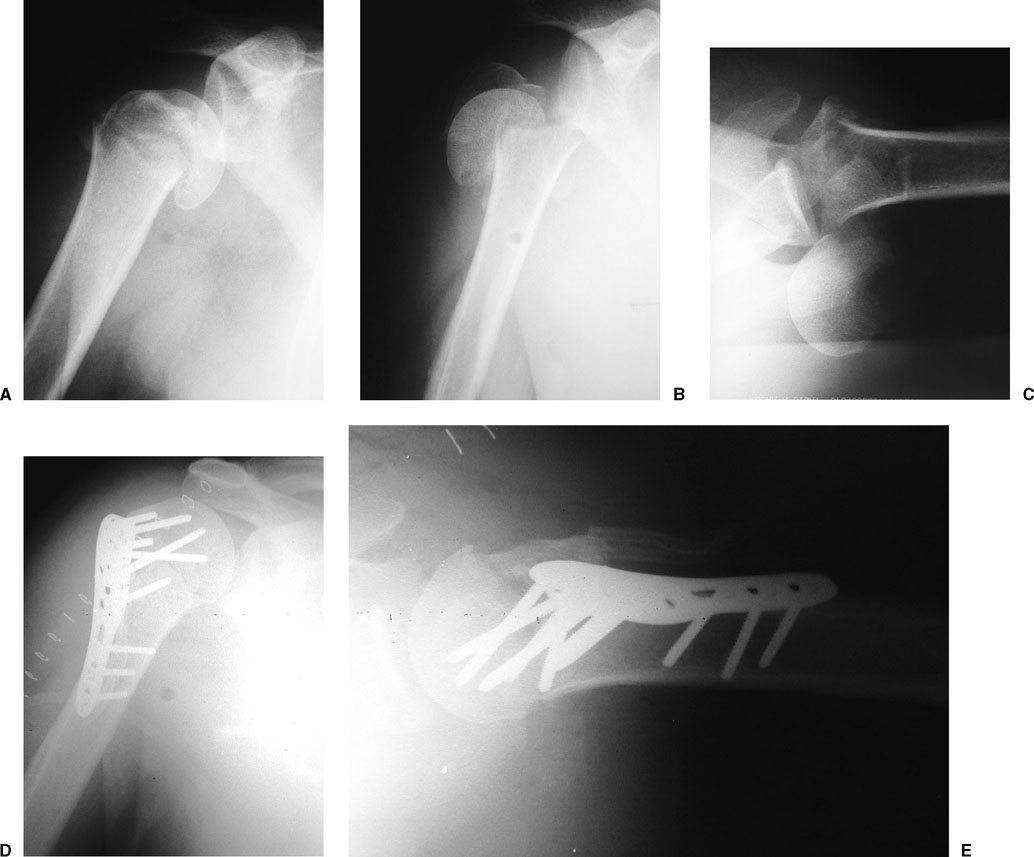
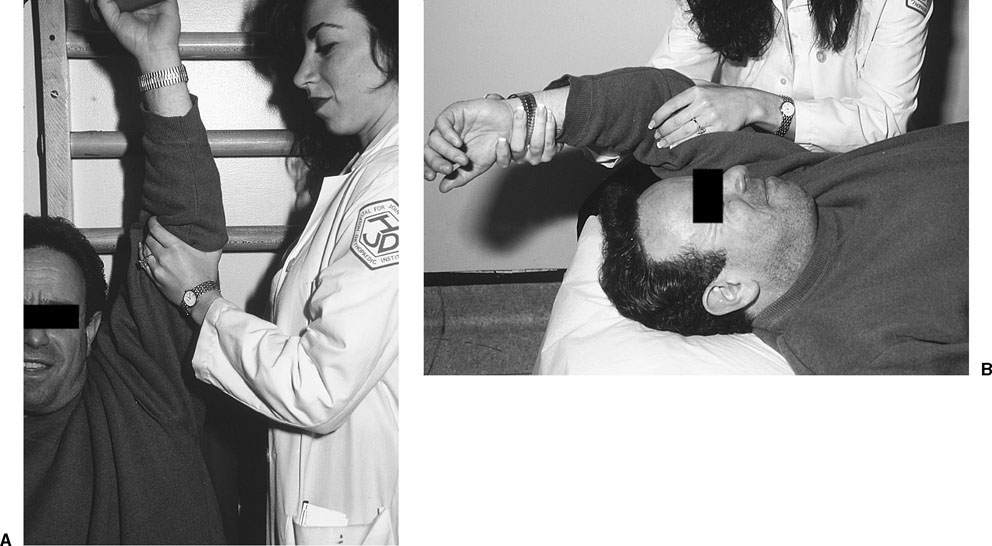
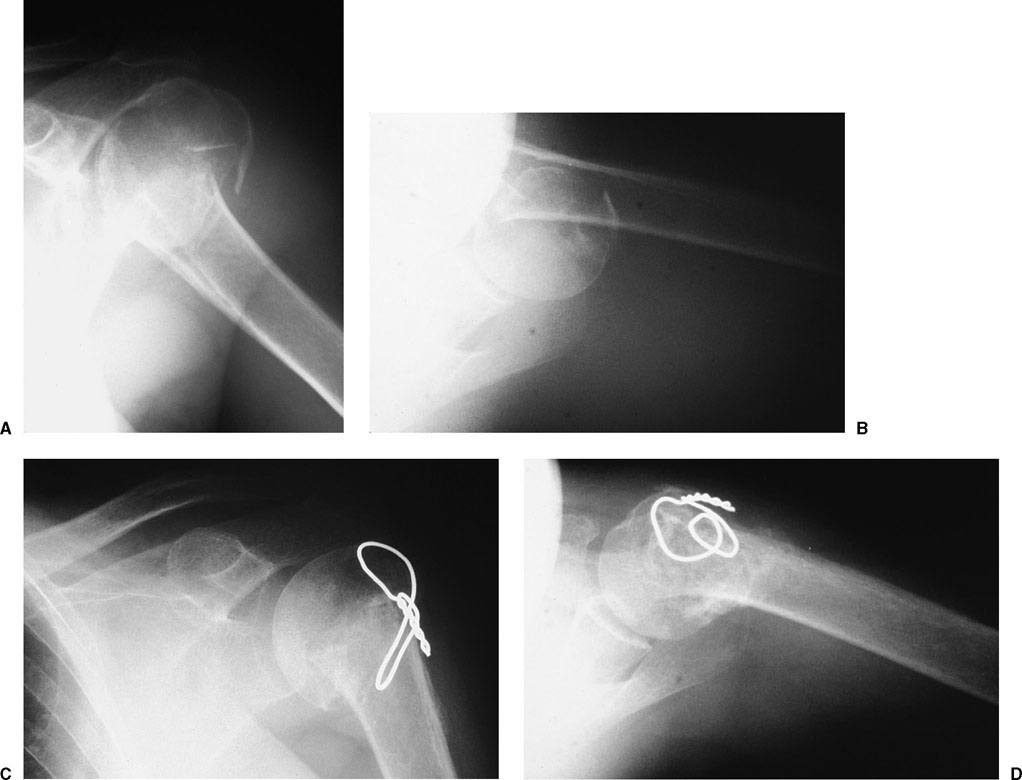
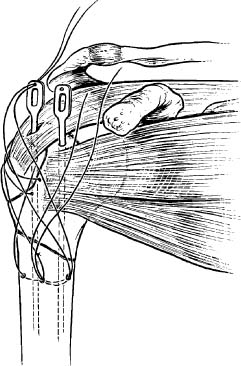
Proximal humerus fractures are common fractures and account for 10% of fractures in patients over age 65.1 Understanding the anatomy about the proximal humerus is paramount to developing a proper treatment plan for displaced three-part fractures. This chapter addresses three-part fractures and fracture-dislocations. Three-part fractures include more commonly surgical neck and greater tuberosity fractures, and less commonly surgical neck and lesser tuberosity fractures. The three-part greater tuberosity pattern can be associated with anterior dislocations, whereas the lesser tuberosity pattern can be associated with posterior dislocations. A detailed history should include handedness, and an assessment of activities of daily living and occupational as well as recreational activities. Chronicity of the injury should be documented, as it impacts the treatment options. Conditions predisposing to seizure such as medications, recent trauma, or stroke should be identified and treated in concert with the management of the fracture. On physical examination, one should expect swelling and tenderness about the shoulder girdle. If anterior dislocation is present, the head of the humerus may be palpable. Crepitation may be elicited with passive range of shoulder motion. Ecchymosis about the proximal humerus is usually present at 24 to 48 hours after injury and may track down the affected extremity or down the axilla. A careful neurologic examination is essential, as many patients with complex fracture patterns with or without dislocation may have an axillary or musculocutaneous nerve neuropraxia. Neurologic injury may be present in up to 45% of these injuries.2 Vascular examination must be performed. The presence of distal pulses, however, does not rule out a more proximal vascular injury, due to the rich collateral circulation about the shoulder. Penetrating injuries, a palpable thrill, or a bruit about the shoulder girdle necessitate vascular surgery consultation. As with all fractures about the shoulder, a standard shoulder trauma series should be obtained including anteroposterior, scapular lateral, and axillary views. The axillary view is critical to evaluate reduction of the glenohumeral joint (Fig. 6-1).3 If the patient cannot tolerate the positioning for the axillary, a Velpeau axillary view can be obtained. Computed tomography (CT) scan may provide additional useful information about involvement of the head (Hill-Sachs or head-splitting component) and tuberosity displacement. Although not required routinely, reformatted reconstruction views can be obtained to provide additional information about fracture anatomy. Most displaced three-part proximal humerus fractures require operative treatment. Exceptions to this are elderly patients with minimal functional ability and patients in whom surgery would be considered high risk. In these cases, a period of 7 to 10 days of immobilization (either for patient comfort or when the fracture moves as a unit) is followed by a structured and supervised rehabilitation program (Fig. 6-2). This program should include pendulum exercises as well as gentle passive range-of-motion exercises.4,5 Once there is radiographic evidence of healing, active range-of-motion exercises can be started. In one retrospective small series, two trauma centers compared their results for three-and four-part fractures. Sixteen patients (seven three-part fractures) treated nonoperatively were compared with 18 patients (eight three-part fractures) who underwent operative treatment. At follow-up no significant differences were found with regard to pain, function, and motion. As would be expected, there were no complications in the nonoperatively treated group.6 FIGURE 6-1 A 48-year-old, right-hand-dominant man was injured while skiing and sustained this three-part fracture-dislocation. The anteroposterior (AP) radiographs (A,B) do not show the posterior dislocation that is evident on the axillary view (C). Open reduction and internal fixation (ORIF) was performed with a locking plate (D,E). The postoperative axillary view (E) shows a concentric reduction. Other studies have reported good functional results with nonoperative treatment of comminuted proximal humerus fractures. In a long-term follow-up study of 17 patients with three-and four-part fractures, mean Constant shoulder scores averaged 59 for three-part and 47 for four-part fractures at 10 years.7 These numbers compared favorably with a second series of operatively treated three-and four-part fractures at 3 years. Mean Constant scores were 51 for three-part and 46 for four-part fractures.8 A three-part fracture consists of a surgical neck fracture with either a greater or lesser tuberosity fracture. Most three-part fractures are treated with reduction and fixation. In some cases, when bone stock is poor, prosthetic replacement may be chosen. The technique for prosthetic replacement is described in Chapter 7. Operative treatment options include closed reduction and percutaneously placed pins or cannulated screws if closed reduction is chosen. If open treatment is chosen, internal fixation options vary and include plate and screws, Enders rod and tension band fixation, tension band fixation alone, and locked intramedullary nailing. FIGURE 6-2 (A,B) A structured, supervised rehabilitation program relies on the interactions between the patient, the therapist, and the orthopaedic surgeon. Percutaneous pinning of three-part proximal humerus fractures is an attractive option when a closed reduction can be obtained. The advantages of this technique include minimal soft tissue dissection, decreased bleeding, and