Fig. 6.1
The Superior Suspensory Shoulder Complex (SSSC) according to the description of Goss, 1993. Osseous structures of the SSSC ring are marked in black, the ligamenteous structures in red
6.3 Clinical and Radiologic Evaluation
History and the mechanism of the injury are helpful to identify scapula fractures and concomitant injuries. The physical examination is mandatory; it may reveal skin abrasions, lacerations, ecchymosis, swelling, or a flattened appearance of the shoulder girdle. The patient will complain about pain and motion will be reduced. However, sometimes the symptoms are unspecific or underscored by severe injuries of head, thorax, or spine so that scapular fractures are primarily missed or not adequately treated as the focus is on other life-threatening injuries. As concomitant vascular injuries or damage of neural structures (plexus) are common and greatly influence the overall outcome, a detailed neurologic examination and evaluation of the vascular status are part of the primary physical examination.
A radiographic examination based on a standard series of three projections (true a.p., axillary, and y-view) should be obtained for the diagnosis of a displaced scapular fracture. However, if the fracture shows a strong displacement and a surgical intervention is planned, the gold standard is three-dimensional computed tomography. The 3D reconstruction can be rotated into optimal planes for a comprehension of complex scapular injuries and for an accurate measurement of displacement, especially when the glenoid or the scapular neck are involved. Because computed tomography is easily available, scans are quick, and complete trauma scans are performed on most of the patients with severe thoracic trauma, conventional radiographic workups are not recommended as a standard diagnostic tool for scapular fractures. In case of concomitant injuries such as vascular damage or a neurologic deficit, the diagnostic methods have to be expanded and an MRI or angiographic examination must be added (Fig. 6.2).
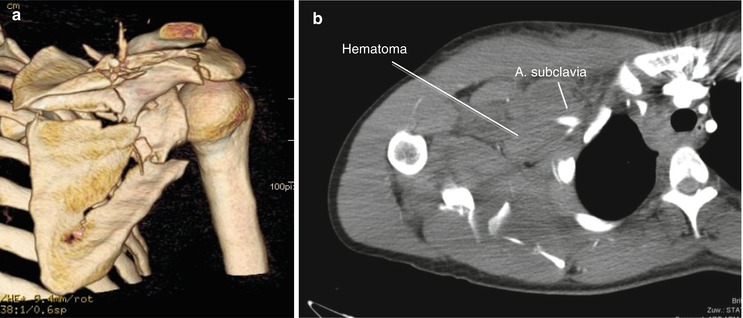
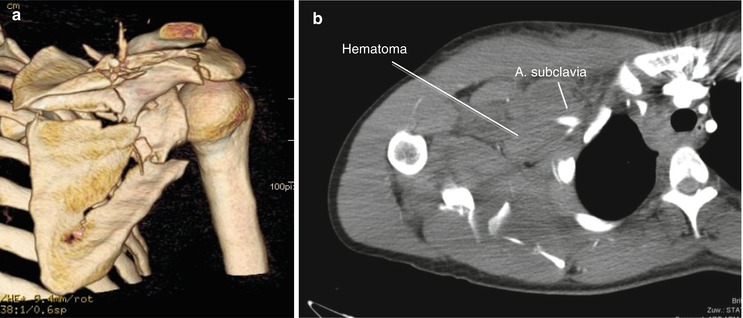
Fig. 6.2
Three-dimensional reconstruction of the computed tomography of a dislocated and unstable fracture of the scapula (a) as the gold standard in the diagnosis of scapular fractures. In case of concomitant vascular injuries, angiographic imaging should be added, demonstrating a ruptured subclavian artery with the surrounding hematoma (b)
6.4 Classification
Scapular fractures can be classified as extraarticular or intraarticular fractures, body-, neck-, or glenoid-fractures, displaced or nondisplaced fractures, and injuries with a stable or an unstable shoulder girdle. However, for clinical use and for scientific workup, a more sophisticated classification is necessary. In Europe, the classification described by Euler and Rüedi is commonly used and practicable [5]. Three subgroups describe extraarticular fractures (Type A: scapular body fractures, Type B: fracture of scapular process, Type C: fractures of the scapular neck), Type D fractures describe intraarticular fractures, and scapular fractures in combination with fractures of the humerus are classified as Type E. The complete Euler and Ruedi classification is shown in Table 6.1.
A | Fractures of the scapular body | |
B | Isolated process fractures | |
B1 | Spine | |
B2 | Coracoid process | |
B3 | Acromion | |
C | Fractures of the collum | |
C1 | Collum anatomicum | |
C2 | Collum chirurgicum | |
C3 | Collum chirurgicum and | |
(a) clavicula fracture | ||
(b) ruptured coracoclav. and coracoacrom. Ligaments | ||
D | Intra-articular glenoid fractures | |
D1 | Fractures of the glenoid rim | |
D2 | Fractures of the fossa glenoidalis | |
(a) with inferior glenoid fragment | ||
(b) transverse fractures through glenoid | ||
(c) separate coraco-glenoid fragment | ||
(d) fracture with multiple fragments | ||
D3 | Intraarticular glenoid fractures in combination with fractures of the collum or corpus | |
E | Fractures of the scapula in combination with proximal fractures of the humerus |
Fractures of the glenoid (intraarticular fractures, Type D) are subdivided according to the classification of glenoid rim and fossa fractures described by Ideberg [6] in 1995: Type I–fractures of the glenoid rim, Type IA anterior and Type IB posterior; Type II–transverse fractures through the glenoid fossa with an inferior fragment; Type III–transverse fracture exiting in the mid-superior scapula; Type IV–transverse fracture extending to the medial scapular border; Types V and VI–fracture with extension of a secondary fracture line to the lateral scapular border.
Complex shoulder injuries, often referred to as double lesions of the superior suspensory shoulder complex or “floating shoulders,” represent a special entity of scapular fractures. In most cases, these unstable shoulder girdle injuries are caused by the combination of a fracture of the scapular neck with a fracture of the ipsilateral clavicle or a lesion of the ipsilateral acromioclavicular joint. However, there are other injury patterns that can result in an unstable shoulder girdle, and a classification has not been described yet.
6.5 Nonsurgical Treatment
Many different publications and authors suggested criteria for surgical and nonsurgical treatment of scapula fractures, such as displacement, stability, medialization, angulation, or shortening [1, 7]. Although definitive proof of the benefit of surgical intervention is lacking for most fracture types, contemporary opinion defines two indications for surgery, displacement and instability. Stable, undisplaced, or minimally displaced fractures of the scapula should be managed conservatively.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








