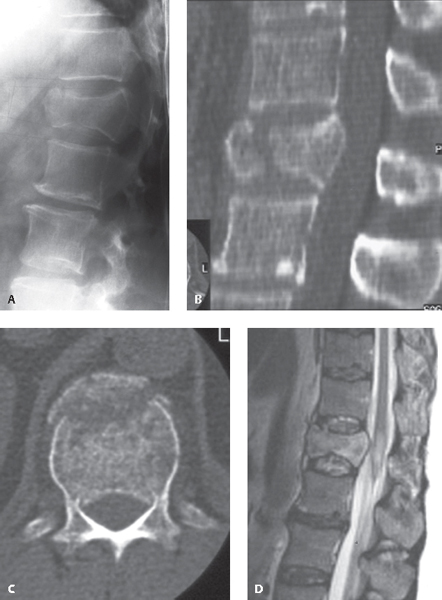
12 Thoracolumbar junctional burst fractures include spinal injuries between the T11 and L2 vertebral levels that result in posterior vertebral wall failure and retropulsion into the spinal canal due to greater than physiologic axial loading forces. The hallmark of these fractures is some degree of bony retropulsion into the spinal canal or violation of the posterior spinal canal cortical margin. Occasionally there will be a herniation of the nucleus pulposus of the intervertebral disk through the respective upper endplate into the vertebral body. Anatomically, the rigid thoracic spine transitions to a more mobile lumbar spine, which predisposes this junction to increased dispersal of energy and the potential for a fracture. Almost 90% of all burst fractures occur at the thoracolumbar junction, representing a fifth of all spine fractures, occurring most commonly in young males and following high-speed motor vehicle collisions.1,2 No universal classification system for thoracolumbar trauma presently exists. Historically, the most commonly used scheme in North America is the Denis classification system. In this system, the spine is divided into three columns. The anterior column consists of the anterior longitudinal ligament (ALL), annulus fibrosus, and anterior half of the vertebral body. The middle column consists of the posterior longitudinal ligament (PLL), the posterior portion of the annulus fibrosus, and the posterior half of the vertebral body. The posterior column consists of the bony neural arch, the posterior spinous processes, the ligamentum flavum, and the facet joints. A recent and presently more popular thoracolumbar fracture classification system is the TLICS (Thoracolumbar Injury Classification and Severity Score) system, which describes the morphology of the fracture, the status of the posterior ligamentous complex, and the neurologic status of the patient. There should be a high suspicion for a thoracolumbar fracture in all trauma patients. This is particularly true in individuals who fall from heights and land on their feet, since this creates high-energy axial compression at the thoracolumbar junction. Patients who have calcaneal fractures due to falls should be evaluated for a thoracolumbar fracture. Patients with a suspected thoracolumbar fracture should be immobilized and placed on flat bed rest. The patient should be kept immobilized until a trauma evaluation has been completed, including a thorough neurologic exam and review of imaging of the entire spinal axis. Plain-film radiographs may help as a screening tool; however, all patients suspected of having a burst fracture should be evaluated by computed tomography (CT). There is a high incidence of concurrent noncontiguous fractures for patients with thoracolumbar fractures; therefore, the entire spinal axis should be imaged (Fig. 12.1A). Additionally, it is common practice to perform a baseline CT scan of the head to survey for intracranial hemorrhage or contusions. Spinal CT with reconstructed images is excellent at demonstrating spinal alignment, osseous architecture, and canal encroachment from retropulsed bone fragments of the vertebral body or laminae (Fig. 12.1B, C). Magnetic resonance imaging (MRI) is particularly valuable for demonstrating injury to the soft tissues. This modality can reveal the extent of damage to the spinal cord and the presence of ligamentous disruption as well as disk protrusions; however, it may be oversensitive in detecting nonspecific soft-tissue injuries (Fig. 12.1D). The treatment of thoracolumbar burst fractures is controversial, and there are no uniformly accepted algorithms or protocols. Operative management is often directed by the patient’s neurologic examination. Surgery in patients with complete neurologic deficits (ASIA A) rarely results in improvements in neurologic function, but it may be indicated to correct a spinal deformity or to confer stability to allow for accelerated rehabilitation. Therefore, the goal of surgery for complete deficits, American Spinal Injury Association (ASIA) A, is to achieve bony healing and stability, and to allow the patient to be mobilized for early rehabilitation. The patient population deriving the greatest benefit from spinal decompression is the neurologically incomplete patient (ASIA B–D). However, operative treatment has yet to be proven in randomized controlled trials to have outcomes superior to those of conservative management in regard to functional outcome and pain scores.2 Surgical treatment has been correlated with improved correction of kyphotic deformity, earlier return to work, and decreased requirements for external immobilization. The optimal surgical approach and technique for treatment of thoracolumbar burst fractures are still of much debate today. Fig. 12.1 L1 burst fracture with retropulsion of middle column bone into the spinal canal causing canal narrowing. (A) Lateral plain radiograph. (B) CT scan with sagittal reconstruction. (C) Axial CT. (D) T2-weighted sagittal MRI of the thoracolumbar spine.
Thoracolumbar Burst Fractures
![]() Classification
Classification
![]() Workup
Workup
Physical Examination
Spinal Imaging
![]() Treatment
Treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







