Chapter 114 Total Knee Arthroplasty—Which Implant Do I Prefer for my Patients? International Roundtable Discussion
Dr. Rosenberg:
I think it’s important to keep in mind the changes in implant design as well as surgical technique made as a result of evaluating early outcomes, and that for the most part these have led to systematic improvements in the quality and consistency of TKA. The implants we use now are different in important ways from those reported on in most long term follow-up studies. These longer term studies also reflect a significantly different patient population than that currently presenting for knee replacement. 11 7
It is my pleasure to have these experienced TKA surgeons gathered from around the world to share their thoughts on contemporary total knee issues with us: Steve Haas, Bruno Violante, Hong Zhang, Christopher Hulet, James Stiehl, and John Callaghan.
Let’s start by discussing the evolution of our implant choices. Dr. Callaghan, what is the current TKA of choice in your practice, how did you come to use this particular knee, and how has your thinking evolved?
Dr. Callaghan:
We now have 15-year survivorship of the PFC knee (DePuy, Warsaw, Ind) that I have been using and, other than a few infections, most of which were hematogenous, the only failures were related to polyethylene wear. This particular implant had an issue with the polyethylene used in the early to mid-1900s and we and others have reported this. Hence, in summary, I use a posterior-stabilized design because it allows me to feel comfortable that I have provided the best operation for patients with little as well as maximum deformity. I think the survivorship is similar to cruciate-retaining designs of the same brand. I do, however, think that the literature is clouded because of the variance in polyethylenes used in the late 1980s and 1990s. The implant I use allows for fixed- or mobile-bearing options and I have gone to using the mobile-bearing design for 60% of knees.
Dr. Rosenberg:
Dr. Stiehl:
As I learned more about the deleterious effects of sliding and ploughing wear on polyethylene surfaces, kinematic issues such as poor femoral condylar rollback in many patients, and femoral condylar liftoff with activity, I began to use a posterior cruciate–sacrificing mobile-bearing implant. These implants seemed immune to these problems from long-term studies, and typically offered higher ranges of motion with activity.
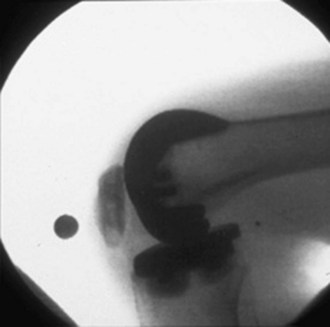
Following my early kinematic studies, I sought methods, such as flexion ligament balancing, that appeared to limit the problems of instability and wear that were often seen with posterior cruciate–retaining, fixed-bearing knees implanted with measured resection methods. I remember a brief conversation with one of the prominent originators of posterior cruciate–retaining implants when I asked if he had seen significant laxity in the lateral compartment in deep flexion. He explained that he witnessed that phenomenon commonly but never recognized a clinical problem with it. He may be correct in his answer to this day, but the kinematics that I could demonstrate on weight-bearing fluoroscopy were truly scary ( Fig. 114-1 ).
Dr. Rosenberg:
Dr. Zhang:
Dr. Rosenberg:
Dr. Violante:
In the early 1990s, I started with a CR design (Genesis, Smith & Nephew), which required managing the PCL, which might be loose, tight, or appropriately balanced. Loose was more desirable in the presence of an optimal flexion space, but a tight PCL led to bad outcomes with lack of flexion, pain, and early tibial loosening.
Because of this early experience and looking more to the anatomy of the knee, I shifted toward a PS design (IB II, Zimmer) to eliminate the PCL management problem and to work on a more easily reproduced surgical technique and more reliable outcomes. So, from the early 1990s I used the IB II and in 1997, switched to the LPS NexGen Legacy (Zimmer), also designed by John Insall.
Dr. Rosenberg: ,
Dr. Hulet:
Dr. Rosenberg:
Dr. Haas:
Dr. Rosenberg: 17 4 16 5
We have not yet talked much about fixed versus mobile bearings. Dr. Stiehl, I know that you have done a lot of research and given a lot of thought to this.
Dr. Stiehl:
Dr. Rosenberg:
Dr. Stiehl:
Second, the problem of tibial tray malrotation on implantation is eliminated with mobile bearings. 22
Mobile-bearing polyethylene adds an important safety factor, in my view. I recently published my retrospective experience evaluating preoperative and postoperative tibial rotation measured with computer navigation, and found that fixed trays tended to be more internally placed and had less internal rotation with flexion compared with the mobile-bearing knees. 22
Dr. Rosenberg:
Dr. Zhang:
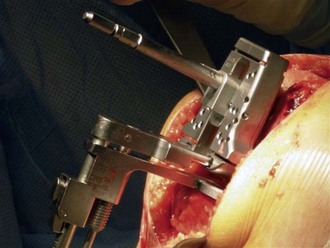
Dr. Stiehl: Fig. 114-2 ). Both implants that I use are particularly stable if a reasonable surgical technique is performed and I can confess not one single bearing dislocation with 15 years of clinical experience. Early on, I avoided mobile bearings in valgus deformities over 20 degrees and, in some severe varus deformities, deferred to a fixed-bearing, posterior-stabilized device, as would be done in total knee revision arthroplasties. Today, I would use the LCS (DePuy) mobile rotating platform or the LPS High Flex mobile (Zimmer) with impunity in any primary total knee setting. The LPS actually has a spin-out stop to limit rotation over 20 degrees in one plane and might be safer for the community surgeon.
I would stongly discourage surgeons from using a measured resection method with a mobile-bearing device. Although measured resection may work in straight forward cases with little deformity, it will fail if there is poor ligament balancing after correction of marked deformity or bone defect and the gaps are not appropriately matched. Mobile-bearing implants are not for the occasional knee surgeon, but more appropriate for the engaged surgeon who is willing to learn from experienced technicians, as I did with my first few.
Dr. Rosenberg:
Dr. Callaghan:
Being as it allows for both fixed bearing as well as mobile bearing the implant I use allows for much versatility. In patients with large valgus deformities, I am a little more apt to use the fixed-bearing design as well as in cases that have tremendous range of motion—that is, more than 140 degrees as I would imagine the patient’s femoral runners run past the tibial inserts which are only designed to obtain 120 degrees of flexion.
Dr. Rosenberg:
Dr. Callaghan:
I have personally reviewed minimum 20-year follow-ups of mobile-bearing designs, performed with polyethylene gamma-irradiated in air, and have seen no loosening over that period. Although the average age of the patients at the time of surgery was 70 years old, I have gained more confidence in believing that these devices have potential for greater long-term durability in the most kinematically challenging patients.
Dr. Rosenberg:
Dr. Violante: 15 10
The polyethylene tibial fixation was subject to micromovements, with subsequent backside polyethylene wear as a cause of tibia lysis in the IB II. In the NexGen Legacy, the polyethylene was compression-molded and gamma-sterilized in inert gas and the polyethylene locking mechanism was reinforced with a posterior dovetail mechanism and peripheral anterior compression.
The cam and post mechanism was also optimized to reduce the risk of posterior dislocation and was moved posteriorly so that the cam engages the post at 75 degrees. High-flexion, specific design geometry variations were made so the patient could safely bend up to 155 degrees. 19, 20
Dr. Rosenberg:
Over time, we made modifications to the implant by creating the Flex design, which allowed for more precise tensioning of the PCL by introducing a larger number of anteroposterior sized implants, and then the Gender design, which allowed for better overall femoral component size matching, medially and laterally, to the individual patient. However, it was particularly gratifying when the kinematic studies that Dr. Stiehl had helped develop demonstrated that our implant design actually produced normal-appearing femoral rollback and minimized liftoff, in comparison to all the other CR designs that Dennis and colleagues 12
Dr. Stiehl, what are the distinguishing features of your current implant choice?
Dr. Stiehl:
The second important advantage is the ability to correct errors with tibial tray placement in terms of rotational position because the device self-corrects with final ligament tension. I have studied this problem extensively with computer navigation and believe that the tibial tray position for a given patient is highly variable and can be affected by anatomic variation, degree of arthritic deformity, and surgical technique.
Dr. Rosenberg:
Dr. Zhang:
Dr. Hulet:
Dr. Haas:
The tibial base plate is also asymmetrical. It allows increased tibial coverage and leads to more accurate rotational alignment. The anatomic shape of the base plate also helps avoid posterolateral overhang, which makes minimally invasive insertion easier. Although there is high coronal conformity medially and laterally, the sagittal conformity is greater on the medial tibial plateau compared to the lateral tibial plateau. This differential geometry helps promote more natural rotational motions with a screw-home mechanism in extension and lateral rollback in flexion.
Dr. Rosenberg:
Dr. Violante: 10
Dr. Rosenberg: 18 6
Dr. Hulet, what about the Jade system?
Dr. Hulet: 1
Dr. Rosenberg:
Dr. Haas:
Dr. Rosenberg:
Dr. Stiehl: 21 ( Figs. 114-3 and 114-4 ).
Only gold members can continue reading.
Log In or
Register to continue
Related
Stay updated, free articles. Join our Telegram channel
Join