75
Transverse Deficiency of the Digits
Scott H. Kozin
History and Clinical Presentation
A 10-month-old boy presented with a congenital anomaly of the right hand (Fig. 75–1). He is the product of a full-term normal vaginal delivery. There were no complications during pregnancy or delivery. The child uses the right hand for bimanual activity and is otherwise healthy. Developmental milestones have been reached at the appropriate time. He is an only child, and there is no family history of congenital anomalies.
PEARLS
- Transverse deficiencies of the digits are most common at the phalangeal level.
- Deficient hands with intact metacarpophalangeal joints and small proximal phalanges are very adept at function.
- Nonvascularized toe phalangeal transfer requires extra-periosteal dissection.
PITFALLS
- Nonvascularized toe phalangeal transfer does not result in prolonged growth.
- Distraction osteogenesis requires frequent monitoring to avoid potential complications.
- Toe-to-hand transfer is difficult in adactyly and may require multiple toe transfers.
Physical Examination
A healthy-appearing infant with an isolated anomaly of the right upper extremity. The right shoulder, elbow, forearm, and wrist appear normal and equal in size when compared with the left side. The right hand is abnormal with absence of the thumb, index, long, ring, and small digits (Fig. 75–2). There are palpable metacarpals, but no phalanges appreciated. There is excellent skin coverage and skin tubes are present where the phalanges would be expected. No amniotic bands or chest wall abnormalities were noted.
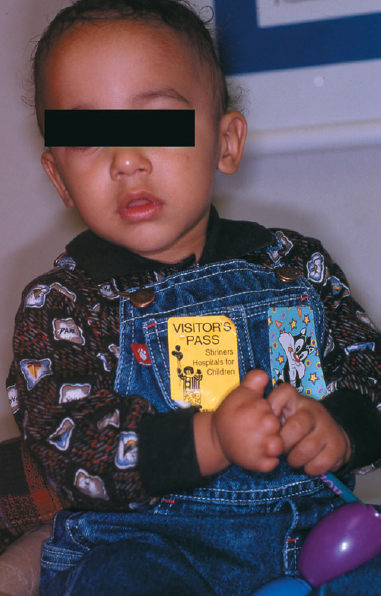
Figure 75–1 A 10-monthold with congenital anomaly of the right hand.

Figure 75–2 Anomalous right hand with absent thumb, index, long, ring, and small digits.
Diagnostic Imaging
Radiograph of the right hand demonstrated five metacarpals with absent phalanges (Fig. 75–3). A comparison radiograph of the left hand revealed five metacarpals and normal phalanges.

Figure 75–3 Radiograph of right hand with normal metacarpals and absent phalanges.
Differential Diagnosis
Brachydactyly
Poland syndrome
Transverse deficiency of the digits
Constriction band syndrome
Brachydactyly refers to a short hypoplastic digit that has the normal complement of bones. The index and small fingers are most commonly affected. The shortening most commonly involves the middle phalanx, which is the last phalanx to ossify. Poland syndrome combines hand hypoplasia with chest wall abnormalities and is usually sporadic in occurrence. The most common hand anomaly is symbrachydactyly (syndactyly combined with brachydactyly), and the typical chest abnormality is ipsilateral absence of the sternocostal portion of the pectoralis major muscle. Constriction band syndrome is a result of entrapment of developing embryonal tissue by fetal lining. Mild band formation can cause simple constriction rings that are primarily a cosmetic deformity, whereas severe bands can cause autoamputation of the digits. As in transverse deficiency of the digits, the thumb is often spared. The diagnosis of constriction band requires the presence of a constriction band either in the hand or elsewhere.
Diagnosis
Transverse Deficiency of the Digits
Transverse deficiency of the digits is most common at the phalangeal level with complete absence of the phalanges (aphalangia) or presence of only the proximal phalanx bases. There may or may not be nail remnant and vestigial tendons, and rudimentary neurovascular structures. The central digits are most commonly deficient and the thumb is often spared. The incidence of transverse deficiencies in the upper extremity is ∼ 1.5 in 10,000 births, which includes transverse deficiencies at the digits level.
