Transforaminal Posterior Lumbar Interbody Fusion
Jeffrey A. Rihn
Sapan D. Gandhi
Todd J. Albert
Lumbar fusion is used to successfully treat many pathologies of the lumbar spine that cause instability and neurologic compromise, including tumor, trauma, infection, and most commonly, degenerative conditions. Lumbar fusion can be performed posterolaterally, anteriorly, or both. Posterolateral fusion is achieved between the transverse processes and across the facet joints. Anterior fusion is achieved within the interbody space. A number of approaches to lumbar interbody fusion have been described including posterior, transforaminal, direct lateral, and anterior. The posterior lumbar interbody fusion (PLIF) was thought to be first introduced by Cloward (5). While this technique increased in popularity because of its ability to achieve 360-degree arthrodesis from a posterior approach, it requires significant neural retraction for disc space preparation and cage/bone graft insertion. The transforaminal lumbar interbody fusion (TLIF) technique, a slight modification of the PLIF, was introduced by Harms in 1993 and has become the most common approach for obtaining a combined anterior and posterolateral fusion through a single posterior incision (8). The benefit of the TLIF over the PLIF is that it involves a unilateral approach to disc space preparation and cage/bone graft insertion that can be achieved with minimal retraction of the traversing nerve root. Numerous publications have reported the safety and efficacy of the TLIF approach to achieving a lumbar fusion (2,7,12,19,22,27,29). This chapter describes the surgical technique of the TLIF and the associated perioperative considerations.
INDICATIONS/CONTRAINDICATIONS
Previously reported indications for the TLIF include lumbar spondylolisthesis (both degenerative and isthmic), degenerative scoliosis, recurrent disc herniation, and degenerative disc disease (DDD). To maximize potential benefit from surgery, confirmatory imaging should correspond to the patient’s symptoms and signs. In patients with considerable disc collapse or spondylolisthesis, anterior column support in the form of an interbody cage may be needed to adequately address the spinal pathology and may improve the chances of obtaining a successful fusion (i.e., greater surface area for fusion compared to a posterolateral fusion alone). Distraction of the interbody space through placement of an interbody cage can indirectly decompress the foramen in cases of severe neuroforaminal stenosis. In cases of degenerative scoliosis, insertion of the interbody cage on the side of the concavity of the curve can help neutralize the disc space and restore a more normal alignment.
The transforaminal approach to interbody fusion is not possible to perform in patients with conjoined nerve roots, as the low take off of the exiting nerve root does not allow for the transforaminal approach to the disc space. Conjoint nerve roots can typically be identified on preoperative MRI. If it is unilateral, then the TLIF can be performed from the contralateral side. If the conjoint nerve roots are bilateral, then an anterior approach should be performed for the interbody fusion. Similarly, TLIF in patients with recurrent disc herniation and scar tissue formation can be challenging, as the traversing nerve root of the affected level is often bound by scar tissue and difficult to mobilize enough to safely perform the interbody fusion. Patients with considerable
osteoporosis or bony destruction from tumor or infection are typically not considered candidates for a TLIF, although reports of treating discitis/osteomyelitis using this approach have appeared in the literature (30). Intact endplates are important when performing a TLIF. Endplate destruction by the pathologic process or endplate violation at the time of the procedure will lead to subsidence of the interbody cage and potentially a less desirable result.
osteoporosis or bony destruction from tumor or infection are typically not considered candidates for a TLIF, although reports of treating discitis/osteomyelitis using this approach have appeared in the literature (30). Intact endplates are important when performing a TLIF. Endplate destruction by the pathologic process or endplate violation at the time of the procedure will lead to subsidence of the interbody cage and potentially a less desirable result.
PREOPERATIVE PREPARATION
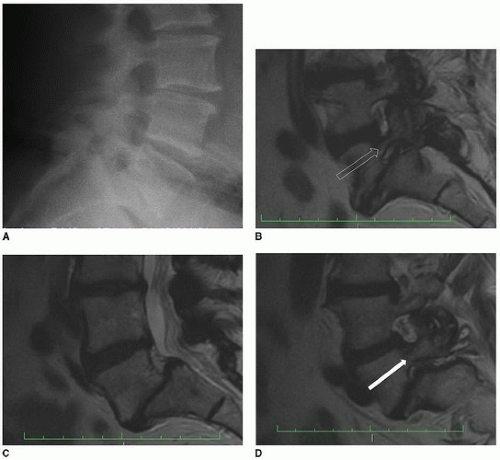
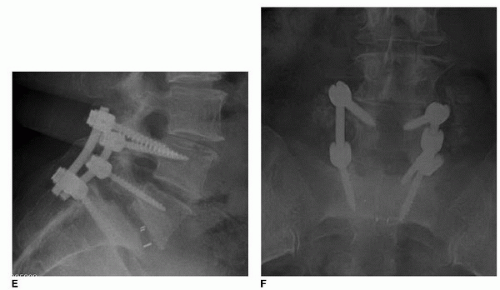
Prior to surgery, imaging studies (i.e., plain radiographs, MRI, and/or CT scan) should be carefully reviewed and used to generate a surgical plan. Patient pathology (e.g., recurrent disc herniation, pars defects, degree of spondylolisthesis and collapse, sacral doming, pedicle anomalies) and variations in patient anatomy (e.g., lumbosacral variations that affect numbering of lumbar vertebrae, conjoint nerve root) should be clearly identified. Patients with isthmic spondylolisthesis, particularly in higher grade slips, may have dysmorphic pedicles or doming of the sacrum that makes the TLIF approach challenging (Fig. 26-1A-F). The pedicles can be dysmorphic, with a very small diameter, that can preclude screw placement. This is not an uncommon finding at the L5 level in cases of a high-grade L5/S1 isthmic spondylolisthesis. In these cases, it may be necessary to instrument and fuse up to the L4 level to allow adequate stabilization. Furthermore, significant sacral doming can make cage placement difficult. The shape of the endplates of the involved level(s) should be clearly defined on preoperative imaging, and a plan for cage placement and positioning should be made in the preoperative planning stages. In very high-grade spondylolisthesis (grade IV), the degree of slippage and endplate deformity may preclude interbody fusion. In these cases, an alternative procedure is often preferable, in which case a fibular strut allograft is inserted, from either a posterior or anterior approach, through the L5 and S1 bodies and across the L5/S1 disc space. The details of this procedure are beyond the scope of this chapter.
Bone graft options should be considered in the preoperative planning stages, and a discussion of such should be had with the patient. The options for bone grafting include local autograft bone, iliac crest autograft bone, allograft bone, demineralized bone matrix, synthetic bone graft material (e.g., beta tricalcium phosphate), and/or recombinant bone morphogenetic protein-2 (rhBMP-2). There is no perfect bone graft option, and each of the above options has both benefits and downsides. Iliac crest bone graft has traditionally been considered the gold standard for lumbar spine fusion. However, high rates of donor-site complications and increased operative time have led to a shift toward alternatives to iliac crest autograft (22). Graft extenders used in combination with autologous bone graft or recombinant bone morphogenetic protein-2 (rhBMP-2)-soaked collagen sponges may help increase fusion rates and decrease rates of pseudarthrosis. The use of rhBMP-2 for TLIF is considered “off-label” in regard to its FDA status. While rhBMP-2 seems to improve fusion rates and decrease donor-site complications, it has been associated with complications such as vertebral osteolysis and postoperative radiculitis (22,23).
TECHNIQUE
Patients are typically positioned on a radiolucent Jackson table with the abdomen hanging free and with all bony and soft tissue protuberances well padded. Allowing the abdomen to hang free reduces venous pressure and minimizes blood loss. An additional benefit of the Jackson table is that it is radiolucent, thus allowing intraoperative fluoroscopy and/or plain radiographic images in both the anteroposterior and lateral views to confirm instrumentation and interbody cage placement. The Jackson table also allows for a lordotic lumbar alignment that helps to prevent fusing the involved levels in a kyphotic position.
After prepping and draping, a longitudinal incision is made in the midline over the spinous processes of the involved levels. Intraoperative fluoroscopy/radiographic and/or palpable anatomical landmarks can be used to localize the incision site. The posterior superior iliac spine is typically at the level of the L5-S1 interspinous level, and the iliac crest is typically at the level of the L4 spinous process. Subperiosteal dissection of the posterior elements (spinous processes, lamina, pars, and transverse processes) of the involved levels is accomplished using electrocautery. Great care should be taken to not violate the facet joints adjacent to involved levels during the exposure. Intraoperative fluoroscopy/radiography should be used to confirm the surgical level.
Once an adequate exposure is obtained, attention is turned toward the decompression portion of the procedure. The nature of the pathology dictates the nature and extent of the decompression. When treating an isthmic spondylolisthesis, a Gill laminectomy is performed by removing the spinous process, lamina, inferior articular processes, and pars of the involved level as one fragment of bone, that is, the Gill fragment (e.g., L5 in the case of an L5-S1 isthmic spondylolisthesis) (6). This is accomplished by dividing the interspinous ligaments above and below the involved level (e.g., L4-L5 and L5-S1 interspinous ligaments), the bilateral facet capsules, and any ligamentum flavum attachments to the Gill fragment. The Gill fragment can typically be removed as a single bony fragment. The removal of the Gill fragment exposes the underlying epidural fat and dura, as well as the superior articular processes of the caudal level involved in the spondylolisthesis (e.g., S1 superior articular processes in an L5-S1 isthmic spondylolisthesis). When performing a TLIF for a unilateral pathology (e.g., recurrent disc herniation, foraminal disc herniation, facet cyst) or a degenerative scoliosis that does not require a full laminectomy, an osteotomy is performed through the pars and lamina of the cranial vertebra of the involved disc level. Such an osteotomy allows removal of the pars and inferior articular process of the cranial vertebra, thus exposing the underlying superior articular process of the caudal vertebra and allowing access to the foramen on the side from which the TLIF is to be performed. Once the superior articular process is exposed, the ligamentum flavum is removed, and the underlying pedicle of that superior articular process is skeletonized using a Kerrison rongeur. This allows identification of the exiting and traversing nerve roots of the involved level.
The triangle through which the TLIF is performed is defined by the inferior border of the exiting nerve root, the lateral border of the traversing nerve root, and the pedicle and posterior aspect of the superior endplate of the caudal vertebra (Fig. 26-2). There are usually epidural veins overlying the disc space in this triangle that should be divided using bipolar electrocautery. If excessive bleeding is encountered that cannot be controlled with the bipolar, thrombin-soaked Gelfoam or Floseal (Baxter, Deerfield, IL) can be used to obtain hemostasis. The traversing nerve root is gently retracted medially using a nerve root retractor. If present, the disc herniation is removed, and the annulus is incised using a no. 15 blade scalpel. Great attention should be given to the exiting nerve root to avoid injury. Excessive manipulation of the dorsal root ganglia of the exiting nerve root can lead to postoperative neurogenic pain. In cases of spondylolisthesis and significant disc collapse, there is often a bony lip arising from the superior endplate of the inferior vertebral body of the involved level (Fig. 26-3). After entering the disc space with a scalpel, this bony lip should be removed using a Kerrison rongeur. Removal of this lip will facilitate disc removal and cage placement. Through the annulotomy, the intervertebral space is debrided free of all accessible disc and cartilaginous material back to bleeding endplate bone. This is accomplished using a series of curved and straight curettes and/or chondrotomes, endplate scrapers, double-angled curettes, and straight and angled pituitary rongeurs. The double-angled curette is effective in removing the contralateral disc and cartilaginous material (Fig. 26-4). There are numerous designs of instruments used to remove disc and cartilaginous material from the disc space. The manufacturer providing the implants typically makes these instruments available to the surgeon. The surgeon should be familiar with the options when it comes to disc space preparation instruments and should choose those with which he/she is most comfortable. Cadaver studies have reported that approximately 70% of the disc can be removed through a unilateral TLIF approach (11,13




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree