Sacropelvic Fixation
Han Jo Kim
Keith H. Bridwell
INDICATIONS/CONTRAINDICATIONS
Sacropelvic fixation involves the use of pelvic fixation methods for the purpose of protecting S1 screws in fusions performed to the sacrum. The reason for this is inherent to the anatomic characteristics of the S1 pedicle—which is patulous, cancellous, and usually comprised of thin cortical bone. Therefore, excessive stress on the S1 screw can result in screw loosening, pullout, loss of fixation, and pseudarthrosis. The indications for sacropelvic fixation therefore include (5)
Long fusions to the sacrum in adults (proximal fusion level L2 or above)
Short lumbosacral fusions under settings of severe osteoporosis
High-grade spondylolisthesis at L5-S1 (greater than 50% slip)
Flat-back deformity requiring three-column osteotomy
Correction of pelvic obliquity
Sacral fractures with spinopelvic dissociation
Tumor resection after sacrectomy
From a conceptual standpoint, constructs that will result in huge biomechanical stresses on the S1 screws will require use of sacropelvic fixation. This includes constructs that provide a substantial amount of coronal or sagittal plane corrections.
Contraindications for sacropelvic fixation are analogous to surgical contraindications for fusions involving the sacrum. If there is absolute certainty as to obviate the use of pelvic fixation for a fusion to the sacrum, sacropelvic fixation is not necessary and should not be performed since pelvic fixation does increase operative times and can increase total operative blood loss.
PREOPERATIVE PREPARATION
Decision making on fusing adult curves to the sacrum is based in part on the patient’s complaints and where the principal pain seems to be (i.e., the thoracic spine, the thoracolumbar junction, or the distal lumbar spine). Appropriate bending films are helpful as well as upright films. It is most helpful that the upright films be long cassette to assess overall balance. 14 × 17 inches anteroposterior (AP) and laterals may be helpful to discern individual and regional segment pathology. Flexibility films that are helpful include a long cassette supine AP x-ray and right- and left-side benders. A supine hyperextension x-ray will help determine the flexibility in the sagittal plane. Also, what we have termed a “push-prone” x-ray may facilitate decision making as to the flexibility of the various curves in the coronal plane. What is usually assessed is the flexibility of the main lumbar curve from T10 or T11 down to L4 and then the fractional curve below, which extends from L3 to the sacrum. The flexibility of that curve from L3 to the sacrum and the degree of degeneration of those segments are part of the decision-making process on whether or not to extend to the sacrum.
MRI evaluation is helpful to determine the extent of disc degeneration at L4-L5 and L5-S1. The study also shows whether there is substantial central, lateral recess or foraminal stenosis at those segments. The parasagittal views are most helpful in assessing stenosis at L4-L5 and L5-S1 foramen. The MRI study is more helpful to evaluate the fractional curve from L4 to the sacrum than it is to evaluate the primary curve where extensive rotation makes visualization difficult. Extra attention to the orientation of the deformity is necessary by adjusting the gantry and allowing for in plane or perpendicular to plane visualization of the segments.
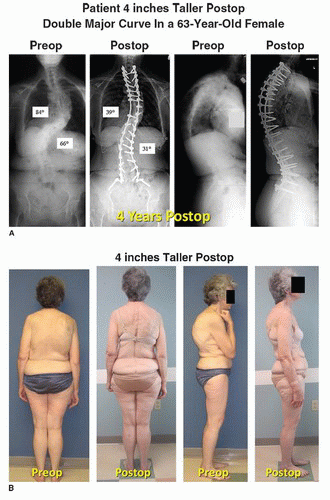
CASE 30-1
A 63-year-old female with complaints of progressive scoliosis and kyphosis. She lost 4 to 5 inches of height over last 30 years. There was no leg pain but increased back pain. A,B: 4 years post-op. Substantial improvement in lumbar back pain (C).
|
|
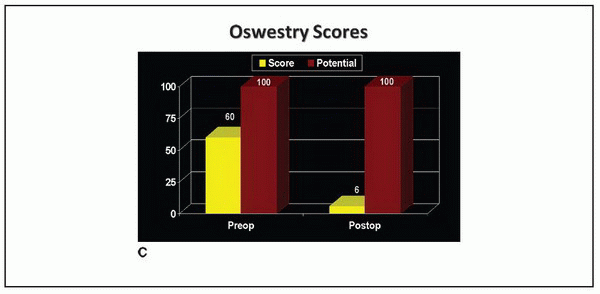
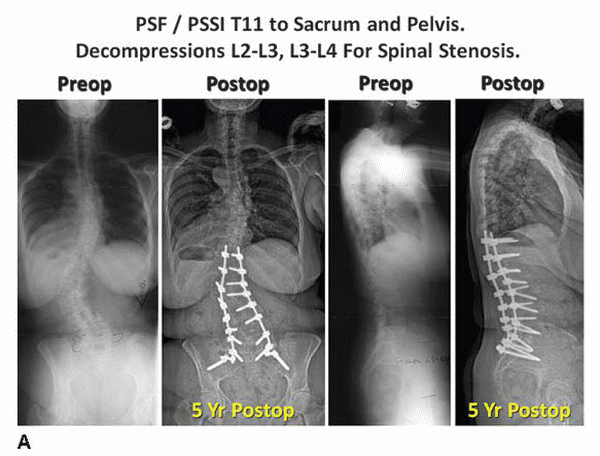
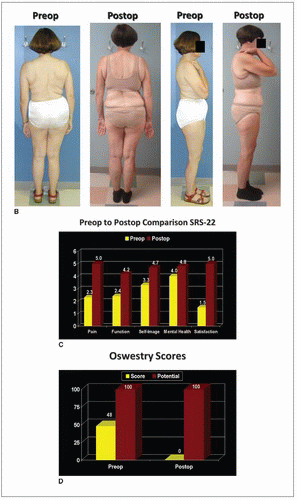
CASE 30-2
A 66-year-old female with progressive adult lumbar scoliosis and severe spinal stenosis at L2-L3 and L3-L4 with substantial spinal claudication symptoms and back pain.
A,B: She underwent a T11-sacrum and pelvis posterior spinal fusion with segmental instrumentation with a decompression at L2-L4. Pre- and post-op clinical photo and radiographs at 5-year follow-up with significant improvement in outcome scores (C,D).
|
|
CASE 30-3
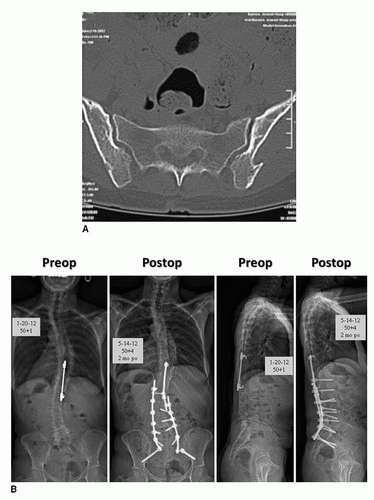
A 50-year-old female with progressive distal junctional degeneration and back pain. She had two surgeries: first a Harrington long fusion to L4 and then a revision for a pseudarthrosis at the thoracolumbar junction. She presented with a T4 to L4 fusion with a single Harrington compression rod around her thoracolumbar junction. A: She had a harvested left ilium from the first surgery and right ilium for the second surgery (see CT scan). B: She underwent a revision T11-sacrum and pelvis PSF/PSSI with a Smith-Peterson osteotomy at L3-L4. A S2 iliac screw was used in the left ilium due to altered anatomy from a prior iliac harvest. Pre- and post-op radiographs are shown.
|
Under the setting of primary surgery, plain radiography is usually sufficient for visualizing the sacrum and pelvis to rule out any congenital anomalies of the sacrum and pelvis such as a bifid sacrum (see Case 30-1). Under the setting of revision surgery, visualization may be difficult due to obscurities from fusion masses and/or from extensive prior iliac crest harvest for bone graft (see Cases 30-2 and 30-3). It is helpful to have a MRI or CT scan study of the pelvis to delineate the anatomy and to demonstrate the extent of prior iliac harvesting to see whether iliac fixation is feasible on one or both sides.
TECHNIQUE
We currently utilize two methods for sacropelvic fixation: iliac screw fixation and S2 iliac screw fixation. With both techniques, we position the patient prone for posterior sacropelvic fixation. To maximize lordosis, use a frame in which the chest, ilium, and thighs are supported, but the thighs are in a relatively extended position. Keep the pads off the anterior superior iliac spine to avoid lateral femoral cutaneous nerve irritation, and flex the knees and feet to take tension off of peripheral nerves. If a long fusion to the sacrum is being performed, then do a wide draping of the patient to accomplish some assessment of spinal balance after the fusion and fixation are completed. So drape out the shoulders as well as the trunk and pelvis.
Surgical Approach for Sacropelvic Fixation with Iliac Screws
A midline skin incision is made to expose the spine from the midline. In particular at L5-S1, we expose out to the tips of the L5 transverse processes, out to the tips of the sacral ala, and then out to the ilium bilaterally. If we are planning to perform S2 iliac screw fixation, we usually do not need to expose out to the ilium.
In the process of exposing the sacrum, we perform more of an extraperiosteal rather than subperiosteal approach to avoid falling into the dorsal sacral foramina, which tend to have substantial veins. The use of Cobb elevators and Hibbs retractors is helpful to lift muscles off of the inner aspect of the ilium on both sides. In particular, the distal aspect of the ilium should be exposed and, to some extent, the lateral aspect of the ilium as well to establish the direction of the iliac screws.
Self-retaining retractors such as Adson-Beckman and deep Gelpi retractors are helpful but have to be placed just proximal to the ilium. Exposing out to the ilium on both sides facilitates the exposure of the sacral ala and the L5-S1 facets and makes accurate placement of S1 bicortical screws easier.
The placement of the bicortical S1 screw is as follows. Identify the confluence between the ala and the lateral facet of S1. Use a burr to find the starting point. Next, use a gear shift to find the way to the anterior cortex of the sacrum. Then check with a ball-tipped probe to be sure that there is still an anterior cortex. Mark the gear shift 5 mm longer, and then, using a mallet, gently tap the gear shift to perforate the anterior cortex of the sacrum. Verify the perforation carefully, and place a bicortical screw. Most commonly, the length of this bicortical screw is 45 mm. The diameter of the sacral screw (if it is going to be protected with an iliac screw) is usually satisfactory at 6.5 mm. It is important to angle in enough lordosis to hit the sacral promontory rather than the sacral endplate if the plan is to place cages or femoral rings in the L5-S1 disc space. Also, it is important to angle medially. If the ilium is in the way or there is insufficient lateral exposure, there is a tendency to not angle the sacral screw medially enough. If the S1 screw comes out laterally rather than medially, there is potential to irritate the L5 root as it is passing underneath the ala.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree