, George C. Babis2 and Kalliopi Lampropoulou-Adamidou3
(1)
Orthopaedic Department Medical School, National and Kapodistrian University, Athens, Greece
(2)
2nd Orthopaedic Department Medical School, National and Kapodistrian University Nea Ionia General Hospital “Konstantopoulion”, Athens, Greece
(3)
3rd Orthopaedic Department, National and Kapodistrian University KAT General Hospital, Athens, Greece
Abstract
Basic principles for better results of total hip replacement in patients with congenital hip disease, especially those with low and high dislocations, are wide exposure, restoration of the normal centre of rotation and the use of special techniques and implants for the reconstruction of the acetabulum and femur. In this chapter, the authors’ experience in conjunction with the international experience on the subject is presented.
Total hip replacement (THR) in patients with congenital hip disease (CHD), especially in cases with low and high dislocation, is difficult and may hide unexpected complications . The major technical difficulties , encountered during surgery, are reconstruction of the deficient acetabulum and implantation of the femoral component in cases with deformed upper femur and narrow and stovepipe-shaped diaphysis . Difficulties are even more increased in cases with angular deformities of the femur from previous osteotomies [1] (Fig. 3.4).
Basic principles for a successful uncomplicated THR in patients with CHD are:
A wide exposure
The restoration of the normal centre of rotation
The use of special techniques and implants
7.1 Wide Exposure
A wide exposure is essential and is better achieved by the lateral transtrochanteric approach (TTA) (Fig. 7.1). The TTA was introduced by Charnley [2], who suggested that it would not only facilitate access to the joint but might also restore normal biomechanics by advancing the greater trochanter distally and laterally, thereby creating a more powerful abductor mechanism , by increasing the abductor lever arm , and minimises the reaction forces acting on the acetabulum [3, 4].
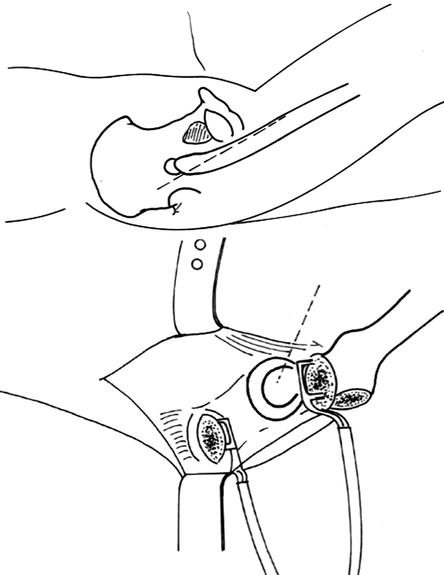
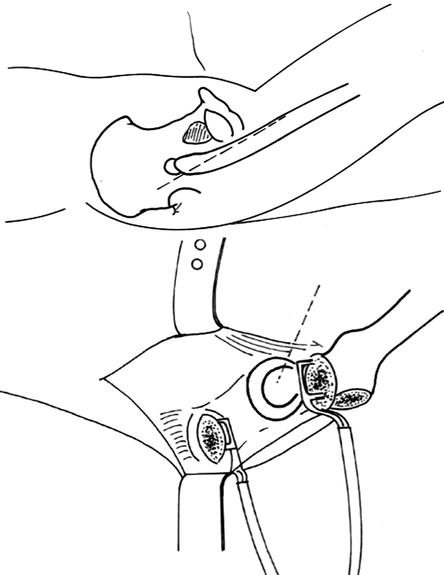
Fig. 7.1
For a wide exposure, an extended incision and trochanteric osteotomy are necessary
Charnley initially recommended the TTA for all THRs [2]. He believed that the problems arising from restricted exposure during surgery might lead to complications more serious than those occurring from the osteotomy itself (Fig. 7.2). He insisted that all orthopaedic surgeons should learn this approach, which would be needed in difficult hips and for revision operations. Although the majority of surgeons today prefer to use other approaches in routine primary cases, this method remains safe and effective in certain instances, including CHD, revision surgery, stiff hips, protrusio acetabuli and cases with severe osteoporosis [4].
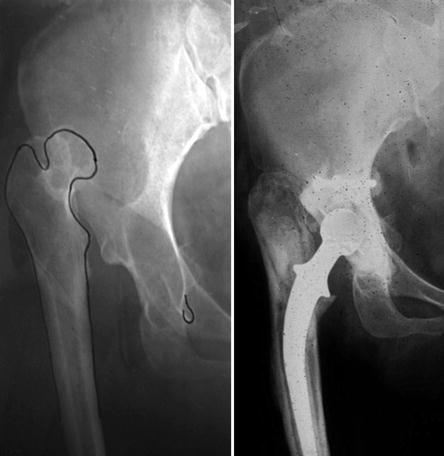
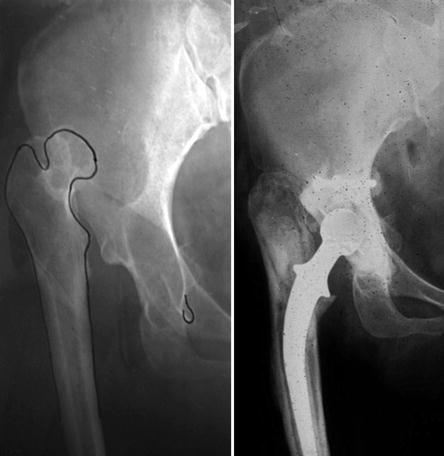
Fig. 7.2
The surgeon of this patient decided not to osteotomise the greater trochanter. The result was a postoperative palsy of both femoral and peroneal nerve and an early loosening of the components within 2 years
Reattachment of the osteotomised greater trochanter is not always easy. This is due to shortened abductors, an often small and malpositioned trochanter and a lengthened limb. Four categories of the position of reattachment of the trochanter in relation to its original bed were recognised (Fig. 7.3): (a) reattachment at the original bed of trochanteric osteotomy ; (b) distal reattachment in relation to its original bed, the trochanter having contact with the distal part of the original bed; (c) reattachment on the lateral femoral cortex in cases where the femoral neck was resected to the level of the distal part of the lesser trochanter and (d) reattachment proximal to its original bed [5].
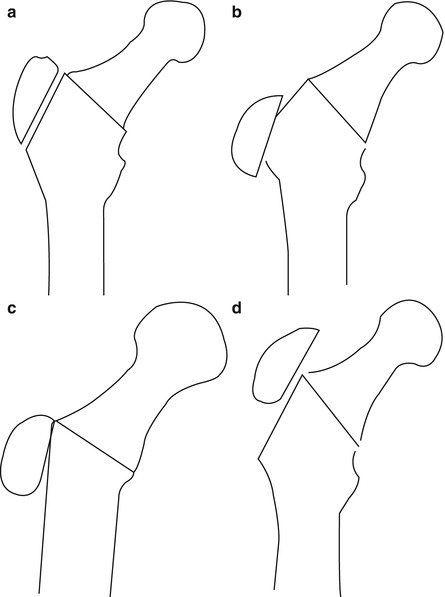
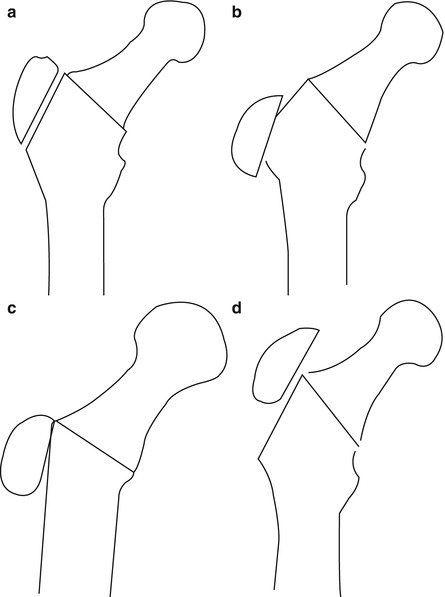
Fig. 7.3
Diagram showing the position of different sites of reattachment of the trochanter: (a) at its original bed; (b) distal reattachment, the trochanter retaining contact with the distal part of the original bed; (c) reattachment of the trochanter on the lateral femoral cortex; and (d) proximal reattachment
Trochanteric non-union has remained a problem, with reported rates of up to 17 % in routine arthroplasties [6]. However, in a series of 192 THRs, presented by the authors exclusively in patients with CHD, the rate of non-union was 3 % (Fig. 7.4) [5]. As it is noted by Eftekhar, those surgeons performing trochanteric osteotomy routinely obtained a better rate of union than those reserving the procedure for cases with difficult anatomical problems [4]. The distinct advantages offered by the TTA in THR for patients with CHD far overweight the risk of non-union and other complications.


Fig. 7.4
Non-union of the trochanter in a case with high dislocation. As a result the patient remained with a Trendelenburg gait postoperatively
7.2 Restoration of the Normal Centre of Rotation
The anatomical placement (true acetabulum) of the acetabular component is recommended mainly for biomechanical reasons [1, 7, 8]. On the basis of a mathematical model of the hip joint, Johnston et al. [9] suggested that the displacement of the centre of rotation of the cemented acetabular component medially, inferiorly and anteriorly reduces hip loads significantly. High placement of the component in the region of false acetabulum has also been proposed [10, 11]. The disadvantage of this technique is that with the acetabular component at this level, the lever arm for the body weight is much longer than that of the abductors and causes excessive loading of the hip (Fig. 7.5). Also, the shearing forces acting on the acetabular component at a higher level can lead to early loosening . In addition, in unilateral cases a high acetabular component does not correct leg-length and leaves the patient with a limb.
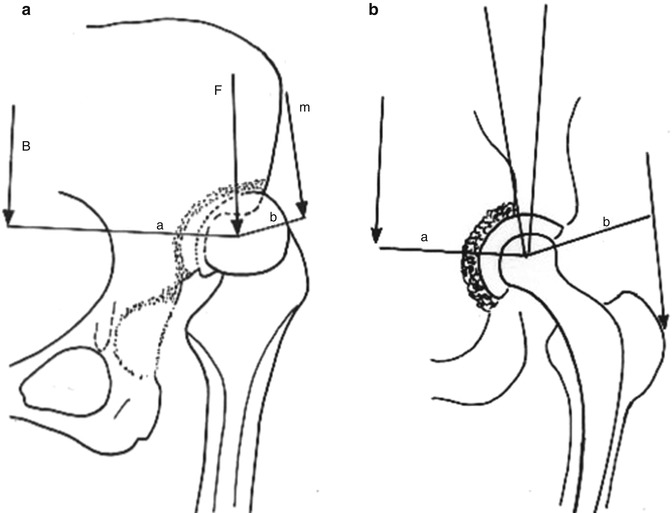
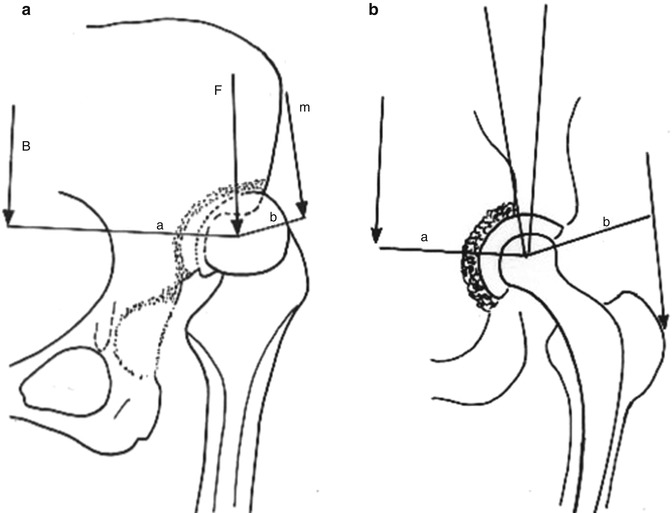
Fig. 7.5
(a) Forces acting on a hip with high dislocation: B body weight, m abductor force , F resultant force ; a lever arm of the body weight , b lever arm of the abductors . (b) By restoring the normal centre of rotation of the hip, the lever arm of the abductors (b) becomes equal to the lever arm of the body weight (a) minimising loads acting on the hip
7.3 Reconstruction of the Acetabulum
In low dislocation, the true acetabulum has to be excavated underneath the inferior part of the false acetabulum by removing the osteophyte that covers the upper part of the true acetabulum. In high dislocation, the true acetabulum is identified by using the thickened and elongated joint capsule as guide. Once the true acetabulum is located, two Hohmann retractors are inserted as markers of the most distal and anterior boundaries of the true acetabulum. One retractor is inserted at the acetabular notch, which corresponds to the superior margin of the obturator foramen. The second retractor is inserted anteriorly, taking care to avoid the possibility of fracture, engaging the thin anterior wall, into the inner wall of the pelvis (Fig. 7.6) [12].
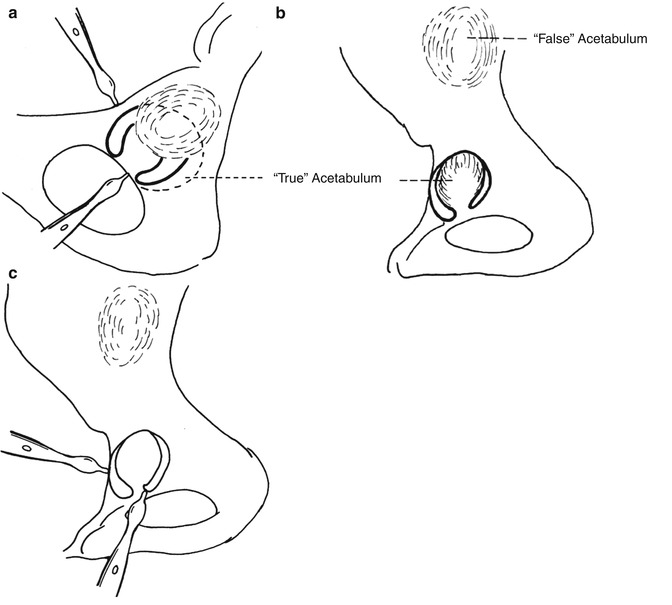
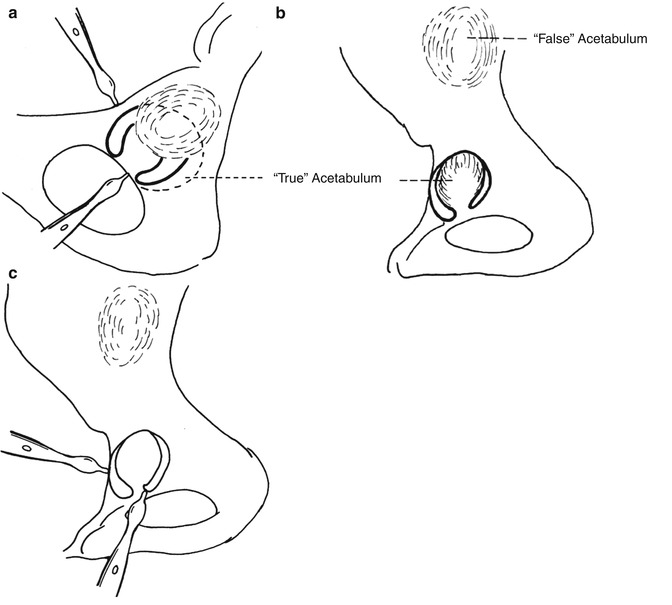
Fig. 7.6
(a) In low dislocation, the true acetabulum has to be excavated underneath the lower part of the false acetabulum. (b) In high dislocation, the true acetabulum is located following the elongated and thickened joint capsule. (c) Two Hohmann retractors, one inserted at the acetabular notch and the other at the anterior wall, indicate the most distal and the anterior boundary of the true acetabulum
Once a wide exposure of the area of the true acetabulum has been achieved, the procedure follows the same steps in low and high dislocation. The hypoplastic true acetabulum is widened and deepened with small (38–40 mm) diameter reamers, directed superoposteriorly (Fig. 7.7). Deepening is continued until the outer surface of the internal pelvic cortex is reached. After preparation of the true acetabulum, a press fit small diameter cementless cup is inserted at an angle of 40–45° to the horizontal and with 10° anteversion, when the remaining osseous cavity can accommodate it with at least 70–80 % coverage of the implant with bone (Fig. 7.8). Due to the poor acetabular bone stock in most hips with CHD and to the effort during surgery to obtain stable fixation of the cementless acetabular component, it is not always possible by using these implants to obtain optimal inclination , positioning (vertical and horizontal distance to teardrop) and full osseous containment .
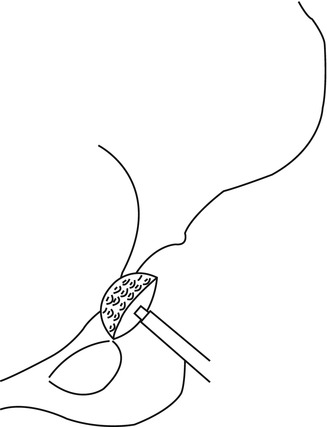
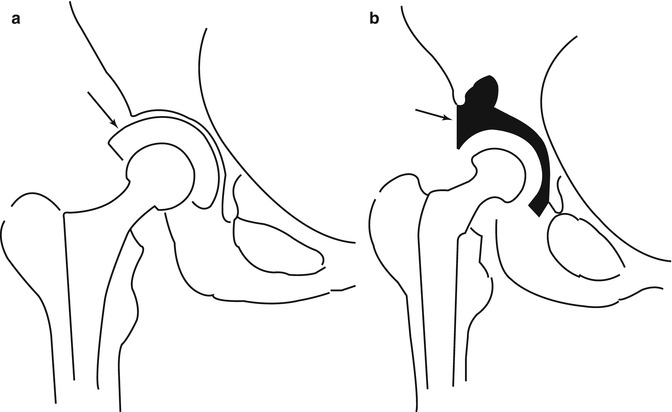
Fig. 7.7
Deepening of the hypoplastic true acetabulum, in low and high dislocations, is initiated with small diameter reamers (38–40 mm)
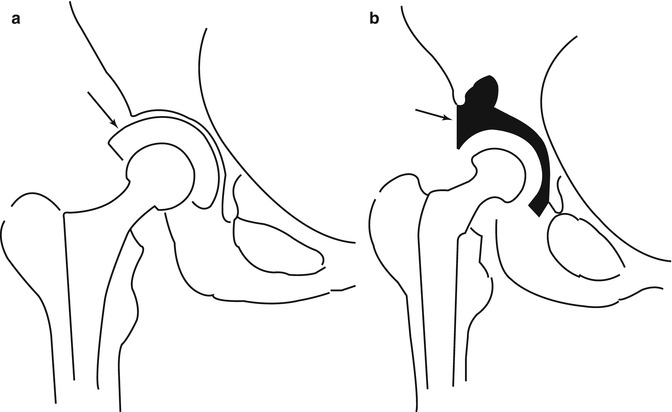
Fig. 7.8
For the reconstruction of the acetabulum, (a) cementless component can be used, when osseous cavity can accommodate it with at least 70–80 % coverage of the implant with host bone. (b) When cemented component is used, full coverage of the implant is necessary. Arrows indicate the extend of coverage of the acetabulum by host bone
The inclination, horizontal and vertical placement, and bony containment of the cementless acetabular component inserted in patients with CHD has been reported that affect on the loosening of acetabular and femoral components, wear of polyethylene and periprosthetic osteolysis [13]. Concerning the positioning of the acetabular components, biomechanical analysis showed that higher joint contact forces occurred with lateral placement of the cementless acetabular components in patients who did not have CHD [14].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








