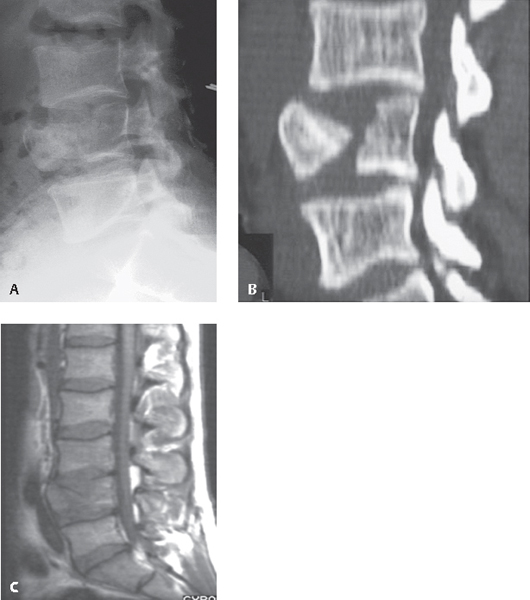
11 Thoracic and lumbar compression fractures are of a bimodal etiology. Most osteoporotic compression fractures result from low-energy injuries, but high-energy trauma sustained in falls from height and vehicular collision contributes a significant quantity of these injuries annually in younger and middle-aged patients. The decrease in bone mineral density seen in osteoporosis is a predisposition to many fractures. These insufficiency fractures occur commonly at the distal radius, hip, and spine, with the majority of vertebral compression fractures occurring in the mid-thoracic to upper lumbar region. With the aging of the baby boomers, with a median age of 65 in 2010, there has been an increased prevalence of vertebral compression fractures in the United States.1 The National Osteoporosis Foundation has estimated that more than 100 million people worldwide are at risk for fragility fractures.2 Many of the fractures that occur within the axial skeleton can be effectively managed with activity modification, bracing, and analgesics. Only a small percentage of patients who cannot be mobilized with these conservative efforts require surgical treatment. Of those with insufficiency fractures treated operatively, most are managed with vertebral augmentation procedures, such as kyphoplasty or vertebroplasty, rather than fusion. In North America, a common classification for thoracolumbar fracture is the Denis system, which divides the axial skeleton into anterior, middle, and posterior columns (Fig. 11.1).3 Utilizing this system, Denis described four injury types: compression fractures, burst fractures, flexion-distraction fractures (e.g., seat belt injuries), and fracture dislocations. Another effective method described by Vaccaro for evaluation of thoracolumbar injury is the Thoracolumbar Injury Classification System (TLICS).4 This system provides treatment recommendations after evaluating fracture morphology, neurologic findings, and the integrity of the posterior osseoligamentous complex. Several studies have validated this system’s usefulness.5 Fig. 11.1 Vertebral body outlining the Denis three-column support structure of the spinal column. The anterior column consists of the anterior half of both the vertebral body and the disks, along with the anterior longitudinal ligament (ALL). The middle column consists of the posterior longitudinal ligament (PLL) and the posterior half of the disk and vertebral body. The posterior column consists of the bony neural arch, posterior spinous ligaments, and ligamentum flavum as well as the facet joints. All vertebral compression fractures involve loading to the anterior spine. They are distinguished from burst fractures, which additionally have posterior vertebral wall involvement and commonly have bone retropulsion into the spinal canal. Vertebral compression fractures are rarely unstable and do not tend to present with spine-related neurologic deficits. Evaluation of the posterior tension band, which is composed of the dorsal osseous and ligamentous structures, is necessary, as high-energy injuries may be unstable despite presenting only as simple anterior vertebral compression fracture injuries on initial radiographs. High-energy, compression-type spinal injuries require an evaluation that determines the stability of the dorsal spinal column. Along with a purposeful physical examination, this may include computed tomography (CT) and magnetic resonance imaging (MRI) studies to evaluate the posterior spinal tension band fully. Patients with low-energy, pathologic fracture etiology should be worked up for neoplasm and osteoporosis and treated accordingly. This may entail additional imaging studies in addition to a CT-guided or other method of spinal biopsy. Initial imaging studies include anteroposterior (AP) and lateral radiographs (Fig. 11.2A). Plain radiographs in the acute trauma setting are often difficult to obtain and interpret because of other injuries and artifact from immobilization backboards, surrounding soft tissues, and bony overlap. CT imaging is a relatively quick and reliable study to determine whether an unstable pattern exists (Fig. 11.2B). Additional information regarding available space in the spinal canal for neural elements can be discerned in those patients with burst fractures that could not be fully appreciated on plain radiography. MRI is perhaps the most clinically useful study in patients with vertebral compression fractures (Fig. 11.2C). Fracture maturity and healing can often be inferred from the amount of bony edema on T2-weighted sequences when vertebral augmentation is considered. Additionally, MRI is useful in determining the extent of both osseous and soft-tissue involvement in both primary and metastatic neoplastic processes if reconstruction is being considered. For patients with high-energy trauma mechanisms, MRI is useful if there is concern for a posterior ligamentous complex disruption. In the atypical case of compression fracture with neurologic deficit, MRI can be useful in determining extent and localization of neural insult along with etiology (for example, fracture-related epidural hematoma versus direct compression of neural elements from retropulsed bone and tissue). In patients who are unable to have MRI scans, a bone scan can be used to determine whether fractures are acute or chronic. Fig. 11.2 (A) Lateral plain radiograph, (B) CT scan with sagittal reconstruction, and (C) T1-weighted sagittal MRI of the lumbar spine demonstrating an L4 vertebral compression fracture. It is a stable fracture as defined by the Denis classification system. Note that there is not posterior extension of the fracture into the spinal canal and no distal spinal cord compression.
Thoracic and Lumbar Vertebral Compression Fractures
![]() Classification
Classification
![]() Workup
Workup
Spinal Imaging
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







