Allograft Prosthetic Composites in the Pelvis
Peter F. M. Choong
Primary tumors of the pelvis account for almost 15% of all primary malignant bone tumors and present a considerable management challenge. Their location frequently involves the acetabulum and surgery to this part has significant implications for mobility and independence. Pelvic tumors often present late and may be quite substantial at the time of diagnosis, which adds to the difficulty of surgery and also has a negative influence on survival. The three most common sarcomas are chondrosarcoma, osteosarcoma, and Ewing sarcoma and the roles of adjuvant therapy in each case and their respective impacts differ widely. Surgery, however, is the mainstay of treatment and in the past, transpelvic or hindquarter amputation was traditionally performed for all resectable tumors. For the majority of these tumors, advances in the efficacy of chemotherapy have led to a profound improvement in survival and with greater sophistication of imaging modalities, the possibilities for limb-sparing surgery have increased. Indeed, the expectations of patients have now also increased in light of the increased success of limb-sparing surgery in general and pelvic surgery specifically.
Resections of the bony pelvis with oncologic margins almost always lead to large segmental defects in the pelvic ring with pelvic discontinuity. This is particularly important if resections include the acetabulum because the hip joint has a pivotal role in weight transmission, limb function, and mobility. In recognition of the importance of the acetabulum and the poor function that follows resection without periacetabular reconstruction, a wide variety of techniques has been developed to maintain the function of the hip joint and these include biologic reconstructions with allograft or autograft bone, prosthetic reconstructions including pelvic and saddle prostheses, and combinations of biologic and prosthetic reconstructions such as allograft prosthetic composites.
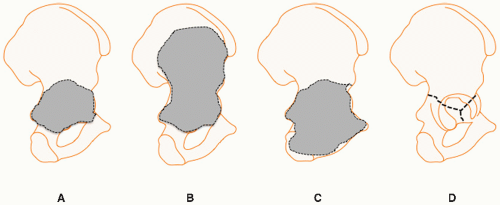
Allograft reconstructions have a number of advantages, including a readily available source, the ability to be size matched, a shape that can be customized to fit the defect created by tumor resection, biologic union with host bone, which may arguably provide better stability than the fixation of a prosthetic pelvic device, and reestablishment of acetabular anatomy, which in turn allows hip arthroplasty with conventional joint prostheses. The acetabular defect may be segmental or total and may include part of the ilium, ischium, or pubis (Fig. 3.1).
INDICATIONS
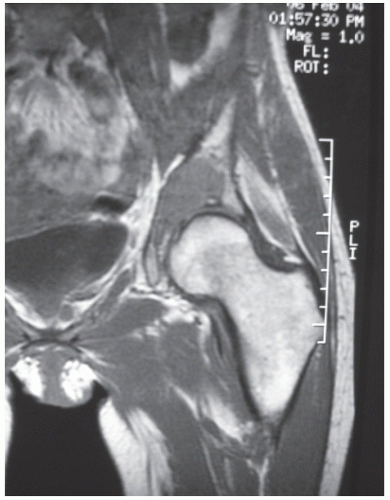
Wide resection with allograft pelvic reconstruction and prosthetic joint replacement is indicated when a primary tumor involves the periacetabulum (Fig. 3.2). Extension of the tumor into the hip joint should not prevent this type of reconstruction.
The extent of encroachment into the ilium or pubic rami should raise concerns if this spread is large because the quality of support provided to the allograft and fixation to ilium and pubic rami gets poorer the further away from the periacetabulum the osteotomy is made.
CONTRAINDICATIONS
Patients undergoing chemotherapy are at high risk of developing secondary infections from their immunosuppression and neutropenia. The use of large segmental allografts during a prolonged surgical procedure also brings with it its own risk of infection. Performing allograft surgery in the presence of pre-existing sepsis in immunocompromised patients raises the certainty of infection to unacceptable levels and pre-existing sepsis should be regarded as an absolute contraindication to allograft transplantation.
True solitary metatases are rare. Often they represent the first presentation of what is usually widespread disease. Therefore, the role of wide resection and allograft reconstruction for a putative solitary metastasis may be questionable. If systemic metastasis is evident, the risk of surgery may outweigh the benefits in a patient with only a limited survival chance.
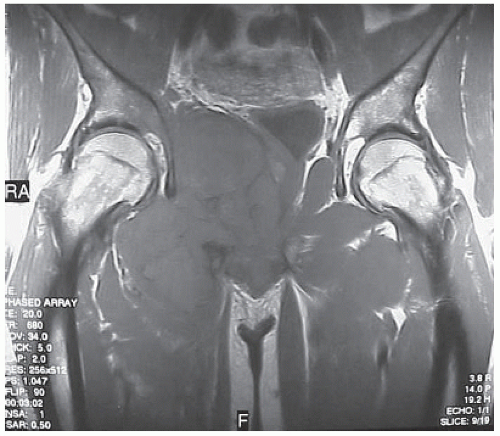
Some tumors are associated with a large soft tissue component (Fig. 3.3). This may render safe dissection around the major neurovascular structures or viscera impossible without violation of the tumor boundaries and contamination of these structures. In this scenario, hindquarter amputation may be a safer option than
limb-sparing surgery. If periacetabular resection is also associated with sciatic or femoral nerve sacrifice, not only does the patient face a dysfunctional lower limb but the stability of the reconstructed hip joint may also be jeopardized. In this scenario, limb-sparing surgery is contraindicated.
If tumor resection requires sacrifice of the whole hemipelvis, only the sacrum will be left to provide a wide surface against which to seat a pelvic allograft. Attempts at achieving union with the contralateral pubis have been disappointing and with only the sacrum and the contralateral pubis for attachment, the allograft pelvis is left unsupported over a wide expanse. This predisposes the allograft to fracture and early failure.
Major pelvic resections and management of subsequent complications require a team approach for successful completion. Skilled surgical staff, intensive care facilities, an experienced anesthetic team, ready access to a blood bank, and excellent ward facilities are mandatory when undertaking major pelvic resections and reconstructions. Absence of any elements of the above will require careful consideration prior to embarking on such complex surgery.
PREOPERATIVE PREPARATION
Staging Investigations
Staging investigations should be performed at the time of diagnosis as part of the patient workup and after neoadjuvant chemo- or radiotherapy to assess the response to treatment immediately prior to surgery. The surgical margins are calculated based upon the imaging performed immediately before surgery except in cases where there has been a poor response to neoadjuvant treatment. In the latter situation, surgical margins should be based on the studies obtained at the time of initial diagnosis.
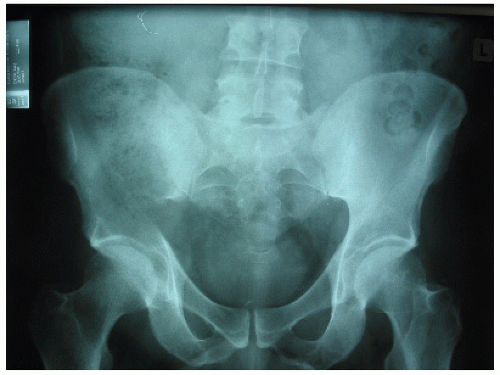
Plain Radiographs
Plain radiographs should be obtained to allow rough planning and sizing of allograft material (Fig. 3.4). Further, it is important to preoperatively create a template of prostheses and preselect of a range of pelvic reconstruction plates that will be required to span and support the graft.
Bone Scan
Technetium methyl-diphosphonate bone scans should be obtained to identify the presence of any osseous metastases.
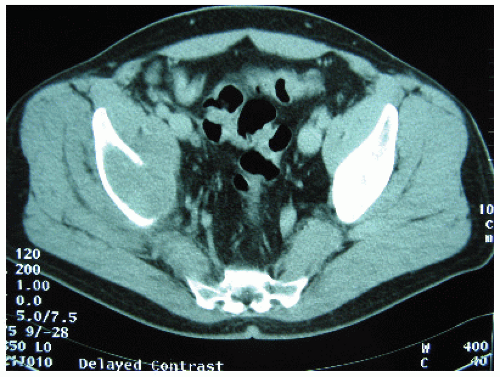
Computed Tomography
Computed tomography (CT) of the lungs is mandatory prior to surgery. Evidence of pulmonary metastases is a contraindication to major pelvic resection or reconstruction. CT is an excellent modality for delineating cortical or trabecular destruction (Fig. 3.5). Further, periosteal new bone formation is best detected using this modality and this will be critical in planning margins. The availability of three-dimensional reconstructed images may assist in planning the type and shape of allograft reconstruction to be employed.
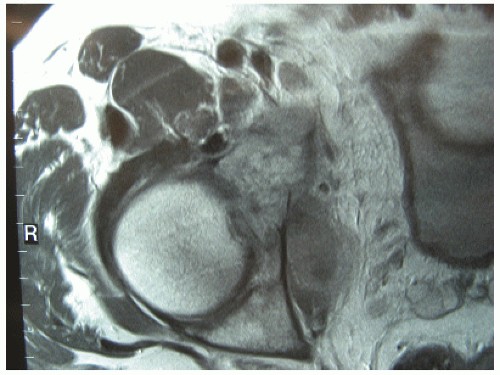
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) provides unsurpassed soft tissue contrast and this characteristic should be exploited when deciding upon the appropriate soft tissue margins. This is particularly relevant when the soft tissue component of tumors lie adjacent to major neurovascular structures such as the lumbosacral trunk, the internal iliac vessels, the sciatic nerve, and gluteal vessels in the greater sciatic notch. Involvement of the hip joint may also be suspected by the presence of a joint effusion or changes in the signal characteristics of the hip joint fat pad or ligamentum teres. MRI is also an excellent modality for assessing the intraosseous extension of tumor which has implications for the planning of surgical margins (Fig. 3.6).
Functional Nuclear Imaging
Positron emission tomography and thallium scanning are two nuclear medical techniques that reflect the metabolic activity of tumors. They are ideal for assessing the most metabolically active part of the tumor for targeted biopsy as well as for assessing the response of tumors to neoadjuvant therapy. Poorly responsive tumors should be excised with far wider margins than those that are applied for good responding tumors.
Blood Cross-Matching
Pelvic resections may be associated with considerable blood loss and this should be anticipated prior to the commencement of surgery. Cross-matching of blood should be performed early to identify the presence of any particular antibodies in the recipient that may make high-volume transfusion during surgery hazardous. Initial blood cross-matching demands should include 15 units of packed cells, 10 units of fresh frozen plasma, and 10 units of platelets. Further blood requirements may be determined on intraoperative testing of the patient’s hemoglobin.
Preoperative Optimisation
Most patients on chemotherapy will experience a fall in peripheral blood products as a consequence of marrow suppression. The level of suppression is dependent on the health status of the patient, the type of cytotoxic drugs employed, and their dose and intensity of delivery. Advice should be sought from the treating chemotherapists as to what would constitute a safe minimum level of red cells, neutrophils, and platelets for surgery to be undertaken. In some circumstances, GM-CSF may be used to stimulate bone marrow activity. It is important to ensure that the patient has good renal function prior to surgery. The extensive blood loss and potential for intraoperative hypotension in the setting of preoperative chemotherapy may lead to renal failure. Some chemotherapeutic agents, for example doxorubicin, may also have a cardiotoxic effect. It is important that the state of the cardiac function is established prior to surgery so that appropriate intraoperative monitoring and care may be provided by the anesthetic team. Close collaboration with internal medicine physicians is required to optimize the preparation of the patient for surgery.
Informed Consent
It is critical that patients and their carers understand the full extent and sequelae of surgery. Information about the material risk must be furnished to patients to guide their acceptance or refusal of the complications and hardship of a failed reconstruction. If patients have understood the real risk of complications they may elect to accept hindquarter amputation or a flail hip in place of allograft reconstruction. Further, they need to understand the need for prolonged recumbency or rehabilitation to ensure safe healing and return of function to the operated limb. Finally, patients also need to understand the impact that surgery and the subsequent prolonged recovery phase will have on the quality of their lives over the ensuring 1 to 2 years. This is important because the risk of local or systemic recurrence of disease within the first 2 years is great and the patients will need to balance what limited time they may have after surgery with the incursion that postoperative convalescence and complications may have on that time.
TECHNIQUE
Patient Position and Draping
The patient is placed in a “floppy” lateral position with loosely applied supports resting against the thoracic spine and sternum. This allows the patient to be flopped forward to provide better visualization of the back of the pelvis or flopped backward to allow better visualization of the front of the pelvis. An axillary support is used to elevate the contralateral chest wall off the downside arm to avoid prolonged axillary and brachial neurovascular compression. The ipsilateral arm is excluded from the operative field under the drapes but is supported by a thoracic armrest to allow it to move with the body when the body is rolled from side to side as well as to reduce the weight of the arm against the chest wall that may cause axillary and brachial neurovascular compression. A protective plastic drape may be applied to shut out the upper body and the contralateral limb, ensuring that the margins of this drape cover the genital and perineal areas to avoid pooling of caustic or alcoholic antiseptic wash that may collect on the operating table or in skin creases and cause chemical skin burns or intraoperative fires sparked by electrocautery. The abdomen is draped free to allow access to the entire abdominal field. The ipsilateral limb is draped free to allow manipulation during surgery and preparation of the proximal femur for joint replacement. Access to the pubic symphysis is important to determine the correct position of the anterior pelvic osteotomy and also to protect the bladder and the bladder neck. Padding under pressure points such as the downside ankle, knee, and trochanter is important to avoid pressure necrosis of skin.
Anesthetic Considerations
Central venous and arterial access is vital for monitoring blood volume and pressure intraoperatively. The former also provides a reliable access for fluid resuscitation and drug delivery. Other intravenous lines are also inserted according to anesthetic preference. All patients are usually subjected to endotracheal intubation and volatile agent anesthesia and then ventilated during surgery. In some institutions, regional anesthesia is
combined with general anesthesia. This achieves two purposes, namely, a reduction in the depth of general anesthesia during surgery because of the presence of regional anesthesia and the ability to continue regional anesthesia postoperatively, which may help to reduce the requirement of intravenous narcotic analgesia.
combined with general anesthesia. This achieves two purposes, namely, a reduction in the depth of general anesthesia during surgery because of the presence of regional anesthesia and the ability to continue regional anesthesia postoperatively, which may help to reduce the requirement of intravenous narcotic analgesia.
Urinary Catheterization
In the case of large pelvic tumors, the decision may be made to insert ureteric catheters prior to the commencement of surgery to assist in the identification of these structures during dissection. These are usually placed endoscopically and secured to a bladder catheter which is inserted at the same time for intra- and postoperative urine volume measurements.
Prophylactic Antibiotic
The risk of infection is high because of the immunosuppression, prolonged surgery, extensive soft tissue trauma, and the implantation of foreign biologic and synthetic material. Combination antibiotic therapy to cover staphylococcal and Gram-negative organisms is recommended. Vancomycin and ceftriaxone in combination provide adequate coverage and may be continued safely postoperatively. These should be given preoperatively and allowed to circulate prior to the commencement of surgery. Vancomycin should be given slowly over 30 minutes to avoid a vascular reaction sometimes referred to as “red man” syndrome.
Incision
A curved iliofemoral incision begins at the posterior superior iliac spine and follows the course of the iliac crest to the anterior superior iliac spine. It then passes distally a few inches in front of the greater trochanter before sweeping slightly distally and posteriorly a hand span distal to the center of the greater trochanter (Fig. 3.7A). The skin incision is carried down to and through the deep fascia. This creates a posteriorly based gluteal flap. Tumors that are covered by the gluteus medius muscle spare the gluteus maximus muscle which carries the blood supply to the overlying skin through the inferior gluteal vessels. If required, a second incision can be created that passes from the anterior superior iliac spine forward to the pubic tubercle (Fig. 3.7B). Should a second
incision be required, a triradiate incision is created, which gives an extensile approach to the hemipelvis. The anterior limb of the triradiate incision is created to provide better access to the vital neurovascular structures as they cross the inguinal ligament. A disadvantage of the triradiate incision is the potential for skin ischemia at the junction of the three limbs of the skin incision.
incision be required, a triradiate incision is created, which gives an extensile approach to the hemipelvis. The anterior limb of the triradiate incision is created to provide better access to the vital neurovascular structures as they cross the inguinal ligament. A disadvantage of the triradiate incision is the potential for skin ischemia at the junction of the three limbs of the skin incision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree