Lumbar Microdiscectomy
C. Chambliss Harrod
Roman Trimba
Alan S. Hilibrand
BACKGROUND/ANATOMY
The lumbosacral spine is the region of the skeleton that transitions from the appendicular to the axial skeleton. Ambulation is most functional when the head is centered over the pelvis in both the coronal and sagittal planes, which are typically balanced in adult patients with cervical and lumbar lordosis counteracting thoracic and sacral kyphosis. Walking places significant biomechanical loads across the lumbosacral junction. Approximately 80% of the weight is supported via the anterior column consisting of vertebral bodies and intervertebral discs, while the posterior bony and ligamentous structures including the neural arches and zygapophyseal (facet) joints accommodate approximately 20%. Typically, the lordotic lumbar spine consists of five nonrib-bearing, mobile osseous segments between the rigid thoracic and fused sacral vertebrae, which serve as a conduit for the cauda equina. Normal lordosis ranges from 40 to 60 degrees with over 50% stemming from L4-S1 as the lumbosacral intervertebral disc is often much taller ventrally than dorsally. Normal lower extremity function depends on mobile joints powered by musculotendinous units, which derive their neurologic innervation via nerve roots stemming from the spinal cord, conus medullaris, and cauda equina.
INDICATIONS/CONTRAINDICATIONS
Compression of the neurologic elements can be secondary to degenerative, neoplastic, congenital, infectious, or traumatic etiologies, although herniation of lumbar nucleus pulposus through the peripheral annulus is most common. Patients are often present with lower extremity radiculopathy (combination of pain, weakness, numbness, paresthesias, loss of function) though bowel, bladder, and autonomic nervous system abnormalities culminating in cauda equina syndrome are possible. Nonoperative management is effective in the vast majority of cases with activity modification, physical therapy, medication, and interventional pain management techniques. Absolute indications
for surgical treatment include progressive neurologic deficit and cauda equina syndrome. Relative indications include recalcitrant pain after failed conservative management. Analysis of disc location, size, and extent and surgical goals allows the correct approach to achieve the surgical goal— decompression of neural elements while maintaining spinal stability. Disc herniations can be located centrally, paracentrally, foraminally, or extraforaminally. Removal of offending compressive lesions under direct vision has been the standard of care over thermal ablative techniques. Posterior-based approaches are utilized below the level of the conus medullaris and include midline, paramedian (Wiltse), or far lateral open, tubular, endoscopic, or arthroscopic techniques with laminectomy, hemilaminectomy, hemilaminotomy, or transforaminal (foraminoplasty) bony resections to perform the discectomy. Each of these techniques has its own unique advantages and disadvantages. Experience of the surgeon, cosurgeon availability, and familiarity with the approach and anatomy of the patient are of utmost importance when deciding on which approach to use. Additionally, most surgeons use loupe magnification or the operating microscope to improve visualization and safety. Studies have shown that results of lumbar microdiscectomy have been superior to traditional techniques (subtotal or complete discectomy). We have enjoyed a low complication profile with use of a 2- to 3-cm open midline or Wiltse paramedian approach to treat nearly all primary recalcitrant symptomatic lumbar disc herniations under loupe magnification. We discuss this approach in the following technique.
for surgical treatment include progressive neurologic deficit and cauda equina syndrome. Relative indications include recalcitrant pain after failed conservative management. Analysis of disc location, size, and extent and surgical goals allows the correct approach to achieve the surgical goal— decompression of neural elements while maintaining spinal stability. Disc herniations can be located centrally, paracentrally, foraminally, or extraforaminally. Removal of offending compressive lesions under direct vision has been the standard of care over thermal ablative techniques. Posterior-based approaches are utilized below the level of the conus medullaris and include midline, paramedian (Wiltse), or far lateral open, tubular, endoscopic, or arthroscopic techniques with laminectomy, hemilaminectomy, hemilaminotomy, or transforaminal (foraminoplasty) bony resections to perform the discectomy. Each of these techniques has its own unique advantages and disadvantages. Experience of the surgeon, cosurgeon availability, and familiarity with the approach and anatomy of the patient are of utmost importance when deciding on which approach to use. Additionally, most surgeons use loupe magnification or the operating microscope to improve visualization and safety. Studies have shown that results of lumbar microdiscectomy have been superior to traditional techniques (subtotal or complete discectomy). We have enjoyed a low complication profile with use of a 2- to 3-cm open midline or Wiltse paramedian approach to treat nearly all primary recalcitrant symptomatic lumbar disc herniations under loupe magnification. We discuss this approach in the following technique.
PREOPERATIVE PLANNING
Understanding of anatomy and radiographic data will facilitate preoperative planning, allowing a smaller incision, with less dissection, blood loss, and tissue trauma. A careful physical examination should inspect for any prior incisions, scars, skin lesions (i.e., psoriasis or acne), infection, or signs of spina bifida (dimpling, hairy tufts, and lack of spinous processes). Morbidly obese patients can increase the difficulty of the operation, necessitating increased radiation to identify one’s level, larger incisions, longer instruments, and longer operating times.
Lumbar spine imaging must include plain radiography with anteroposterior and neutral, flexion, and extension lateral views to clearly identify the lumbosacral junction, the 12th (or most caudal) rib, the number of lumbar vertebrae, presence of transitional (or sacralized) vertebrae, and superimposed level of the iliac crest. Adequate plain radiographs aid in preventing wrong-level surgery. Flexionextension views allow identification of instability, while oblique views are occasionally helpful in identifying pars interarticularis fractures. Computed tomography is of limited importance though can be helpful to quantify the amount of foraminal stenosis and osteophytic compression. In revision lumbar spine surgery with instrumentation and for patients who cannot undergo magnetic resonance imaging (MRI), addition of myelography is helpful to identify disc herniations and stenosis. MRI best assesses the extent of nerve root, thecal sac, conus medullaris, or spinal cord compression with or without intradural extension. Gadolinium administration with enhancement is useful with neoplasms, infections, revision microdiscectomy cases, and as an aid in diagnosing an early reherniation. T1 parasagittal images are vital in assessing the amount of foraminal root compression in far lateral disc herniations. Rarely, an anomalous or bifid nerve root may also be identified that will alter decompression tactics. In addition, engorged epidural plexi should be noted as occasionally large ventral epidural leashes will be encountered and can be difficult to control. Lastly, we typically require a recent MRI (within 3 months) prior to performing surgical decompression as lumbar disc herniations can resorb over that period of time.
In order to minimize incision length and bony removal, while still obtaining adequate decompression, one must understand the exact location of the disc herniation prior to surgery. Lesions can be characterized using the McCulloch “three-floor anatomic house,” which provides a three-dimensional grid of the spinal canal. Vertically, the house is broken down into three floors (Fig. 22-1). The most inferior or caudal floor contains the disc level (“1”). The second floor extends from the inferior border of the pedicles to the inferior endplate and contains the foraminal level. The third or most cephalad is the pedicle level and spans from the superior endplate to the inferior border of the pedicle. One flaw in this vertical system is that it is designed for cranial migration of discs (i.e., an L4-L5 disc migrating toward the L4 pedicle). Caudal disc herniations are given the nomenclature of a “minus-one” (-1) level. An example would be an L3-L4 disc migrating to the level of the pedicle of L4. Disc pathology is further divided in the sagittal plane from medial to lateral into central, subarticular (lateral recess), foraminal, and extraforaminal (far lateral) zones (Fig. 22-2). Medially, the central zone is situated between the edges of the dura, while the subarticular (lateral recess zone) sits between the lateral edge of the dura and the medial borders of the pedicles. The foraminal zone lies from the medial to lateral border of the pedicle, and the extraforaminal zone is lateral to the pedicles. The seven posterior bony elements include the superior and inferior articular processes, spinous process, lamina, pedicle, transverse process, and pars. The pedicle and transverse process are the only ones that lie in a single floor, the third or pedicle level. All other structures straddle two floors.
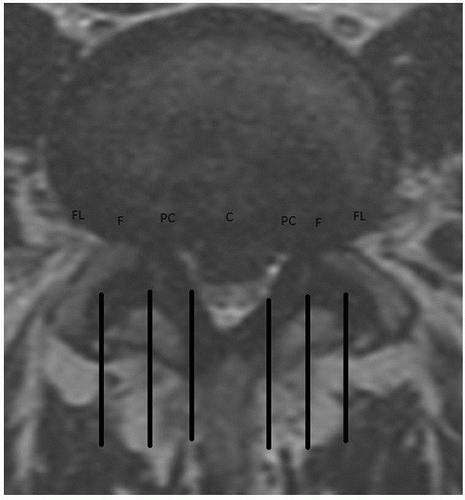 FIGURE 22-2 A T2-weighted axial MRI image at the L4-L5 disc level from Figure 22-1 demonstrates a central disc herniation with lateral recess stenosis with compression of the caudal equina. The patient clinically had left-sided radiculopathy, so a left-sided hemilaminotomy with microdiscectomy was planned with a low threshold to convert to either bilateral hemilaminotomy or laminectomy if the appropriate-sized fragment was not removed. The central (C), paracentral (PC), foraminal (F), and extraforaminal or far lateral (FL) zones are defined. |
TECHNIQUE
Anesthesia
The majority of microdiscectomies are still performed under general anesthesia; however, some patients opt for spinal and/or epidural anesthesia. The degrees of sedation are determined according to the preference of the patient and/or surgeon. While a small percentage of patients chose to be awake and watching the procedure on the television monitor, the majority prefer to be unconscious. An epidural anesthetic dilates the vessels in the lower extremities, resulting in lower intraoperative bleeding. It is also associated with lower recovery room times, faster return to orientation and alertness, and general absence of postoperative nausea and vomiting compared to a general anesthetic. However, there are several disadvantages to using an epidural or local anesthetic. The peripheral vasodilation caused by the epidural may lead to general hypotension. Lack of general anesthesia and complete sedation may cause difficulty with patient positioning and moving during the procedure, as well as difficulty establishing an emergency airway in case of a complication. Increased incidence of urinary retention with epidural anesthetic may lead to an overnight stay during what would normally be an outpatient procedure. Neurologic complications may also result from the epidural anesthetic/procedure itself; the anesthesiologist may inadvertently cause a dural tear necessitating a repair.
Patient Positioning
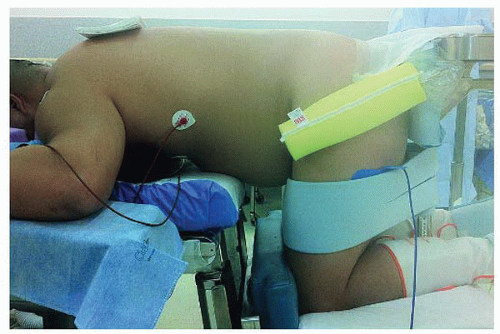
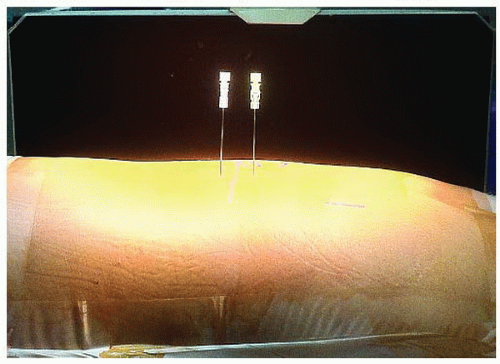
Careful patient positioning can facilitate a successful lumbar microdiscectomy. The first is to minimize lumbar lordosis as much as possible. This will increase the interlaminar space allowing for easier access into the spinal canal and resulting in a smaller laminotomy to expose the disc. The second goal is to decrease abdominal compression to decrease venous pressure, which results in markedly reduced epidural blood loss and enhanced intraoperative visualization. This can be accomplished with the Andrews frame in a knee-chest position. The patient is placed with his/her back parallel to the floor with the knees and hips flexed to an angle slightly greater than 90 degrees with the frame kneeling angle increased to maximum. The patient should be positioned prone on an Andrews frame or table if the patient weighs less than 250 pounds; otherwise, a Jackson table with a sling is preferred to allow the abdomen to hang freely to decrease venous congestion and subsequent epidural venous bleeding (Fig. 22-3). The Andrews frame is secured to a regular operating room table with the legs flexed to the floor (the surgeon or assistant should test with his or her own weight that the frame is rigidly affixed prior to patient placement). The patient must be rolled prone onto the table, knees are secured initially with both feet strapped in place, a buttocks plate is placed at the appropriate height, and then the patient is translated caudally. A semifirm gel bolster is used as a chest or sternal roll and must be 2 cm caudal to the sternal notch to not impinge on the airway or cause cranial vascular engorgement. The arms are then gently rotated into a “90-90” position, and care must be taken to pad bony prominences and ensure the safety of the peripheral nerves and brachial plexus. The surgeon must then ensure that the patient’s back is parallel to the floor by either raising or lowering the legs or more typically cranking the tibial tray up or down. Finally, lateral bolsters are squeezed on the midthighs to ensure patients are safely and securely fastened. Note that patients should be examined preoperatively for adhesive capsulitis (frozen shoulder) or shoulder pathology as those with such disorders will not be able to be positioned with the arms in the “90-90” position. They will require the arms to be at the side, which should be low enough not to block the marker radiograph. We typically drape out the operative field widely with 1,010 drapes and then mark the iliac crests transversely; the posterior superior iliac spines are vertically marked bilaterally. After scrubbing skin and prepping with ChloraPrep, a World Health Organization (WHO) “time out” is performed to verify the details of the procedure and equipment and review major intraoperative risks with the anesthesia, surgical, and nursing teams.
Localization of the Level
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree