Measured resection technique
Flexion gap balanced technique
Favored by 80 % of surgeons
Favored by 20 % of surgeons
Bone resection independent of ligaments
Bone resection independent of bony landmarks
Several bony landmarks for femoral rotation
Extension gap must be balanced perfectly
Soft-tissue control after bone resection
Ligaments must be sufficient
Bony landmarks are difficult to identify
Limits possible after huge ligamentous release
Femoral rotation parallel to the transepicondylar axis
Rectangular flexion gap
Joint line: femoral recut or downsizing maybe necessary
Joint line: uncontrolled change possible
In addition to these techniques, the kinematically aligned prosthesis [6] represents a further concept in TKR.
The most commonly used references for femoral rotational alignment are:
Surgical transepicondylar axis
Anteroposterior trochlear line
Posterior femoral condyle line
“Grand piano sign”
3.2 Bony Landmarks as Orientation for Rotational Femoral Alignment
3.2.1 Transepicondylar Axis
Two types of transepicondylar axes have been described [7]: the surgical and clinical transepicondylar axis (Fig. 3.1). A line connecting the tip of the lateral epicondyle to the medial epicondylar sulcus is defined as the surgical transepicondylar axis, whereas a line connecting the tip of the lateral epicondyle to the medial epicondylar tip is defined as the clinical transepicondylar axis. The surgical transepicondylar axis is typically used to determine femoral rotation [7]. However, the identification of both axes is difficult during surgery, and no instrument relies directly on these axes. The posterior condylar line is, on average, internally rotated 3° from the surgical transepicondylar axis [8]. Thus, standard instruments use 3° of external rotation from the posterior femoral condyles to set the femoral rotation parallel to the surgical transepicondylar axis. The location of the collateral ligaments can help to determine the medial and lateral epicondyles and to identify the clinical transepicondylar axis [9]. Several authors [7, 10] suggested preoperatively identifying the surgical transepicondylar axis on a special computed tomography (CT) scan [7]. However, studies demonstrated it was difficult to find the medial epicondylar sulcus on axial CT scans and, therefore, difficult to identify the surgical transepicondylar axis [10]. In these cases, 3° of the clinical transepicondylar axis could be subtracted to determine the surgical transepicondylar axis [10]. The surgical transepicondylar axis was shown to be the optimal flexion axis [11]. However, recent studies focused on more kinematic three-dimensional models to describe the optimal femoral rotation [8, 12, 13]. These studies described the kinematic axes (the cylindrical axis [12] and femoral transverse axis [8]), which did not coincide with the surgical transepicondylar axis.
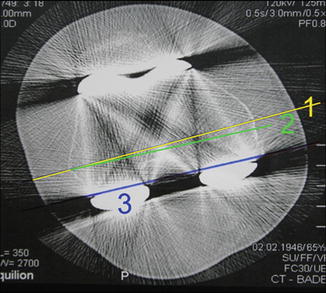
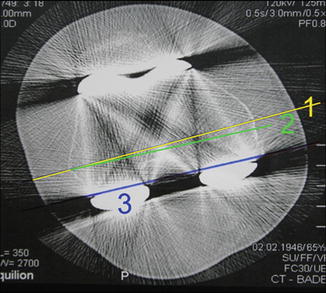
Fig. 3.1
Computed tomography (CT) of the TKR [1]. (1) Clinical transepicondylar axis (medial epicondylar to lateral epicondylar tip). (2) Surgical transepicondylar axis (medial epicondylar sulcus to lateral epicondylar tip). (3) Posterior femoral condyle line
The surgical transepicondylar axis connects the lateral epicondyle and the medial epicondylar sulcus. The posterior condyle axis is 3° internally rotated with regards to the surgical transepicondylar axis.
3.2.2 AP Trochlear Line
Whiteside et al. described the anteroposterior (AP) trochlear line as a reliable landmark for femoral component rotation. This line is defined as a line connecting the deepest point of the trochlea to the center of the notch [2]. In a cadaver study of 30 femora, 5 observers identified the AP trochlear line more accurately than the transepicondylar axis [14]. The AP trochlear line is, on average, rotated 90° from the surgical transepicondylar axis. Thus, both landmarks may be used to double-check during surgery. Several other studies confirmed the AP trochlear line as a reliable landmark for femoral rotation [2, 15, 16]. However, in cases in which severe anterior and posterior deformity is present or in cases with a dysplastic trochlea, the AP line may be difficult to identify. One study demonstrated that the AP trochlear line was less reliable in knees with medial femorotibial osteoarthritis [17].
Whiteside’s line connects the deepest point of the trochlea to the center of the notch and it is perpendicular to the surgical transepicondylar axis.
3.2.3 External Rotation Based on the Posterior Condyles
Several resection instruments use the posterior condylar line plus a few degrees (0–10°) of fixed external rotation to determine femoral rotation. Several authors concluded that the average value of the angle between the surgical transepicondylar axis and the posterior condylar line is −3° in the “standard” osteoarthritic varus knee [8]. However, it is critical to always use +3° external rotation of the femoral cutting guide with respect to the posterior femoral condyles. In up to 30 % of cases, the femoral rotation alignment will not be correct, especially in the valgus deformed knees [18].
3.3 Soft Tissue Landmarks for Femoral Rotational Alignment
3.3.1 Flexion Gap Balanced Technique
In the flexion gap balanced technique, the flexion gap is balanced by laminar spreaders or a tensioning device after ligamentous release in extension [19]. With the knee in flexion, the femoral cutting block is rotated by the ligaments parallel to the 90° proximal tibia cut. Thus, a rectangular flexion gap is created. However, a perfect 90° proximal tibia, a perfectly balanced extension gap, and a perfect 90° distal femoral cut are key for proper femoral rotation and offer several possibilities for failure. Studies have shown there are difficulties in obtaining proper femoral rotation using only the soft tissue as a reference [20–22]. Surgeons who prefer the flexion gap balanced technique may use bony landmarks to verify their femoral rotation.
A variation of the flexion gap balanced technique is the tibial shaft axis method [23]. Here, the tibia shaft axis is used to balance the flexion gap, rather than the soft tissue [23]. Studies have shown a perpendicular relation of the transepicondylar axis to the longitudinal axis of the lower extremity (tibia shaft axis) [23, 24]. Therefore, the tibial shaft axis can be used to determine the femoral rotation and balance the flexion gap [23].
Flexion gap technique: Flexion gap balanced by laminar spreaders or tensioning devices after ligamentous release in extension. In flexion the femoral cutting block is placed parallel to the 90° proximal tibial cut.
3.3.2 The Anterior Surface of the Femur as Landmark for Femoral Component Rotation
The anterior surface of the femur was described as a possible landmark for femoral component rotation [4]. The anterior surface of the femur was cleared and used directly as a platform to determine femoral component rotation [4]. The anterior surface of the femur showed a strong correlation to the anteroposterior (AP) trochlear line (Whiteside’s line) [4]. However, further studies are necessary to confirm this correlation and the practical relevance.
3.3.3 Grand Piano Sign
The external rotation of the femoral component with regard to the posterior condylar line (parallel to the transepicondylar axis) creates a morphological pattern on the anterior resected surface of the femur, known as the grand piano sign [5, 25] (Fig. 3.2). One study showed variance of the grand piano sign was related to this external rotation from the posterior condylar line [5]. However, the grand piano sign cannot be used directly to identify proper femoral rotation, given that the rotational alignment can only be estimated and verified after the anterior femoral cut.
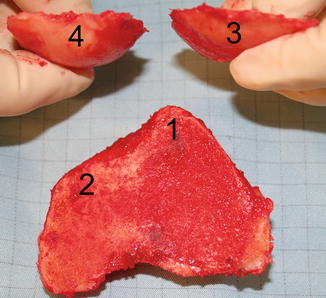
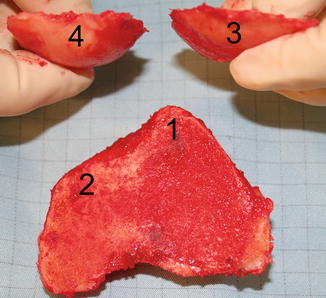
Fig. 3.2
The grand piano sign as an indicator for femoral external rotation with regard to the posterior condylar line. In consequence of the external rotation, the resected anterior surface is lateral (1) more than medial (2). The resected posterior epicondyle is medial (4) larger than lateral (3)
3.4 The Kinematic Alignment in Total Knee Replacement
Recently, the kinematic alignment in TKR was described [6]. The components of the TKR are aligned according to three kinematic axes: (1) an axis about which the tibia flexes and extends, (2) an axis about which the patella flexes and extends, and (3) an axis about which the tibia rotates on the femur [6]. The requirement for a kinematic aligned knee is a non-arthritic knee model. A three-dimensional arthritic knee model of the patient is generated from MRI scans. Computer software is applied to this arthritic knee to create a normal knee model. The normal knee model is then used to restore the normal interrelationship among the three kinematic axes. The authors of this method used patient-specific guides with a single radius TKR [6]. Initial encouraging results of this method are published [6]. However, the concept of kinematic TKR is controversial. Patients undergoing total knee replacement do not have normal knees with normal function and soft tissue. The creation of a normal knee model and the surgical realization may be difficult; the lifetime of a nonmechanical aligned knee prosthesis may be reduced.
3.5 Consequences of Malrotation
3.5.1 Femoral Malrotation
3.5.1.1 Internal Femoral Malrotation
The clinical consequences of internal femoral malrotation were described in several studies over the last decade [1, 26, 27]. Internal malrotation of the femoral component (Fig. 3.3) creates an asymmetric, unbalanced flexion gap [26–28], instability in flexion [29], correlation of the femoral component malrotation with lateral condylar lift-off [30], stiffness and pain on the medial side of the proximal tibial bone [3, 31], and anterior knee pain [32]. One study suggested classifying internal malrotation of the femoral component in three degrees of severity: mild, ≤3°; moderate, 4–6°; and severe, >6° [33].


Fig. 3.3
Femoral internal malrotation (the femoral component is internally rotated to the surgical transepicondylar axis) creates an unbalanced, unstable flexion gap with patellar maltracking
3.5.1.2 External Femoral Malrotation
Several studies described the effects of external malrotation of the femoral component [16, 18, 34]. Similar to internal malrotation, excessive external rotation of the femoral component leads to an asymmetric, unbalanced flexion gap with instability in flexion. However, in contrast to internal rotation, the condylar lift-off is medial [18]. Mild external malrotation of the femoral component seems to be more forgiving compared to mild internal malrotation. Possible explanations may be the greater laxity of the lateral soft tissue structures in flexion and the lateral direction of the patellar tracking.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








