Megaprosthesis for Non-Neoplastic Conditions of the Proximal Femur
Javad Parvizi
S. M. Javad Mortazavi
Tim van de Leur
Panayiotis J. Papagelopoulos
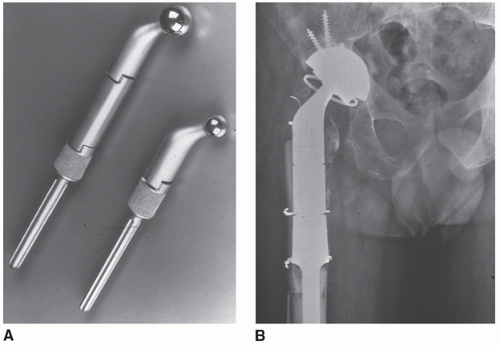
With the rise in the number, and to some extent the complexity, of revision hip surgery, continuous challenges need to be met. One of these challenges is the reconstruction of femur with extensive bone loss. Although a number of options exist, there are some patients in whom the best option is replacement of the proximal femur with a so-called megaprosthesis. Megaprosthesis has been available in the armamentarium of orthopedic surgeons for a few decades. The problems with the earlier generation of megaprosthesis were twofold. First, these prostheses did not provide flexibility for restoration of limb length and soft tissue tension. The second problem is related to the proximal surface of these prostheses that did not allow reattachment of soft tissues or ongrowth of bone. In recent years, modular megaprostheses (Fig. 10.1A) have been introduced that intended to address the shortcomings of the first-generation megaprosthesis. The modularity has allowed reconstructive surgeons to more accurately restore limb length, soft tissue tension, and subsequently reduce the incidence of instability that was seen with the older megaprostheses. In addition, the introduction of constrained cups (Fig. 10.1B) has been very effective in reducing dislocation following the use of megaprosthesis.
INDICATIONS
Due to concomitant advances in alternative reconstruction methods and increased use of cortical strut grafts to augment host bone, the indications for the use of the megaprosthesis have narrowed. Recent evidence, however, does point to the fact that in select cases with severely compromised bone stock where the use of a conventional prosthesis is precluded, proximal femoral replacement is a viable choice for reconstruction (7).
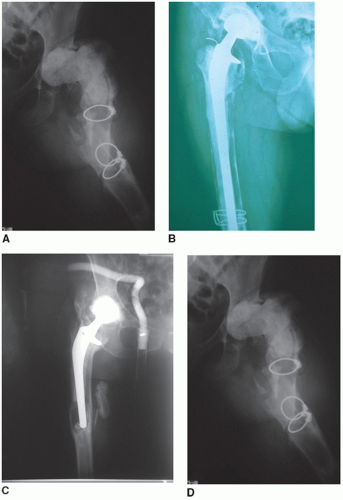
The indications for megaprosthetic use include older patients with extensive femoral bone loss that may have occurred as a result of
Infection (Fig. 10.2A)
Osteolysis (Fig. 10.2B)
Periprosthetic fracture (Fig. 10.2C)
Multiple previous surgeries (Fig. 10.2D)
Nonunion of proximal femur despite multiple attempts for osteosynthesis
Reconstruction of femur following resection arthroplasty
In younger and more active patients, reconstruction of deficient proximal femur may be attempted by an allograft prosthetic composite (See Chapter 12). An important and critical prerequisite for the use of
proximal femoral replacement is that there is sufficient distal femoral length (>10 cm available for secure fixation of the prosthesis). When distal bone is inadequate, consideration for total femoral replacement must be given.
proximal femoral replacement is that there is sufficient distal femoral length (>10 cm available for secure fixation of the prosthesis). When distal bone is inadequate, consideration for total femoral replacement must be given.
CONTRAINDICATIONS
The presence of superficial or deep infection around the hip
Uncooperative patient
Vascular insufficiency of the limb
Malnutrition
Skin disorders with active lesions or ulcers
Significant medical comorbidities precluding administration of anesthesia
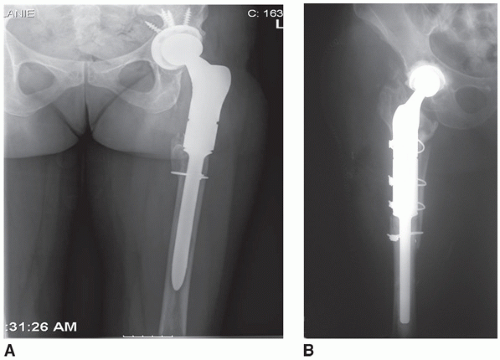
PREOPERATIVE PLANNING
Preoperative planning is an important aspect of hip reconstruction particularly during revision surgery. Patients requiring proximal femoral replacement have often had numerous previous surgeries making preoperative evaluation and templating critical. The purpose of the preoperative templating is mainly to determine (a) if sufficient length of distal femur is available to allow fixation of the proximal femoral replacement and (b) the approximate length of the prosthesis that will be needed. The templating also allows the surgeon to determine the site of transverse osteotomy and the diameter of distal femur. During templating, the quality of the distal bone is also assessed and decision is made regarding the use of cemented versus uncemented prosthesis (Fig. 10.3). For cementless fixation, adequate bone stock must be present to allow either creation of a 4-to 5-cm tube of bone of a specific diameter into which a porous stem may obtain a scratch fit or a tapered geometry into which a tapered, splinted stem may be placed for axial and rotational loading. If the remaining bone stock is deemed inadequate because of osteopenia or extremely patulous and capacious, cemented fixation should be used.
Most patients undergoing megaprosthesis reconstruction have had multiple previous hip procedures. Therefore, it is imperative to examine the incision site carefully for the presence of skin lesions that may predispose or increase the rate of infection and to determine the appropriate previous scar to be utilized. A new incision may occasionally have to be used if the previous scars are inappropriately placed. On occasion, involvement of plastic surgeons may be necessary to evaluate the status of the soft tissues in case local or free flaps may be required for reconstruction.
Thorough examination of the hip with particular attention to the status of the abductors and the limb length should also be carried out preoperatively. Clinical and radiographic (standing films) assessment of the limb length is carried out and recorded. Patients should be counseled about the possibility of limb length discrepancy that may result from surgery. In our opinion, lengthening of the limb up to 4 cm can be carried out safely. Any lengthening beyond this point is likely to place the neurovascular structures at increased risk. Intraoperative monitoring of the sciatic and femoral nerves should be performed in patients in whom extensive (>4 cm) limb lengthening is anticipated.
It is paramount to rule out infection. We always order a white blood cell count with differential, C-reactive protein, and erythrocyte sedimentation rate for this purpose. Based on clinical and radiographic examinations and the result of serology, hips with a high index of suspicion are also preoperatively aspirated to rule out deep infection. At the time of surgery, multiple (usually odd numbers) tissue samples should be sent for culture.
All patients should receive a thorough medical examination with appropriate laboratory investigations to ensure their fitness for surgery. Revision hip arthroplasty with megaprosthesis involves extensive soft tissue dissection and unusually long operative times; moreover, large volumes of blood loss place immense physiological demand on the patient.
Preoperative templating to select the appropriate stem length and diameter is essential for operative success. Problems with the removal of existing hardware, specific needs for acetabular reconstruction, and the potential need for insertion of constrained liners should be anticipated and addressed appropriately. Despite the most accurate preoperative measurements, a variety of prosthetic sizes should be available in the operating room as intraoperative adjustments often lead to changes in the anticipated size of prosthesis. The megaprosthesis manufacturing company representative should be contacted and be present in the operating room for assistance. Experienced operating room personnel, particularly the scrub person, should be available and assist with this procedure. An experienced anesthesia team should administer anesthesia as invasive monitoring in these, often elderly and frail, patients is warranted.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree