, George C. Babis2 and Kalliopi Lampropoulou-Adamidou3
(1)
Orthopaedic Department Medical School, National and Kapodistrian University, Athens, Greece
(2)
2nd Orthopaedic Department Medical School, National and Kapodistrian University Nea Ionia General Hospital “Konstantopoulion”, Athens, Greece
(3)
3rd Orthopaedic Department, National and Kapodistrian University KAT General Hospital, Athens, Greece
Abstract
In our days the majority of patients with advanced osteoarthritis secondary to congenital hip disease are treated with total hip replacement. However, this operation must be reserved for selected patients and performed by experienced surgeons familiar with this type of procedure. In this chapter, the indications of total hip replacement and the value of preoperative assessment are presented. The surgeon should be preoperatively informed of the type of the deformity in order to be prepared for the method, instruments and implants that will be used.
The introduction of total hip replacement (THR) by the pioneers in the field, John Charnley [1] and McKee Farrar [2], radically changed the treatment of congenital hip disease (CHD) in adult patients. The older methods, such as of osteotomies and excision arthroplasties, were gradually abandoned in favour of the new revolutionary method of THR. During the first years, a scepticism existed and even Charnley [3] stated that THR, in some technically difficult cases of high dislocation, should be avoided. However, in the next years, new techniques and implants made THR feasible even in these extreme cases. The last 20–25 years the literature is full of articles reflecting the worldwide experience on the field (see Chap. 8).
THR became an exceptionally significant procedure for the treatment of CHD in adults (Figs. 8.2 and 8.3). However, it may involve unexpected disappointment (Figs. 10.9, 10.10, 10.11 and 10.12). Therefore, it is imperative to be decided when it is absolutely necessary. Orthopaedic surgeons should protect this operation from the overuse. The patients should be informed for the severity of the procedure, for potential complications and that their new artificial joint is a subject of physical wear.
The term “total hip replacement (THR)” than “total hip arthroplasty (THA)” must be used. This term is more accurate because it reminds that this is an irreversible procedure in which the destroyed joint is removed and replaced by an artificial one. “Arthroplasty”, a compound Greek word, has the meaning of joint anaplasis/formation and may be misleading for both the surgeon and the patient.
6.1 Indications
Due to surgical difficulties and serious complications of THR in patients with CHD, the operation should be reserved for very selected patients who realise the increased risks and the possibility of failure [4]. Obviously, an experienced surgeon familiar with these hips must perform THR in dislocated hips, and only when there is a clear indication [4]. The simple fact that new methods and prostheses have developed and, also, that our surgical experience has increased are no reasons for early intervention (Fig. 6.1).
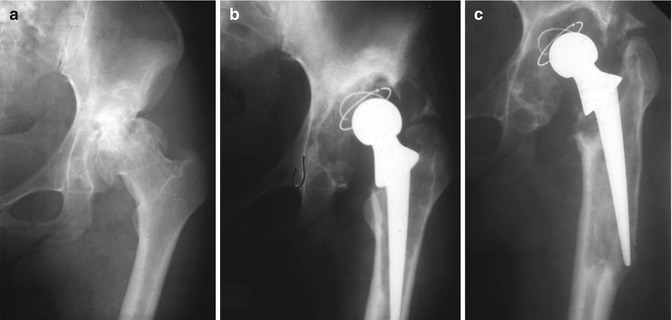
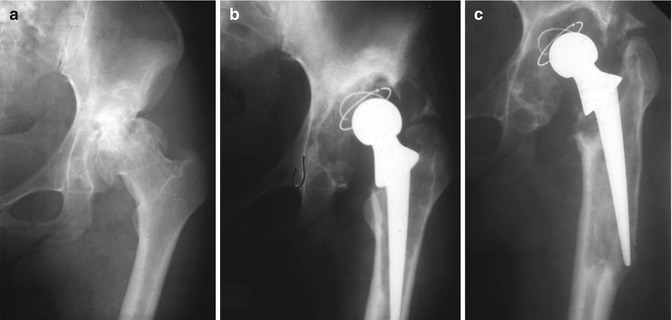
Fig. 6.1
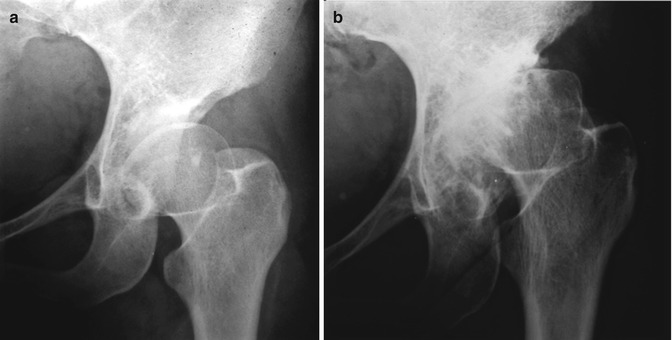
(a) This patient with a dysplastic left hip, at the age of 33, had only mild limp without pain. She was operated without clear indications. (b) Radiograph one year postoperatively. The cup was not inserted in the right place as the surgeon did not notice in the preoperative radiograph that the femoral head was articulated with a false acetabulum and the stem was fixed in varus and penetrated the lateral cortex. (c) The hip was revised 7 years later, after incomplete follow-up that resulted in major bone stock loss
Pain and/or severe functional impairment with severe limping, before pelvic inclination , fixed flexion deformity of the hip and knee and spinal deformities have been established are the main indications for surgery. Mild limping alone is not an indication, especially in young active patients. These patients should be encouraged to avoid extreme daily activities and occasionally use anti-inflammatory drugs and follow a programme of adapted physiotherapy (Figs. 6.2 and 6.3) [5].