AO
Schatzker
Description
41-A
Extra-articular fractures
41-B
Partial intra-articular fractures
B1
I
Split fracture of the lateral plateau
B2
III
Depression fracture of the lateral plateau
B3
II
Split-depression fracture of the lateral plateau
41-C
Complete articular fractures
C1
V
Simple bicondylar fracture with simple metaphysal fracture
C2
Simple bicondylar fracture with comminuted metaphysal fracture
C3
VI
Comminuted articular and metaphysal fracture
25.6 Associated Injuries
Anterior cruciate ligament injuries are found in up to 23 % of patients, meniscal injuries in up to 50 % of patients, and collateral ligament injuries in up to 43 % of patients.
25.7 Management
The outcome following tibial plateau fractures is closely associated with the degree of articular depression and knee stability. Knee instability may result from the fracture itself and from accompanying injuries such as meniscal injuries or rupture of cruciate or collateral ligaments. For nondisplaced fractures, nonoperative management is justified. Displaced fractures require anatomic restoration of the intraarticular fragments.
25.7.1 Nonoperative Management
Nonoperative management is indicated for stable knee joints with articular depression <1 cm. The patient may undertake partial weight bearing in a hinged fracture brace for 8–12 weeks. The mainstay of nonoperative care is intensive physical therapy with early motion and isometric quadriceps exercises to avoid muscle atrophy and joint stiffness.
25.7.2 Operative Management
25.7.2.1 General Aspects of Surgical Management
Indications for emergency operative management are open tibial plateau fractures and tibial plateau fractures with associated neurovascular injuries or compartment syndrome. Displaced tibial plateau fractures (>1 cm articular depression) or tibial plateau fractures resulting in an unstable knee joint (more than 10° varus/valgus instability) are indications for operative management. The mainstay of operative care is open reduction and internal fixation (ORIF) with anatomic reduction, which is an important aspect for cartilage regeneration. Minimally invasive approaches (MIPO technique) are the standard of care for surgical management of tibial plateau fractures because the marginal soft tissue envelope predisposes for tissue necrosis and infection.
Delayed internal fixation with primary external stabilization may be necessary in high-energy injuries with severe soft tissue destruction. Nonlocking plates are suitable for simple fracture patterns with minimal comminution, whereas locking plates are indicated for high-energy fractures, those with severe comminution, and in osteoporotic bone. Adequate reduction should be achieved by the use fluoroscopy. Arthroscopic-assisted reduction and internal fixation may be helpful in pure depression fractures; however, extravasation of irrigation fluid, especially in extracapsular fractures, carries the risk of a compartment syndrome and must be used with extreme caution.
25.7.2.2 Lateral Plateau Fractures (AO-41-B1/B2/B3)
Fixation of pure split fractures of the lateral plateau (AO-41-B1//Schatzker I) may be achieved with two or three percutaneously inserted 6.5- or 7.0-mm partially threaded cancellous bone screws with washers. In cases of fracture fragmentation or in osteopenic patients, a lateral buttress plate may be used in an antiglide position (Fig. 25.1). In depression fractures of the lateral plateau (AO-41-B2//Schatzker III), the depression is elevated through a cortical window. Often, bone graft or bone substitute is needed. Stabilization is achieved with two or three 6.5- or 7.0-mm subchondral cancellous bone screws in “rafting” position (Fig. 25.2). In split-depression fractures of the lateral plateau (AO-41-B3//Schatzker II), the depression is elevated through the split component and the application of bone graft or bone substitute may be needed. Stabilization is achieved with lateral plate osteosynthesis with the proximal screws in “rafting” position (Fig. 25.3).
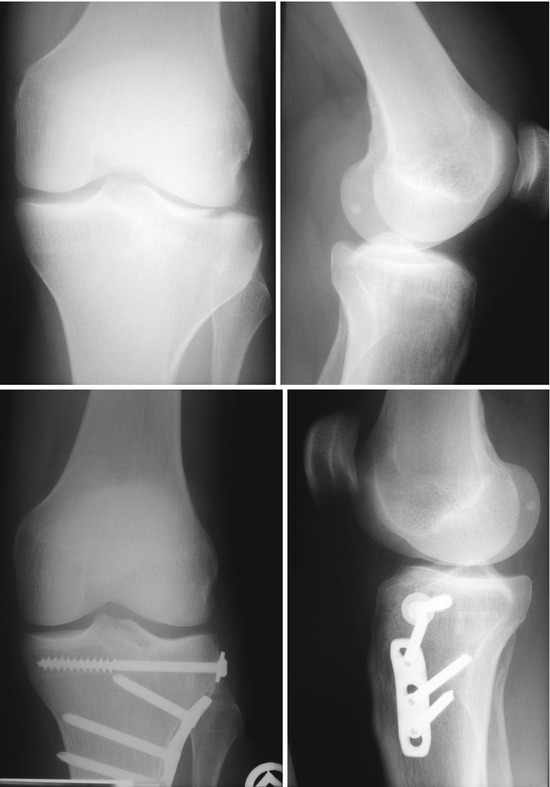

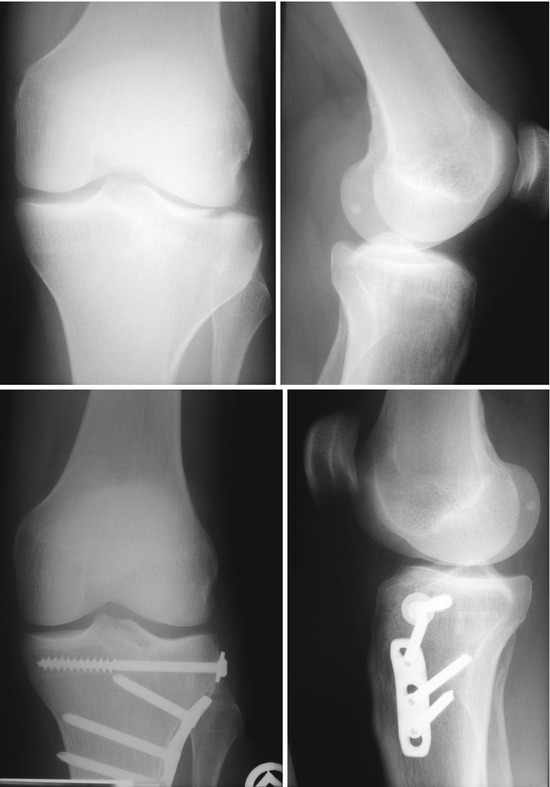
Fig. 25.1
AO-41-B1//Schatzker I fracture managed with a threaded 6.5-mm cancellous bone screw with washer and a lateral buttress plate in antiglide position

Fig. 25.2




AO-41-B2//Schatzker III fracture managed with four 6.5-mm subchondral cancellous bone screws in “rafting” position
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








