I. Introduction—Tibial shaft fractures are one of the most common diaphyseal fractures treated by orthopaedic surgeons. The majority of these fractures heal without complication and most patients return to their preinjury level of functioning. Specific types of tibial shaft fractures are more prone to complication and require the expertise of a well-trained orthopaedist to avoid complication and optimize functional outcome.
II. Evaluation
A. History and Physical Examination
1. History—Patients with tibial shaft fractures experience pain in the leg after sustaining a low- or high-energy injury. Information about the nature and timing of the accident, any reduction or manipulation performed on the extremity and the patient’s significant medical history should be obtained.
2. Visual examination—All clothing should be removed from the extremity. The overall appearance of the extremity should be noted for open wounds, alignment, contusions, swelling, and color. Wounds should be assessed for size, location, degree of contamination, and severity of tissue injury.
• Deformities—Often a significant deformity is present at the level of the fracture. Contusions may indicate the point where a force was applied to the leg to create the fracture, or they may be incidental. The location of a significant contusion is important because it can necessitate a change in the treatment plan to avoid incising through badly traumatized tissue.
• Comparison to the contralateral leg—Comparison of the injured leg to the contralateral leg usually reveals a large amount of swelling. This swelling progresses with time. The amount of swelling present should serve as a preliminary index of the severity of injury to the tissues.
• Color—The color of the extremity reveals essential information about a limb’s perfusion. A pinkish color indicates oxygenated blood in the capillaries of the skin but reveals little about the deep circulation. A gray or dusky color, however, indicates circulatory compromise and a potential for limb loss if proper treatment is not provided promptly.
• Movement—After visually inspecting the leg, the physician should observe what the patient can do with the leg before the physician palpates or manipulates it. Attention should be directed at flexion and extension of the knee, ankle, and toes. Occasionally, the patient is too uncomfortable to comply with this part of the examination.
3. Palpation
• Pulses—An effort should be made to feel for pulses of the popliteal, dorsalis pedis, and posterior tibial arteries. If strong pulses are not appreciated, Doppler ultrasound should be used to evaluate the dorsalis pedis and posterior tibial arteries. If triphasic pulses are not present on Doppler ultrasound and the leg is deformed, traction should be applied to the extremity and the pulses reevaluated. If the pulses remain abnormal, emergent arteriography and/or consultation with a vascular surgeon should be obtained.
• Direct palpation—Occasionally, the injured leg appears fairly normal, and the results of the neurovascular exam are unremarkable. Direct palpation of the fracture, however, elicits pain and possible crepitation, which are indicative of a tibial shaft fracture.
4. Compartment syndrome—After ruling out vascular injury, the physician must evaluate for compartment syndrome. If the patient can actively flex and extend the ankle and toes without severe pain, compartment syndrome is not likely to be present at that time. Compartment syndrome can, however, evolve with time; thus serial examination and attention to the patient’s symptoms are necessary.
• Signs and symptoms—The alert patient commonly has a significant amount of pain from the fracture, and so ruling out compartment syndrome becomes more difficult. Pain out of proportion to the injury should make the physician suspicious. The most sensitive sign on physical examination is pain on passive stretch of the muscles in the involved compartment. Other significant signs are tight compartments, decreased sensation, and muscle weakness, although these signs may not always be present. Examination of the pulses is misleading since pulses may be palpable when compartment syndrome is present.
• Compartment Pressure—Evaluation of the compartments in the unconscious, intoxicated, or otherwise mentally impaired patient is more difficult because the patient has an altered response to pain. If there is any suspicion of compartment syndrome, then slit-catheter measurement of pressure in all four compartments is necessary to confirm or rule out the diagnosis. The exact pressure at which compartment syndrome occurs is variable. In general, a compartment-diastolic pressure difference of less than 30 mm Hg in any compartment is an indication for emergent four-compartment fasciotomy.
5. Open fractures—It must be assumed that open wounds in the vicinity of a tibial shaft fracture communicate with the fracture, and urgent irrigation and debridement should be planned (Fig. 11-1). Open wounds a distance away from the fracture may communicate with the fracture. Probing or inspection of extremity wounds for communication with the fracture should be performed in the operating room after sterile preparation and draping of the extremity.
B. Radiographic Evaluation—Radiographic evaluation of a tibial shaft fracture requires anteroposterior and lateral X-ray films. These X-ray films must include the entire tibia in addition to the distal femur and ankle, since associated fractures may be present and could alter the treatment plan. Computed tomography is occasionally helpful in delineating subtle fracture extension in very distal and very proximal shaft fractures. Stress fractures of the tibial shaft may not be visible on plain X-ray films. In this instance, an MRI scan or a three-phase bone scan assists in making the diagnosis.
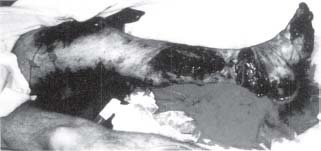
FIGURE 11-1 Clinical photograph of a young man involved in a coal mining accident showing severely contaminated wounds overlying his tibia fracture. Because of the significant tissue destruction this is a Gustilo type IIIb open tibia fracture.
III. Classification
A. Fracture—Several classification systems exist for the tibial shaft fracture. The importance of any system is its ability to differentiate fractures into treatment groups and its ability to predict outcome. For the closed tibial shaft fracture, the classification of Johner and Wruhs is straightforward and simple (Fig. 11-2). This classification system is based on the fracture location, the mechanism of injury, and the amount of energy dissipated in the fracture (i.e., the fracture comminution). The Arbeitsgemeinshaft für Osteosynthesfragen (AO) or Orthopaedic Trauma Association (OTA) classification is somewhat similar in scope but more detailed and complex. This classification is probably best used for accurately classifying fractures for research purposes because it allows for meaningful evaluation and comparison of fractures in different patients from different studies.
B. Open Fracture—Open fractures are best described using Gustilo’s grading system. Type I open fractures have small (<1 cm), clean wounds; minimal injury to the musculature; and no significant stripping of periosteum from bone. Type II open fractures have larger (>1 cm) wounds but no significant soft-tissue damage, flaps or avulsions. Type III open fractures have larger wounds and are associated with extensive injury to the integument, muscle, periosteum, and bone. Gunshot injuries and open fractures caused by a farm injury are special categories of Type III open fractures on account of their higher risk of complications, particularly infection. Type IIIa injuries have extensive contamination and/or injury to the underlying soft tissue, but adequate viable soft tissue is present to cover the bone and neurovascular structures without a muscle transfer. Type IIIb injuries have such an extensive injury to the soft tissues that a rotational or free muscle transfer is necessary to achieve coverage of the bone and neurovascular structures. These injuries usually have massive contamination. Type IIIc injuries are any open fractures with an associated vascular injury that requires an arterial repair. Often, what appears to be a Type I or Type II open fracture on initial examination in the emergency room is noted to have significant periosteal stripping and muscle injury at the time of operative debridement and may require muscle transfer for coverage with serial debridements. Thus there is a tendency for the Gustilo classification type to increase with time.
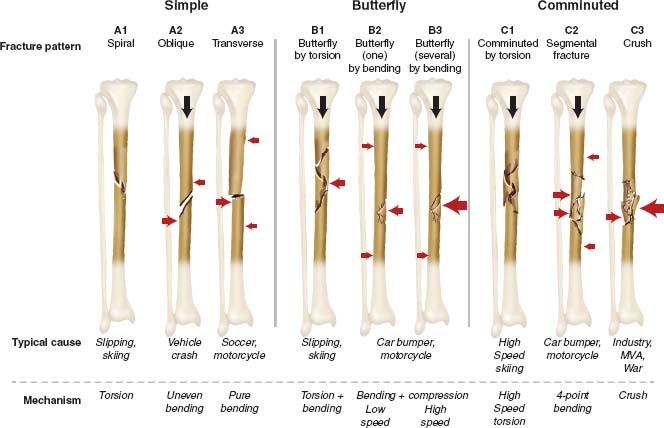
Fracture by torsion (A1, B1, C1): One spiral fracture line, the others ± longitudinal fibular fracture are usually at a different level
Fracture by bending (A2, A3, B2, B3, C2): Transverse on tension side (i.e., opposite fulcrum). Fibular fracture is usually at the same level
Fracture by crushing (C3)
FIGURE 11-2 Johner and Wruh’s classification system for tibial shaft fractures.
C. Soft-Tissue Injury—Tscherne has classified closed fractures according to the severity of the soft-tissue injury. Grade 0 injuries have negligible soft tissue injury. Grade 1 closed fractures have superficial abrasions or contusions of the soft tissues overlying the fracture. Grade 2 closed fractures have significant contusion to the muscle and/or deep contaminated skin abrasions. The bony injury is usually severe in these injuries. Grade 3 closed fractures have a severe injury to the soft tissues, with significant degloving, crushing, compartment syndrome, or vascular injury. The influence of the soft-tissue injury on treatment is discussed later.
IV. Associated Injuries
A. Fractures—Most tibial shaft fractures result from low-energy trauma and do not have associated injuries. As the severity of the tibial fracture increases, the incidence of associated injuries increases to greater than 50%. Injuries to the ipsilateral extremity, including knee ligament disruption, femur fracture, and ankle fracture, are among the most common associated injuries. Thus physical examination should be directed at ruling out these injuries before and after treatment of the tibial shaft fracture.
1. Ipsilateral fibula—Fracture of the ipsilateral fibula occurs with most tibial shaft fractures. This fracture can occasionally signify a significant injury to the ankle or proximal tibiofibular articulation, so the importance of a fibula fracture should not be underestimated.
B. Neurovascular Injuries—Injury to the neurovascular structures is also common; thus thorough serial examination of the circulation, sensation and motor function is necessary to detect these injuries early and to provide proper treatment.
C. Other Injuries—Associated injuries to the head, chest, and abdomen occur most commonly in patients with severe tibial fractures sustained from high-energy trauma. These patients require a thorough, systematic evaluation according to the advanced trauma life support (ATLS) guidelines to detect and treat these injuries as expediently as possible.
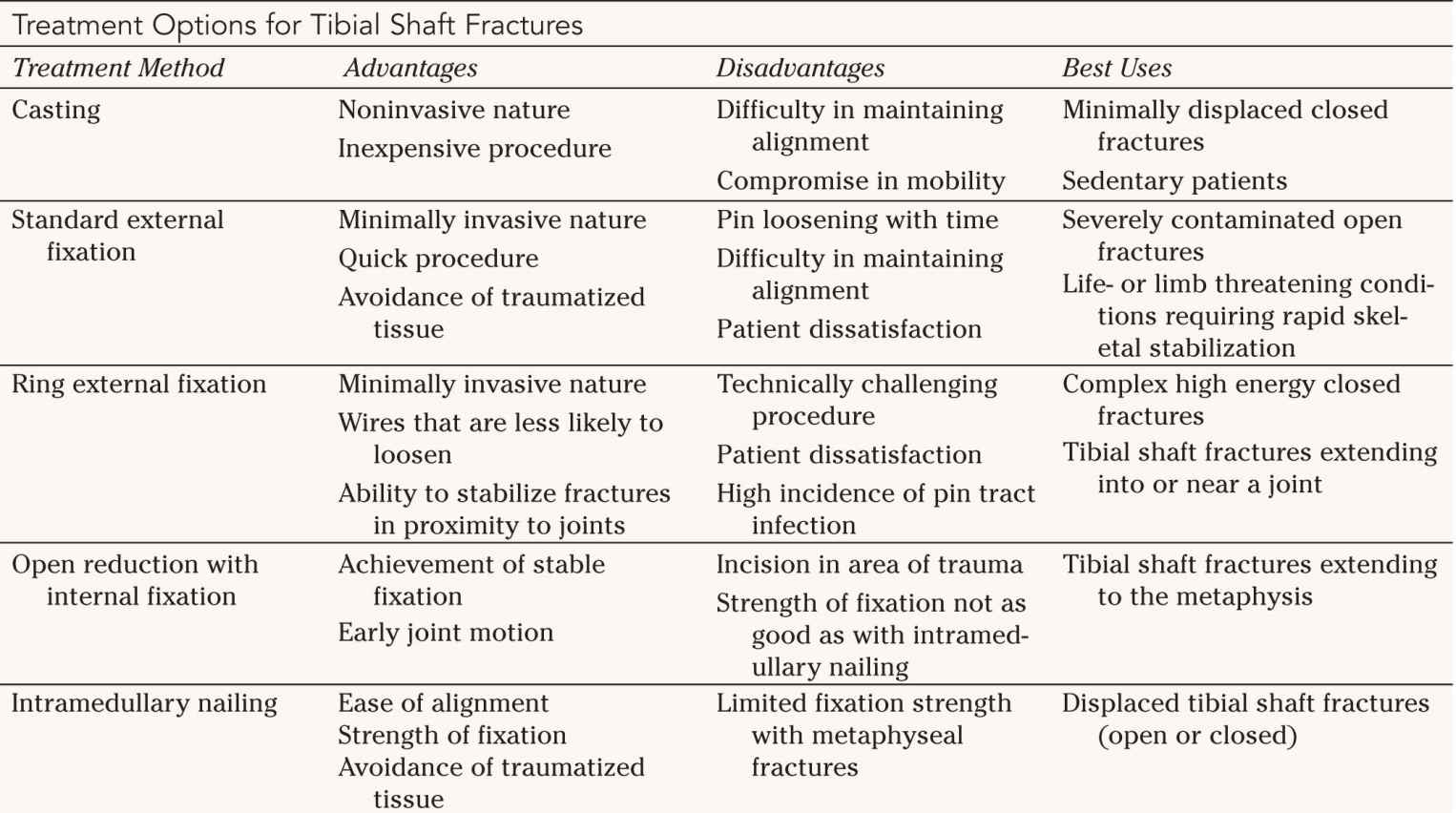
V. Treatment and Treatment Rationale (Table 11-1)
A. Nonoperative Treatment—Closed treatment of most tibial shaft fractures produces good-to-excellent results. Because it is inexpensive and fairly quick to perform, and because it carries little risk of complication, closed treatment should be the treatment considered first for most stable tibial shaft fractures.
1. Reduction—The technique of closed treatment begins with the administration of sedation or anesthesia to perform closed reduction of the fracture, if necessary. Reduction is achieved by hanging the leg over the stretcher and applying longitudinal traction. Manipulation of the fracture may be required to achieve proper alignment. X-ray films should be obtained after manipulation to ensure acceptable reduction.
2. Immobilization—The fracture should initially be placed in a well-padded long leg splint. Circumferential casting will not accommodate swelling and can lead to increasing pain and parasthesias subsequent to reduction. If a cast is applied, it must be bivalved to allow for soft-tissue swelling. The long leg splint or cast can be changed to a patella-tendon bearing (PTB) cast when soft callus has formed at the fracture site, at which time the fracture site will not have tenderness when pressure is applied. This may take as little as 8 to 10 days or, with some fractures, as long as 3 to 4 weeks. X-ray studies in the PTB cast are essential to confirm proper alignment. At this point, the patient may begin to bear weight on the extremity.


3. Alignment—There is considerable controversy regarding how much malalignment of a tibia fracture can be tolerated. Certainly, anatomic alignment with no angulation on the anteroposterior and lateral X-ray films is the goal, but this is not always achieved. Angulation in the sagittal plane is tolerated better than angulation in the coronal plane. This increased tolerance is due to the fact that the knee and ankle move in the sagittal plane, so this motion “makes up for” some angulation. Coronal plane angulation, however, results in varus or valgus malalignment, which produces asymmetric loading of the ankle and knee joints.
• Angulation—It is not clear how much angulation is required to produce osteoarthritis, since multiple factors influence the progression of osteoarthritis, including the location of the fracture and the age of the patient. In general, angulation of more than 10° in the sagittal plane and more than 5° in the coronal plane are significant enough to warrant remanipulation of the fracture or wedging of the cast. On the other hand, some surgeons argue that a tibia fracture that heals with as much as 20° angulation can be tolerated by most patients. (The authors do not agree with these surgeons.)
• Shortening—Shortening of 1 cm or less is rarely symptomatic, and shortening of 2 or 3 cm can be made tolerable with a 1.25 cm (0.5 in) shoe insert.
• Rotational malalignment—The amount of rotational malalignment that can be tolerated varies from patient to patient. In general, if the rotational malalignment affects gait or causes knee or ankle symptoms, operative correction should be considered.
4. Assessment of healing—The patient in a patella-tendon bearing cast should have radiographic evaluation of the fracture every 6 or 8 weeks. When the healing appears complete on X-ray films and the patient has clinical evidence of healing (i.e., no motion or pain with force applied across the fracture), then the cast is no longer required. This may be as early as 8 weeks after the injury but most commonly occurs 12 to 16 weeks after the injury. At this point, a rehabilitation program, including gait training, ankle rehabilitation, and strengthening of the quadriceps and gastrocsoleus muscles, quickens the return to normal function.
B. Operative Treatment
1. Indications
• Absolute—There are several absolute indications for operative stabilization of tibial shaft fractures. Open fractures should have stabilization of the fracture to provide a stable environment for soft-tissue healing and to facilitate wound care. Fractures with a vascular injury require skeletal stabilization to protect the vascular repair. Fractures with compartment syndrome should have skeletal stabilization to provide a stable environment for the injured tissues. Stabilization of the tibia should be performed in tibial shaft fractures in patients with multiple injuries to improve patient mobility, minimize pain, and possibly reduce the release of pro-inflammatory mediators.
• Relative—Relative indications for operative stabilization include significant shortening of the fracture on initial X-ray studies, significant comminution, a tibia fracture with an intact fibula (Fig. 11-3), and a displaced tibia fracture with a fibula fracture at the same level. In each of these fractures, there is a high incidence of malunion or nonunion with nonoperative treatment.
2. External fixation
• Standard—External fixation of a tibial shaft fracture is a quick and technically easy way to achieve fracture stability. For this reason, it is useful in a patient with multiple injuries who is hemodynamically unstable (“damage control”) or in a patient who would benefit from quick fracture stabilization before emergent repair of an arterial injury. It also can be used if an open fracture wound is severely contaminated and the surgeon has reservations about putting hardware in the wound. An external fixator can be applied through small incisions, thus avoiding additional trauma to tissues that may lack the ability to heal.
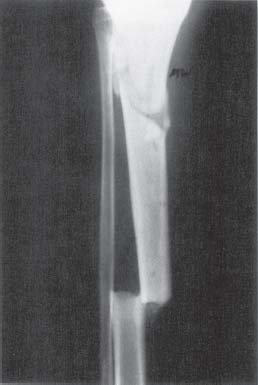
FIGURE 11-3 Anteroposterior X-ray film of a leg demonstrating a segmental tibia fracture with an intact fibula, a very unstable fracture.
• Ring fixators—Ring fixators, including Ilizarov and hybrid fixators (which use half-pins on one side of the fracture and rings with wires on the other side), offer the same advantages of traditional external fixators. These fixators obtain fixation with wires passed through bone. The wires are then placed on tension and attached to a ring. The ring is then attached to the external fixation frame, which may consist of a single bar or multiple, smaller threaded rods. The bars are secured to half-pins inserted into the bone. The advantage of wires and rings is that they provide a relatively noninvasive means of fracture fixation, and obtain good fixation strength, particularly with metaphyseal proximal or distal tibia fractures. Ring fixators require more expertise than traditional external fixators do, but can be used to fix fractures that are more complex and fractures with intraarticular extension without spanning the associated joint (Fig. 11-4). Furthermore, the wires of these fixators do not loosen as quickly as the half-pins used with traditional external fixators, so these fixators are useful for treating fractures that are likely to heal slowly.
3. Open reduction with internal fixation (ORIF)—ORIF is an excellent means by which to achieve stable fixation of a tibial shaft fracture and allow early postoperative motion. Successful healing is usually the rule. The chief risk of the procedure is wound-healing problems. In fractures with significant injury to the soft tissues of the leg, the use of a plate and screws may not be appropriate because the risk of wound-healing problems with this treatment may be too high. Severely traumatized legs with open tibial fractures (Gustilo type III) have a high incidence of wound-healing complications and deep infection when treated with ORIF.
• Fracture fragments—When ORIF of a tibial fracture is performed, the surgeon must respect the biology and physiology of all of the tissues. It is unnecessary and unwise to attempt to reduce and stabilize every fracture fragment, since attempts to do this often require extensive dissection and periosteal stripping. The result will be an attractive postoperative X-ray film of a tibia that lacks the ability to heal. It is preferable to obtain proper alignment and secure fixation of the proximal and distal tibia. The intervening bone fragments should be gently reduced with a dental pick, leaving their soft-tissue attachments alone so that they maintain their capacity to heal.
• Postoperative treatment—After ORIF of a tibial fracture, the incision should be closed over a suction drain and the leg splinted in neutral position to protect the soft tissues in the early healing phase. In 3 to 5 days, active motion of the knee and ankle should be initiated. Weightbearing should be prohibited until in the judgment of the surgeon, sufficient healing has occurred and the bone-plate construct can tolerate this. Often, a tibial fracture that has been treated with ORIF heals with minimal fracture callus (primary cortical healing). In these patients, a useful radiographic sign of fracture healing is “fading” or “blurring” of the fracture lines as new bone grows across the fracture line (Fig. 11-5) Weightbearing should begin with a protective orthosis, from which the patient can be weaned as healing nears completion and the patient becomes more comfortable.

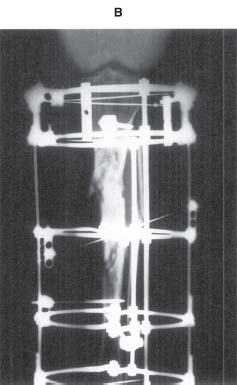

FIGURE 11-4 A. Anteroposterior X-ray film of a multifragmentary tibial shaft fracture caused by a gunshot wound. B. Postoperative X-ray film demonstrating excellent alignment achieved with an Ilizarov external fixator. C. Clinical photograph demonstrating minimal dissection of the skin in the fracture region.
• Minimally Invasive Plate Osteosynthesis (MIPO)—Techniques and devices have been developed that allow plate and screw fixation of tibial shaft fractures through small incisions and with limited dissection. This technique has the advantage of minimizing disruption of the peripheral blood supply to the bone, and potentially decreases wound healing problems. However, acceptable fracture reduction and stable fixation must be achieved if this technique is to be successful.
4. Intramedullary nailing
• Advantages—Intramedullary nailing has emerged as the most popular method for stabilizing displaced tibial shaft fractures. The advantages of intramedullary nailing are that proper alignment of the fracture is not difficult to achieve and the intramedullary location of the nail makes it more resistant to fixation failure (Fig. 11-6). Intramedullary nails are inserted through incisions near the knee, so badly traumatized tissues in the mid-leg can be avoided. Placement of interlocking screws can be performed percutaneously through small incisions. The use of proximal and distal interlocking screws maintains proper length and rotation of even an unstable, comminuted fracture until healing has occurred.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






