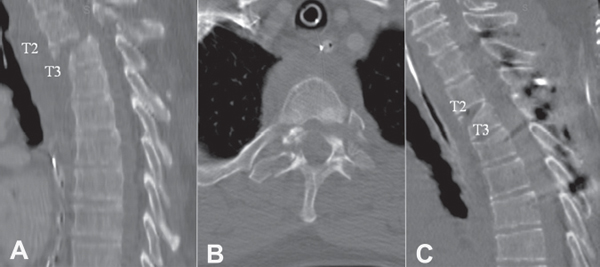
14 The thoracolumbar spine is a complex morphological structure that provides a challenging task regarding the evaluation and management of a traumatized patient. Fracture dislocations usually involve high-energy trauma and are associated with multisystem injuries. Diagnosis can be difficult because of the multiple distracting injuries. A patient might be physiologically unstable, preventing accurate history, physical examination, and radiological work-up. A thorough understanding of the complexities of thoracolumbar fracture dislocations is necessary. Management should therefore be conducted by a well-experienced multidisciplinary team. The mechanical characteristics of the thoracolumbar junction place it as the most common site for spinal injuries. The thoracic spine is considered a stable segment because of the protective and stabilizing effects of the rib cage. The lumbar spine, as a mobile segment, creates a lever arm at this transitional zone. The L1 vertebra is the most common site of spinal fracture, and the T12 is the next most common site. Thoracolumbar fracture dislocations occur most frequently as a result of motor vehicle accidents and falls from heights. Both mechanisms involve high-energy impact and are frequently associated with spinal cord injury. Thoracolumbar fracture dislocations found in neurologically intact patients are those with spontaneous decompression of the spinal elements and widening of the spinal canal. Several classification methods have been suggested over the years for thoracolumbar injuries. Unfortunately, no consensus exists among spine surgeons regarding the use of a single method with which to classify these injuries. With the advent of computed tomography (CT), Denis developed the “three column” concept in 1983. To this date, no one has validated the concept of the middle column. Denis defined four categories of major spinal injuries based on the mechanical forces at the time of impact: compression fractures, burst fractures, seat belt–type injuries (Chance fractures), and fracture dislocations. Fracture dislocations are defined as failure of all three columns under compression, tension, rotation, or shear. In his study, Denis classified three types of fracture dislocations: flexion-rotation, shear, and flexion-distraction injuries. The flexion-rotation type fracture was the most commonly observed. In the 1990s, the AO group suggested a different type of classification for spinal column injuries. This mechanistic classification system is based on the three basic functions of the normal and stable spine while resisting implied external forces: axial compression, axial distraction, and torsional forces. Three types of major injuries are as follows: Type A, compression; Type B, distraction; and Type C, rotation injuries. The AO classification demonstrates the severity of the injury, increasing instability, and risk of neurological compromise from Type A to C patterns. The groups are further divided into 27 total subtypes. This comprehensive and logical classification system has no specific advantage regarding fracture dislocations (Type C). However, with a more accurate and detailed description of the wide spectrum of injuries, it allows a more precise estimation of the severity of the fracture dislocation. In 2005, Vaccaro et al. presented the Thoracolumbar Injury Classification and Severity Score (TLICS). This classification method was developed to serve more as an outcome-predictive tool and less as an injury morphology description method. This classification combines several factors regarding thoracolumbar injuries, including assessment of spinal stability, future deformity, and progressive neurological compromise. One of the goals of the TLICS was to help spine surgeons in their clinical decision making. Three major variables were identified as critical in serving this purpose: (1) the morphology of the injury, (2) the integrity of the posterior ligamentous complex (PLC), and (3) the neurological status of the patient. Morphology refers to the three known types of injury forces affecting the human spine: compression, translation and/or rotation, and distraction. The PLC includes the supraspinous and interspinous ligaments, ligamentum flavum, and facet joint capsules. The role of this complex is to serve as a posterior tension band, and disruption of these structures usually requires surgical stabilization because of their poor healing ability. Information gathered from plain radiographs, CT scans, and MRI can categorize the PLC integrity as intact, indeterminate, or disrupted. Neurological status is the third element because of its important role in predicting prognosis and as a tool for treatment plan decision making. Four levels are considered: neurologically intact, nerve root injury, complete spinal cord injury, and incomplete spinal cord injury and cauda equina injury. An injury severity score is calculated by adding numeric values collected within each subgroup of the main three categories. A score of 3 or less indicates an injury that can be treated nonsurgically, a score of 5 or more indicates an injury for which surgery is recommended, and a score of 4 denotes a discretionary case, allowing clinical scenarios to bias the surgeon toward surgical or nonsurgical management. Although the usefulness of the TLICS is promising, long-term follow-up data regarding its prognostic value need to be collected and assessed. The majority of patients diagnosed with thoracolumbar fracture dislocation have incurred multiple traumatic injuries. Treatment begins at the accident scene according to the Advanced Trauma Life Support (ATLS) guidelines. The patient should be immobilized and secured in a neutral position of the vertebral column, including a rigid cervical collar and a backboard. Detected hypotension can be caused by hemorrhage in addition to neurogenically mediated shock. Maintaining the mean arterial blood pressure above 85 mmHg is thought to maintain spinal cord perfusion and can improve neurological outcome. A full assessment of the chest and abdomen should be performed by a multidisciplinary trauma team to rule out any immediate life-threatening injuries. In the case of an unconscious patient, the medical team at the scene can provide additional information regarding mechanism of injury. Physical examination of these patients should be handled with a systematic multidisciplinary team approach, taking into consideration all bodily systems. Examination of the vertebral column and the neurological examination should be performed under the assumption that an unstable injury is highly suspected until proven otherwise. The physical examination of an unconscious patient can be challenging, and in most cases, the only clues for spinal cord function can be obtained from emergency medical technician personnel on the scene with reports of spontaneous movements. Reaction to touch and/or painful stimuli might allow for assessment of spontaneous movements of the extremities. Additionally, asynchronous activity of normal chest motion versus diaphragmatic respiration might be a subtle clue of spinal cord injury. Signs of thoracic trauma, including ecchymosis, lacerations, abrasions, and step-off while palpating the spinous process, should alert the physician to a spinal column injury. A thorough motor and sensory neurological evaluation using the standard American Spinal Injury Association (ASIA) scoring method should be conducted. Additionally, the presence or absence of reflexes, including Babinski (upper motor neuron lesion), cremasteric (T12–L1), anal wink (S2, S3, S4), and bulbocavernosus (S3, S4) reflexes, should be assessed. Any painful area on the thoracolumbar spine should be analyzed with anteroposterior and lateral radiographic views. In cases in which plain imaging findings are negative and in cases that require more thorough evaluation of the complexity of the thoracolumbar injury, CT scans can be obtained. Coronal and sagittal reconstructions can be helpful in gaining a better understanding of the bony injuries and can be used to assess the magnitude of bony canal compromise (Fig. 14.1). In patients with neurological deficits, MRI can be useful to determine the magnitude of soft-tissue canal compromise, such as hematoma, traumatic meningocele, and compromise by a herniated disk. In addition, MRI can assess whether the injury is at the cord, conus, or cauda equina level. From a prognostic standpoint, MRI can also assess edema of the spinal cord and conus medullaris. MRI can also provide additional information regarding discoligamentous disruptions at the site of the thoracolumbar dislocation. Fracture dislocations are unstable because of the magnitude of the spinal column disruption in addition to associated neurological deficits. Therefore, surgical treatment is recommended for most of these cases. When physiologically stable, the patient can be brought to the operating room. The goals of surgery are to improve or to preserve neurological function, to realign the spine, to stabilize the spine, to prevent post-traumatic deformity, and to enable early mobilization with aggressive rehabilitation. The basic tenets of neurological recovery teach that patients with complete neurological deficits will achieve no significant gains in return of function. On the other hand, patients with incomplete deficits can make significant neurological gains with a decompressive and stabilization procedure. Decompression can be performed indirectly via fracture dislocation relocation or directly via an anterior approach. Alternatively, posterior decompression in the thoracolumbar spine can be performed through extracavitary or transpedicular decompression. Stabilization of the spine with modern implants through an anterior and/or posterior approach enables a patient to begin the rehabilitation phase aggressively and reduces the need for postoperative bracing. Thus, fracture dislocations in patients who are neurologically intact typically require posterior reduction, stabilization, and fusion with pedicular instrumentation. Fig. 14.1 T2–T3 flexion-rotation fracture dislocation that resulted in complete spinal cord injury. (A) Sagittal CT imaging. (B) Axial CT imaging. (C) With clear instability, spinal column was reduced and stabilized posteriorly.
Thoracolumbar Fracture Dislocations
![]() Classification
Classification
Denis Classification of Acute Thoracolumbar Spinal Injuries
AO Types
Thoracolumbar Injury Classification System
![]() Patient Management
Patient Management
![]() Treatment
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