Nonsurgical Management
The initial treatment for transverse deficiencies of the digits is nonoperative. The parents are often devastated and require support and education. Parents often feel guilty about this anomaly and have lots of questions. A team that consists of a physician, therapist, and social worker often provides sufficient information for the family. We attempt to explain to the parents that transverse deficiencies are usually sporadic in occurrence and not associated with other syndromes. This defect most likely affected the limb bud covering (apical ectodermal ridge) early during pregnancy (between 4 and 8 weeks of gestation). We also stress that the parents attempt to treat the child as normal as possible, as the child does not know he or she is different. In addition, the child will develop many adaptive maneuvers to achieve a variety of activities. These manipulations are necessary for independent function and are part of normal development in the child with a transverse deficiency.
Surgical Management
Hands with transverse deficiencies through the carpus and absent metacarpals are not amenable to surgical correction. The remaining carpus allows wrist range of motion, and the extremity is used primarily as a helper for bimanual activity. Prosthetic fitting is an option in these children, although the acceptance rate is low because of the adequate limb length, intact sensation, and available wrist motion. Adaptive equipment can be used to supplement hand function for a particular task that cannot be accomplished (e.g., tying shoes, playing musical instruments).
Deficient hands with short proximal phalanges and intact metacarpophalangeal joints have good potential for function, as the shortened digits can be used for crude grasp and have normal sensibility. These hands have the potential for surgical reconstruction aimed at improving length. There are multiple methods to increase digital length including web space deepening, bone grafting, on-top plasty, distraction osteogenesis, or toe-to-hand transfer. Web deepening is indicated when there is a combination of syndactyly and digital deficiencies. The commissure should be placed as proximal as possible to achieve a relative lengthening of the separated digits. Intercalary bone grafting and on-top plasty are most applicable during first web space reconstruction (see Case 79, Hypoplastic Digits and Hands). An index metacarpal can be excised during first web space reconstruction and used as bone graft to increase length of the thumb or long finger. In addition, an index proximal phalanx can be harvested as a neurovascular flap and transferred to the tip of the thumb to augment length and function (Fig. 75–4).
Distraction osteogenesis can be applied to these hands, but there is little tolerance for error. The small size of the phalanges and technicalities of external fixation application are important preoperative considerations. Distraction lengthening is usually reserved until the bone is large enough to accommodate the fixator device and the child old enough to comprehend the external fixator. The distraction is performed slowly at 1 mm per day with careful pin and soft tissue monitoring. Therapy is required to prevent contracture formation, and weekly radiographs are necessary to assess callus formation and consolidation. Distraction osteogenesis can double the lengthened segment, but the regenerate bone is prone to fracture, and the external fixator must remain in place for three times the duration of the lengthening to allow for bony consolidation.
Transverse deficiency without phalanges is more difficult to manage surgically as the options for treatment diminish. Lengthening of the metacarpals may provide a pinch post in hands with an adequate thumb (Fig. 75–5). However, metacarpal lengthening does not result in motion and is contraindicated when there are other digits that possess good motion. In these cases, a long stiff finger hinders hand function because it interferes with the mobile digits. Nonvascularized toe phalangeal transfer is an option in hands without phalanges (aphalangia) and can use any of the toes as a donor. The donor phalanx is harvested in an extraperiosteal fashion (Fig. 75–6). The phalanx is removed along with the metacarpophalangeal collateral ligaments and a portion of the volar plate. The toe phalanx is placed within the soft tissue sleeve of the recipient finger. An adequate skin tube must be present to prevent disruption of blood supply to the skin and subsequent tip necrosis. The collateral ligaments are sutured to the metacarpal and any vestigial tendons are sutured to the transferred phalanx. The transferred phalanx and the donor toe are pinned with a 0.035- or 0.045-inch longitudinal Kirschner wire (K wire). Both the lower and upper extremities are placed in a cast with the pins covered. The foot is placed in a walking cast and the pin removed between 3 and 4 weeks after surgery. The transferred phalanx K wire is maintained for 10 to 12 weeks time. This technique adds additional bone and creates a metacarpophalangeal joint. However, the ensuing growth of the transferred phalanx is limited with mild growth only for a few years.










