deformity, and an understanding of the effectiveness of management options.
Terminology
Version
describes normal variations in limb rotation [A]. Tibial version is the angular difference between the axis of the knee and the transmalleolar axis. The normal tibia is laterally rotated. Femoral version is the angular difference between the transcervical and transcondylar axes. The normal femur is anteverted.
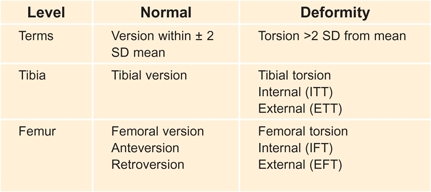
A Terminology of rotational variations Normal variations and deformities are described by different terms.
Torsion
describes variation beyond ±2 standard deviations (SD) from the mean and is considered abnormal and described as a “deformity.” Internal femoral torsion (IFT) or antetorsion, and external femoral torsion (EFT) or retrotorsion, describe abnormal femoral rotation. Internal tibial torsion (ITT) and external tibial torsion (ETT) describe abnormal tibial rotation.
Torsional deformity may be simple, involving one level, or complex, involving multiple segments. Complex deformities may be additive or compensating. Thus, internal tibial torsion and internal femoral torsion are additive. In contrast, external tibial torsion and internal femoral torsion are compensatory.
Normal Development
The lower limb rotates medially during the seventh fetal week to bring the great toe to the midline. With growth, femoral anteversion declines from about 30° at birth to about 10° at maturity [B]. Values for anteversion are higher in the female and in some families [C]. With growth, the tibia laterally rotates from about 5° at birth to a mean of 15° at maturity. Because growth is associated with lateral rotation in both the femoral and tibial segments, medial tibial torsion and femoral antetorsion in children improve with time. In contrast, lateral tibial torsion usually worsens with growth.
B Lower limb laterally rotates with age Both the femur and tibia laterally rotate with growth. Femoral anteversion declines and tibial version becomes more lateral.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








