Pelvic Prosthesis
Martin Dominkus
Rainer Kotz
Surgical reconstruction after pelvic resections remains a highly demanding procedure. More efficient chemotherapy in primary malignant bone tumors and a high percentage of long-term survivors have inspired greater interest in the development of pelvic reconstruction methods that permit limb salvage resections. The reconstructive procedures that are associated with pelvic reconstructions may be biological, endoprosthetic, or a combination of the two, and include pelvic allograft, saddle prosthesis, allograft prosthetic composites, and pelvic prosthesis reconstructions. This chapter gives an overview of the history, development, and state of the art of pelvic reconstruction with pelvic prostheses.
PREOPERATIVE PLANNING
Independent of the reconstruction method, accurate preoperative imaging of the intraosseous and extraosseous tumor extent is obligatory. This includes
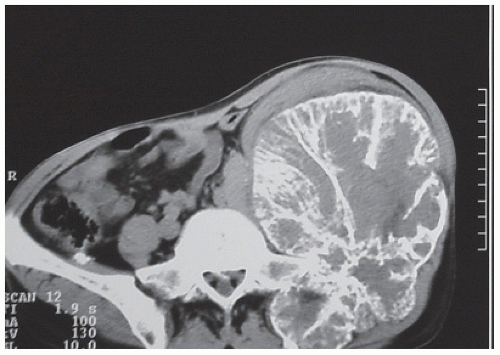
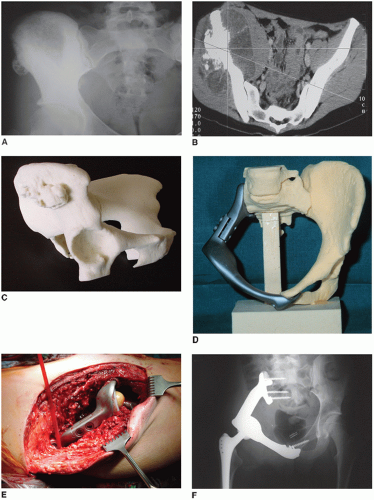
Computerised tomography (CT) scans, which provide the best information for detection of cortical lesions and offer the basic data for three-dimensional (3D) reconstruction (Fig. 4.1).
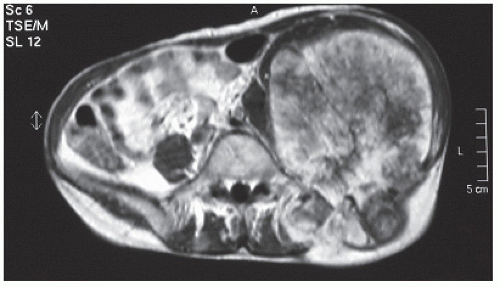
MRI scans, which is ideal for demonstrating the intraosseous tumor extent, soft tissue involvement, and joint involvement (Fig. 4.2).
Intravenous pyelography, which highlights the anatomical position of the ureter. Preoperative insertion of a ureteric catheter may prevent intraoperative damage.
Arteriography or venography, which demonstrates the position and potential involvement of the iliac or femoral vessels. Recent generation MR angiographic techniques permit noninvasive assessment of the arterio and venous systems.
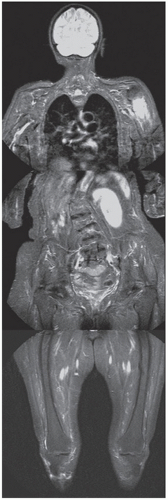
Scintigraphy or whole body magnetic resonance imaging (MRI), which can diagnose or exclude metastatic disease (Fig. 4.3).
The insertion of a vena cava filter, which can prevent fatal intraoperative or postoperative thromboembolism.
PREOPERATIVE CONSIDERATIONS
The patient should be in a good health condition with normal blood values before the operation. Sufficient amounts of blood products (packed cells, platelets, fresh frozen plasma) should be crossmatched and available, and a rapid blood warming-transfusion system should be available.
OPERATIVE CONSIDERATIONS
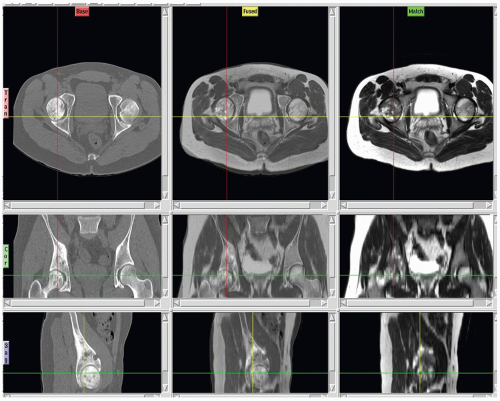
Newer computerized techniques that employ coregistration of CT and MRI images facilitate intraoperative computer navigation techniques for tumor resection and exact planning of the bone resection lines (Fig. 4.4).
Depending on the type of endoprosthetic reconstruction additional preoperative planning has to be done. Most of the custom-made prostheses are designed via a 3D pelvic model, produced from the original CT data (Fig. 4.5A-F).
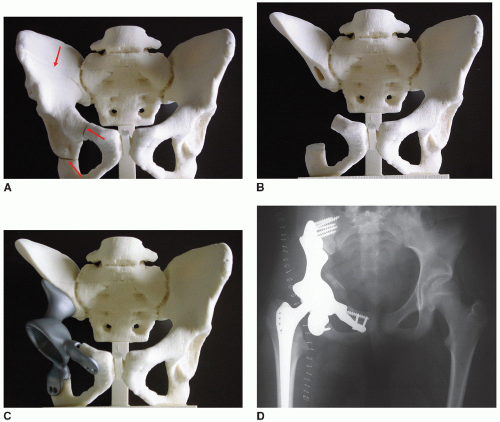
More recently a virtual reality planning and simulation of endoprosthetic reconstruction of the pelvis has been reported (1). Using this technique, three-dimensional models are generated and manipulated in real time during the simulation of the pelvic operation. Cutting planes can be positioned in the 3D scene. The resected bone model is then used to determine the shape and geometry of the endoprosthesis. This technique prevents the time-consuming step of production of a solid pelvic model but the preoperative modeling of the prosthesis’s size and position is critical for planning the intraoperative bone resection (Fig. 4.6A-D). An example of preoperative 3D visualization and determination of the bone resection, followed by computer aided design (CAD) designing and production of the prosthesis from the preoperative dataset and the exact intraoperative navigation of the appropriate bone resection, reporting a case of a patient with a metastatic destruction of the left acetabulum from a rectal carcinoma, was reported (2).
DISCUSSION
The first attempts of endoprostheses to reconstruct resected pelvic bone and to restore the pelvic ring can be found in the early 1970s. Scales and Rodney (personal communication) implanted a temporary spacer of acrylic cement and designed a steel prosthesis in the shape of the resected iliac bone. In a second surgery, they implanted the prosthesis by fixation with pins and cement. Unfortunately, the prosthesis had to be removed a few months later due to infection.
In 1974, Schöllner and Ruck (3) published the first case, in which resection of a chondrosarcoma in a 53-year-old truck driver was followed by implantation of a pelvic prosthesis during the same surgery. The extent of the planned resection was determined from x-rays of the patient. Next, a cast model was produced
from a pelvic skeleton, which was similar in size to that of the patient. On this pelvic model, the resection lines were determined and a custom-made pelvic prosthesis was machined from steel. The tumor was removed by a Type II wide resection (4) and the prosthesis was implanted in the same procedure. The prosthesis was fixed to the remaining part of the ilium, ischium, and pubic bone by flanges and screws. The femoral part of the hip joint was reconstructed with a conventional Charnley-Mueller prosthesis. Five weeks after surgery the patient left the hospital, mobilized with partial weight-bearing, and at follow-up examination, the prosthesis was still in place without any signs of dislocation, loosening or infection, and the patient was able to walk with one cane and drive his car.
from a pelvic skeleton, which was similar in size to that of the patient. On this pelvic model, the resection lines were determined and a custom-made pelvic prosthesis was machined from steel. The tumor was removed by a Type II wide resection (4) and the prosthesis was implanted in the same procedure. The prosthesis was fixed to the remaining part of the ilium, ischium, and pubic bone by flanges and screws. The femoral part of the hip joint was reconstructed with a conventional Charnley-Mueller prosthesis. Five weeks after surgery the patient left the hospital, mobilized with partial weight-bearing, and at follow-up examination, the prosthesis was still in place without any signs of dislocation, loosening or infection, and the patient was able to walk with one cane and drive his car.
Johnson treated two patients after internal periacetabular resection with a reconstruction of the pelvic ring by cement reinforced Küntscher rods and Kirschner wires (5). One patient, who had adequate resection of a chondrosarcoma, was reported to be well and able to walk without a cane 5 years postoperatively, and the other patient, who had an inadequate resection of a high-grade chondrosarcoma, died after 2 years but was also able to walk with a cane.
Since that time attempts have been made to improve the accuracy of pelvic prosthesis production and design. Better imaging techniques now allow precise preoperative planning and 3D CT data help to obtain an exact model of the patients’ pelvis.
Gradinger reported on 25 patients with internal hemipelvectomy and endoprosthetic reconstruction for primary bone tumors in 17 and metastases in 8 patients. Also in his series the first prostheses were custom-manufactured from plain x-rays. Intraoperatively, they were difficult to adopt and the anatomical orientation of the acetabulum was imprecise. Prostheses made from polyacetal could be adopted intraoperatively more easily, but still the orientation was insufficient. Since the use of CT and the possibility of computer-aided design of pelvic models, Gradinger developed a new custom-made, anatomically adoptable prosthesis. The anchorage into the remaining iliac bone was mainly provided by an intramedullary stem with additional plates and flanges with screw holes to also enable screw fixation. To reduce lateral shear forces, the pelvic ring was closed with a semidynamic connection mimicking the symphysis function. Twenty of these prostheses were used in his series and he reported a reduction of complications, for example, dislocation, reduction in operation time, and infection (6).
In a review of our own series, Windhager et al. reported on 21 consecutive cases who underwent limb salvaging surgery for periacetabular sarcomas between 1972 and 1990. In cases with preoperative conventional imaging techniques only 50% of the resection could achieve wide margins, whereas 100% wide margins were documented after 3D imaging. In nine of these patients, a custom-made endoprostheses (Howmedica) was used after defining the resection on a real-size model produced using computer-assisted reconstruction of CT sections. The functional outcome was best after reconstruction with a custom-made prosthesis, only satisfactory after saddle prosthesis and poor, when allografts or when no reconstruction was performed (7). A new ventral and dorsal approach was used in most of the patients, which offered the advantage of good exposition of the ischium and the lateral part of the sacrum.