Total Humeral Reconstruction
Kristy L. Weber
Total humeral reconstruction is a rare procedure with limited indications. Its use is generally confined to the oncologic patient, and other indications are not extensively discussed here. When performed in the ideal clinical scenario, local control can be achieved while preserving maximal function. Although most tumors that involve the distal humerus are treated palliatively with radiation and limited surgery, extensive lesions can lead to severe pain and loss of function. A limbsparing total humeral resection and reconstruction allows the patient to avoid a disfiguring amputation of the upper extremity and maintain elbow, wrist, and hand function. This chapter outlines total humeral reconstructions using either a prosthesis or an allograft.
INDICATIONS
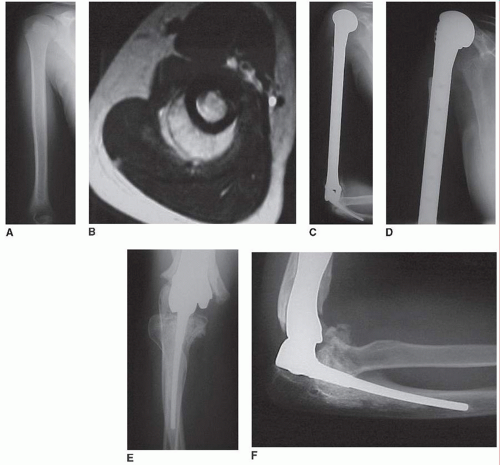
(Most common) Primary malignant bone tumor of the humeral diaphysis that extends too close to the shoulder and elbow to effectively use a diaphyseal intercalary spacer (Chapter 31), a proximal humeral reconstruction (Chapter 29), or a distal humeral reconstruction (Chapter 32) (Fig. 32.1)
In a patient with a reasonable expected lifespan, painful metastasis to the humerus that cannot be reconstructed or stabilized with a simpler, more functional reconstruction
Pathologic fracture through a primary malignant bone tumor of the humerus where adequate margins can still be achieved with total humeral resection
Solitary extensive metastasis to the humerus where the procedure would be done to theoretically provide the patient a longer survival (controversial)
Primary soft tissue sarcoma that extensively involves the upper arm/humerus but spares the neurovascular bundle
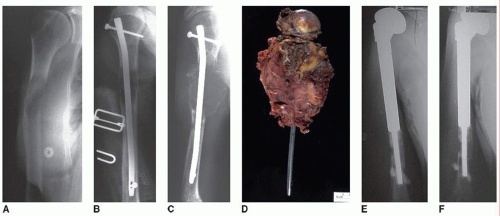
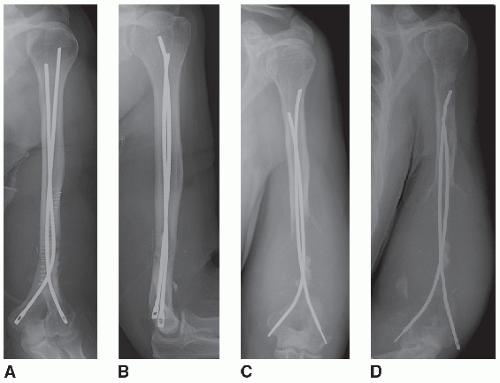
Failed prior stabilization (retrograde flexible nails, anterograde humeral nail) or reconstruction for oncologic/nononcologic reasons (proximal/distal humeral prosthesis, allograft or combination) (Fig. 32.2)
CONTRAINDICATIONS
Prior infected shoulder/humeral/elbow reconstruction (although in specific cases, an antibiotic spacer and intravenous antibiotics could be justified to clear an infection prior to reconstruction)
Primary sarcoma with widespread metastasis or metastatic carcinoma to the upper arm/humerus in a patient with a limited lifespan or extensive co-morbidities/operative risk (Fig. 32.3)
PREOPERATIVE PREPARATION
Patient Expectations
A total humeral resection and reconstruction is an extensive surgery often used to avoid a forequarter amputation. Although it is a limb salvage procedure, the patient should be aware of the potential complications (specifically infection and nerve injury) as well as the expected postoperative shoulder function. Generally, patients will have painless shoulder and elbow motion that allows completion of most basic activities of daily living. However, the shoulder function will be limited to an active range of motion of approximately 30 degrees of motion in any plane and decreased lifting ability.
Workup
A detailed history and physical examination are performed preoperatively with attention to pain, neurologic status, stage of tumor, expected lifespan, handedness, prior activity level, range of motion at the shoulder and elbow, use of the ipsilateral hand, presence of any signs/symptoms of infection, axillary lymphadenopathy, and presence of prior incisions/biopsy tracts. Plain radiographs of the humerus are obtained in two planes and include the shoulder and elbow. An MRI is necessary in patients with primary malignant bone tumors to assess the extent of disease in preparation for an adequate surgical margin. Specifically, the extent of tumor at the shoulder/elbow joints and amount of soft tissue extension in relation to the neurovascular structures are assessed. If tumor extends into the glenohumeral joint, an extra-articular resection may be required. Appropriate imaging of the chest, abdomen, and pelvis is performed to assess the stage of disease. Appropriate laboratory tests to include a complete blood count and electrolytes in patients on chemotherapy or who have medical comorbidities are indicated. If the patient has a highly vascular metastasis to the humerus (renal cell carcinoma, thyroid carcinoma), consideration should be given to preoperative embolization. If a large soft tissue defect is expected around the elbow or shoulder, a rotational or free flap might be necessary, so a preoperative plastic surgery consultation is prudent.
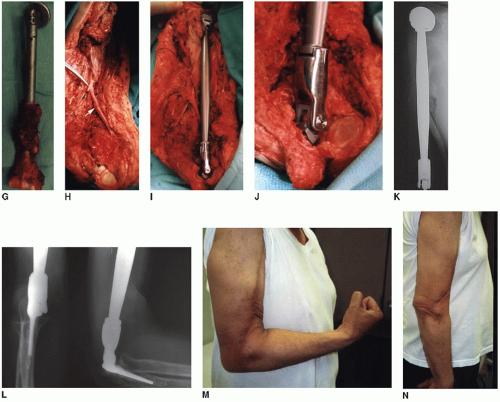
Equipment
A decision should be made as to the type of reconstruction to be used after humeral resection. If an allograft-prosthetic composite (APC) is to be used for the shoulder, an appropriate total humeral allograft should be appropriately sized and procured. The length of the allograft is important as well as a close match at the elbow joint. The proximal humerus is less critical for size matching than the distal humerus. The standard shoulder prosthesis to be placed in the proximal end of a total humeral allograft is templated. If a total humeral megaprosthesis is used, the elbow stems should be templated for the proximal ulna. If an extra-articular resection is performed at the shoulder, the standard prosthetic humeral head may not fit well against the scapular neck. Instead, a spacer can be used that is fitted to the top of the prosthetic humeral body segment and attached with heavy suture to the scapula and clavicle. Methylmethacrylate is used to fix the elbow prosthesis into the ulna. If an olecranon osteotomy is performed, wire fixation is necessary. A shoulder immobilizer or spica cast is used postoperatively.
Anesthesia Considerations
General anesthesia with or without a regional block is used during the procedure. It is important, however, that the neurologic status of the arm can be assessed postoperatively. The patient should have a viable type and screen/cross for blood products. Patients who receive preoperative chemotherapy may be anemic, and there is no tourniquet option during the case.
TECHNIQUE
Positioning
The patient should be positioned supine on the operative table to facilitate the anterior incision and dissection around the medial epicondyle and ulnar nerve. The entire upper extremity is prepared and draped up to the neck. The endotracheal tube should be positioned toward the opposite arm. A urinary catheter is placed if the procedure is anticipated to last more than 2 hours. Intravenous antibiotics are given and redosed throughout the procedure as appropriate.