generally reduced morbidity.9 In addition, the minimized scarring and adhesions with early range of shoulder motion can be beneficial with respect to final shoulder range of motion. The operative technique is demanding and requires proper radiographic image intensification. Closed manipulation of the fracture fragments should correct the adducted position of the humeral shaft (secondary to the medial pull of the pectoralis muscle) combined with varying degrees of internal and external rotation to bring the proximal fragment in opposition to the tuberosity. Longitudinal traction, with adduction and internal rotation helps to reduce the humeral head to the shaft (Fig. 6-3).10,11 With the reduction confirmed fluoroscopically, terminally threaded Schantz pins or threaded Kirschner wires (K-wires) are inserted lateral to medial and anteriorly to posteriorly. Pin insertion should be done with careful consideration of the anatomic structures at risk. In particular are the long head of the biceps and cephalic vein. Based on one anatomic study, a relative safe zone for lateral pin placement is from a point approximately two head diameters distal to the top of the humeral head to the deltoid tuberosity.9 At least one pin is directed from superolateral to infero-medial to capture the greater tuberosity fragment. This pin should be placed while the patient’s shoulder is held in external rotation to minimize risk to the axillary nerve and directed to exit medially 2 cm distal to the inferior medial articular surface.9 The use of terminally threaded 2.5-mm Schantz pins should prevent pin migration, which has been reported as a complication of this technique.12 This technique is most suitable for younger patients with good-quality bone. Fixation is likely to be less secure in older patients, although the technique can be utilized successfully in these patients with proper attention to detail and close postoperative follow-up. Jaberg et al13 reported on their experience with 48 patients treated with percutaneous wire fixation. Their cohort included two-, three-, and four-part fractures. Of the eight patients in their series with three-part fractures, all had a good or excellent result. Complications included pin tract infections in four and symptomatic osteonecrosis in two patients with anatomic neck fractures. In an attempt to avoid the two largest complications with this technique, pin tract infection and stiffness from the period of immobilization required secondary to a prominent superolateral pin, some authors have advocated the use of cannulated screws. Chen et al11 reported on 18 patients who were treated with percutaneous pinning or cannulated screw fixation of two-and three-part fractures including six three-part fractures in their series. All but one of the fractures united and all of the three-part fractures had satisfactory clinical outcomes. One patient who was pinned with K-wires had a skin problem that resolved after wire removal. FIGURE 6-3 A 76-year-old man with displaced three-part fracture involving the surgical neck and the greater tuberosity (A–C). Closed reduction and percutaneous pinning was performed (D,E). Follow-up radiographs 6 months later show the fracture to be healed with excellent alignment (F,G). FIGURE 6-4 A 69-year-old woman with a three-part greater tuberosity fracture (A,B) treated by the open tension band wire technique (C,D). In another series of three-and four-part proximal humerus fractures, 27 patients (including nine with three-part fractures) were treated with percutaneous screw fixation.10 At 2-year follow-up, the three-part group had an average constant score of 91 and no cases of osteonecrosis. The small numbers and mixture of fracture patterns in all of these series make it difficult to draw meaningful conclusions. The tension band technique described by Hawkins et al14 is an open procedure (Fig. 6-4). We utilize the tension band techniques in elderly patients with poor-quality bone. Because all of these techniques depend more on the rotator cuff-tendon bone interface than on the often thin and osteoporotic tuberosity fragments, hardware failure is less likely. The patient is placed in the beach chair position with the head secured. A deltopectoral incision is made with the arm in abduction to facilitate mobilization of the deltoid muscle. Once the fracture fragments are identified, the tuberosity fragment is reduced to the articular segment, which is then reduced to the shaft. The technique was originally described with the use of wire, but we prefer the use of No. 5 nonabsorbable braided suture. Two drill holes are placed in the shaft in an in-and-out technique. These sutures are then passed in a figure-of-eight fashion through the supraspinatus tendon insertion across the rotator interval. Additional sutures (two or three) are passed in a similar fashion, including one encompassing the infra-spinatus tendon insertion and another encompassing the subscapularis. These sutures are tied securely to achieve the desired fixation. The rotator interval is then repaired and the shoulder tested to assess stability and determine parameters for the postoperative rehabilitation plan. The Hawkins technique utilized wire passed through the bone of the tuberosity and the articular segment. They reported their results on 15 patients with three-part fractures using this technique. All 15 fractures united by 6 weeks. The active forward elevation averaged 126°. There was one poor functional result in a patient who had sustained an axillary nerve injury. There was one early failure of the tension band and two cases of osteonecrosis. One patient required revision to hemiarthroplasty.14 An alternate to this technique is the modification of adding a supplemental cancellous lag screw to enhance fixation.15,16 The screw is placed from the lateral humeral cortex and angled toward the articular surface. The tension band fixation is placed around the head of the screw. In a series of 13 patients Cornell et al15 used this technique to treat two-and three-part fractures. At final follow-up at an average of 20 months, all fractures had united. Four of the five patients with three-part fractures had good functional shoulder scores and one had a fair result. There were no complications in this series. This technique combines intramedullary fixation using modified Enders rods with a suture tension band technique for secure head and tuberosity fixation (Fig. 6-5). This technique is preferable when there is medial neck comminution and the surgical neck is tipped into a varus position. A deltopectoral approach is utilized. The incision starts just lateral to the coracoid process and curves distal and lateral toward the deltoid tuberosity. The cephalic vein is identified and retracted laterally to protect its branches. Next the clavipectoral fascia is incised, and the conjoined tendon of the coracobrachialis and biceps is retracted medially. Partial release of the pectoralis major may facilitate shaft reduction by removing a deforming force. The displaced tuberosity, whether it is the greater or lesser tuberosity, is identified and mobilized. Tag sutures are placed into the rotator cuff to help mobilize the fracture fragments. The tuberosity is reduced and repaired to the head fragment first. This can be done with wire as described by Hawkins et al,14 or, as we prefer, heavy nonabsorbable suture. Flexible rods such as Enders are placed through the head down the humeral shaft. Rotational stability is obtained by the three-point bend on the rods.17 Some implant manufacturers (Smith and Nephew Richards, Memphis, Tennessee) have modified the Enders rod by adding a hole superior to the eyelet in the rod (Fig. 6-5). This enables the Enders to be buried deeper within the bone and minimizes the risk of encroachment on the subacromial space. The tension band is then passed through the rotator cuff and the superior eyelets of the Enders and tied in a figure-of-eight fashion through drill holes in the shaft (Fig. 6-6). Passing the suture through the humeral head and tuberosities prior to passage of the rods will limit the superior migration of the rods as long as the tension band is intact. The shoulder is then placed through a range of motion to assess stability. A passive range of shoulder motion program is begun immediately. Active motion is started 6 weeks after surgery when fracture healing has occurred (Fig. 6-6).
Three-Part Fractures and Fracture-Dislocations
 Clinical Evaluation
Clinical Evaluation
Radiographic/Imaging Studies
 Treatment
Treatment
Nonoperative
Operative
Percutaneous Pinning
Tension Band Technique
Enders and Suture Tension Band
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree