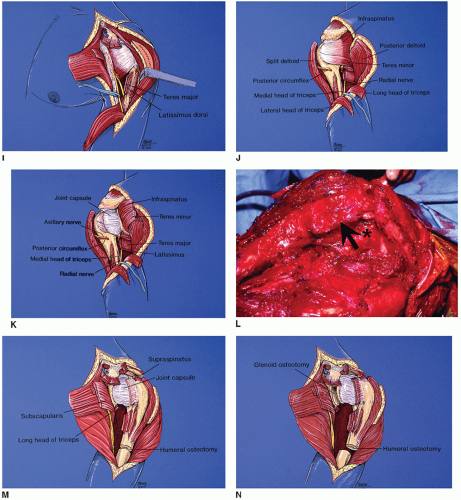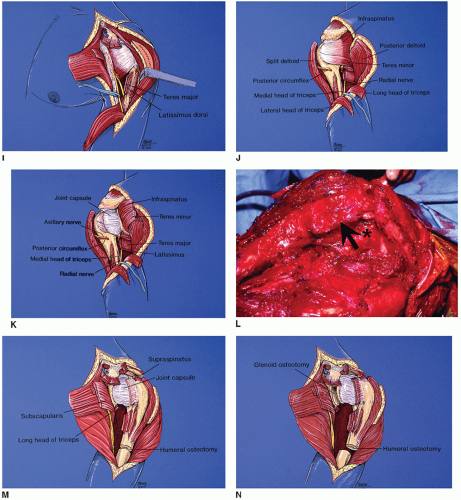
FIGURE 28.1 (Continued) I: The broad insertion of the latissimus dorsi is divided from the humerus and just posterior to this is the insertion of the teres major. The radial nerve is identified and protected. (Used Mayo Foundation for Medical Education and Research, with permission.) J: The posterior dissection begins with the deltoid released from the acromion and scapular spine and divided along the posterior aspect of the biopsy site, and the posterior aspect of the rotator cuff musculature is identified. The posterior humeral circumflex vessels are ligated, the axillary nerve is transected (if necessary), the long head of the triceps is released from the inferior glenoid, and the lateral head of the triceps is released from the proximal humerus. The posterior humeral circumflex vessels and axillary nerve are located in the quadrangular space formed by the teres minor (superior), long head of the triceps (medial), teres major (inferior), and lateral head of the triceps (lateral). (Used Mayo Foundation for Medical Education and Research, with permission.) K: The infraspinatus and teres minor are divided to expose the posterior capsule of the shoulder joint. (Used Mayo Foundation for Medical Education and Research, with permission.) L: Intraoperative photograph showing division of the infraspinatus and teres minor (arrow), with exposure of underlying posterior capsule (asterisk). M: Attention is directed again anteriorly, and the supraspinatus and supscapsularis are transected to expose the anterior and superior joint capsule. (Used Mayo Foundation for Medical Education and Research, with permission.) N: Drawing of the anterior aspect of the glenoid osteotomy medial to the joint capsule. (Used Mayo Foundation for Medical Education and Research, with permission.) |